Study says risk of ischemic events high in ACS patients with high residual platelet reactivity

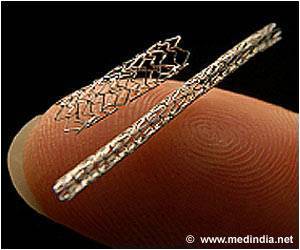
Guido Parodi, M.D., and colleagues of Careggi Hospital, Florence, Italy, conducted a study to examine whether high residual platelet reactivity (HRPR) after clopidogrel loading (a comparatively large dose of the drug given at the beginning of treatment) is an independent prognostic marker of risk of long-term thrombotic events in patients with acute coronary syndromes (ACS) undergoing an invasive procedure and receiving long-term antithrombotic treatment adjusted according to the results of platelet function tests. The study included 1,789 patients with ACS undergoing PCI from April 2005 to April 2009 and who had platelet reactivity assessed via testing. All patients received 325 mg of aspirin and a loading dose of 600 mg of clopidogrel followed by a maintenance dosage of 325 mg/d of aspirin and 75 mg/d of clopidogrel for at least 6 months. Patients with HRPR as assessed by adenosine diphosphate test (70 percent platelet aggregation or greater) received an increased dose of clopidogrel or switched to the antiplatelet drug ticlopidine under adenosine diphosphate test guidance. The primary outcome measure was a composite of cardiac death, heart attack, any urgent coronary revascularization, and stroke at 2-year follow-up. Secondary measured outcomes were stent thrombosis and each component of the primary end point.
The researchers found that the primary end point event rate was 14.6 percent (36/247) in the HRPR group and 8.7 percent (132/1,525) in the low residual platelet reactivity group (LRPR). The difference in the event rate was driven by the difference in cardiac mortality, which was 9.7 percent in the HRPR group and 4.3 percent in the LRPR group. The stent thrombosis rate was 2-fold higher in the HRPR group (6.1 percent [15/247] vs. 2.9 percent [44/1,525]). Additional analysis indicated that HRPR was independently associated with a 49 percent increased risk of the primary end point and a 81 percent increased risk of cardiac mortality.
The authors write that "the results of this study should be considered only as hypothesis generating for further studies of tailored therapy using new antithrombotic agents."
(JAMA. 2011;306[11]:1215-1223. Available pre-embargo to the media at www.jamamedia.org)
Editor's Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Dominick J. Angiolillo, M.D., Ph.D., of the University of Florida College of Medicine-Jacksonville, comments in an accompanying editorial on the use of platelet function testing.
(JAMA. 2011;306[10]:1260-1261. Available pre-embargo to the media at www.jamamedia.org)
Editor's Note: Please see the article for additional information, including financial disclosures, funding and support, etc.
Source-Eurekalert
 MEDINDIA
MEDINDIA



 Email
Email