The drug prescribed for chest pain is found to also act as against angina and possibly other cardiac pathologies, as said by the researchers after conducting a study on animals.
A compound, designed to prevent chest pains in heart patients, could act as a drug to treat angina and possibly other cardiac pathologies, according to a study on animals.
Researchers from the Centre de Recherche Pierre Fabre in France have shown that the novel compound F15845 has anti-angina activity and can protect heart cells from damage without the unwanted side effects often experienced with other drugs.As F15845 does not interfere with heart function, like some conventional drugs such as beta blockers, it could be given as part of a combination therapy.
"It's completely different from other anti-angina drugs which directly interact with the function of the heart. So the idea is to do a co-administration with conventional heart drugs such as beta blockers," said lead author of the study, Bruno Le Grand from the Centre de Recherche Pierre Fabre in Castres, France.
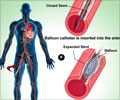
The drug works by blocking excess influxes of sodium into heart cells through 'gate' proteins called sodium channels.
High levels of sodium in heart cells are linked with low oxygen levels, which cause angina and can in turn lead to the build up of toxic concentrations of calcium that are lethal to cells.
While many drugs that target sodium channels can block the influx, but they act universally on heart cells and can sometimes cause further heart irregularities.
Advertisement
These channels also control what is known as the persistent sodium current, which causes a permanent excess sodium influx.
According to the researchers, the drug is absorbed well when given orally and represents a novel therapeutic opportunity for treating angina and possibly other cardiac pathologies.
"We know that in animals, we have acceptable bioavailability, but with the data that we have in human volunteers following phase I clinical trials we are very confident that it is above 70 per cent," said Le Grand.
The study is published in the second issue of the British Journal of Pharmacology.
Source-ANI
PRI/SK