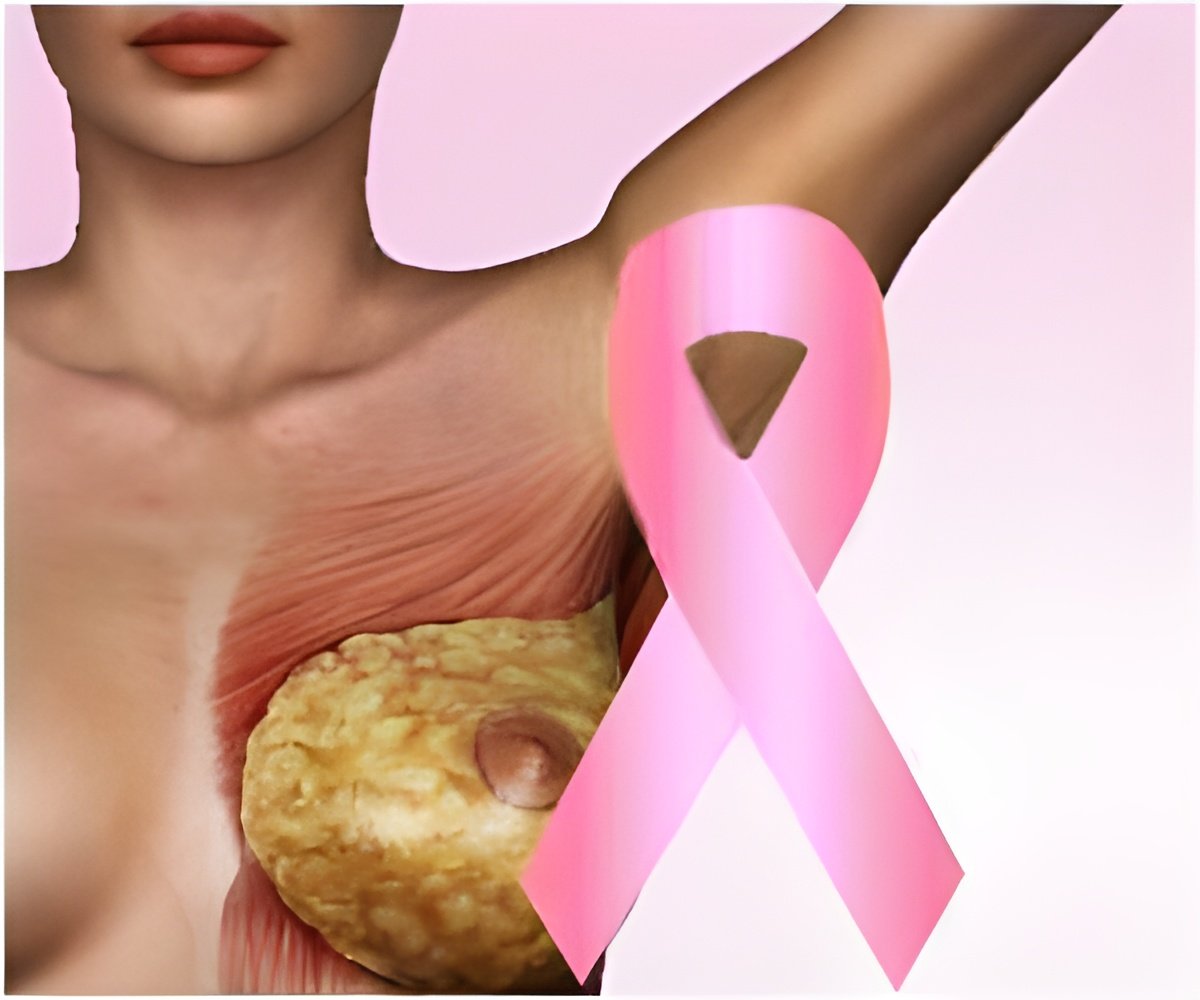
Treatment Approach to Metastatic Hormone Receptor-positive, HER2-negative Breast Cancer
Patients whose breast tumors express the estrogen receptor (ER) and/or the progesterone receptor and do not overexpress the growth factor receptor HER2 are most commonly treated in the first line with a CDK4/6 inhibitor, such as ribociclib, plus a form of endocrine therapy (ET), which blocks the tumor-promoting effects of estrogen. However, some physicians treat tumors with aggressive characteristics, such as visceral crisis, with chemotherapy instead. Those decisions are often made on a case-by-case basis, Lu said.‘Patients with advanced breast cancer treated with ribociclib plus endocrine therapy had fewer adverse events and a significantly longer progression-free survival compared to those treated with combination chemotherapy.’





“Treatment approaches for patients with visceral crises can sometimes be difficult for clinicians, as there is no precise guidance on treatment strategy,” Lu explained. While National Comprehensive Cancer Network (NCCN) guidelines recommend chemotherapy for this patient population, he added that patients with compromised organ function as a result of metastatic spread are often excluded from clinical trials, making it more difficult to determine new treatment regimens for them. They recruited 222 premenopausal or perimenopausal patients with hormone receptor-positive, HER2-negative, aggressive breast cancer, more than 50 percent of whom had visceral crises, as determined by the investigators; 112 were randomly assigned to receive ribociclib plus an aromatase inhibitor—letrozole or anastrozole—and goserelin, which decreases ovarian estrogen production. The other 110 patients were assigned to receive a physicians’-choice combination chemotherapy regimen.
Patients treated with ribociclib plus ET had a progression-free survival of 24 months, nearly one year more than that of patients treated with chemotherapy (12.3 months). The median time to treatment failure was also longer among patients treated with ribociclib plus ET—18.6 months versus 8.5 months among patients treated with chemotherapy.
The overall response rate was similar between the two treatment arms (65.2 percent for ribociclib plus ET and 60 percent for chemotherapy). However, the rates of symptomatic adverse events, such as diarrhea and fatigue, were different: Serious, treatment-related adverse events emerged in 1.8 percent of patients receiving ribociclib plus ET and in 8 percent of patients receiving combination chemotherapy. Similarly, 7.1 percent of patients treated with ribociclib plus ET and 23 percent of patients treated with chemotherapy discontinued at least one component of study treatment due to treatment-related adverse events.
“To be able to extend lives, treatment compliance is key,” Lu said. “A treatment with improved tolerability will definitely enhance compliance and thus increase the chances of longer disease control.
Advertisement
Lu hopes that forthcoming subgroup analyses will reveal clinical characteristics that may help physicians predict which patients will respond best to ribociclib plus ET versus those who may respond better to chemotherapy.
Advertisement
Funding for this study was provided by Novartis Pharma AG. Lu has received personal funding from Novartis, Roche, Merck Sharp & Dohme, Pfizer, AstraZeneca, Eisai, Eli Lilly, and Daiichi Sankyo.
Source-Eurekalert















