COVID-19 in pregnant women increases their risk of death by seven times and has been linked to severe illness in newborns
- COVID-19 increases the risk of women's fatalities by seven times and is also linked to severe diseases in neonates
- A diagnosis of COVID-19 at any stage during pregnancy increased the woman's risk for all critical COVID-19 indications, including ICU (Intensive Care Unit) admission, ventilation, and pneumonia
- Infants born to infected mothers were more likely to be admitted to the NICU (Neonatal Intensive Care Unit), to be born prematurely, or to be born with a low birth weight
Adverse maternal, fetal, and newborn outcomes among pregnant women with SARS-CoV-2 infection: an individual participant data meta-analysis
Go to source).
COVID-19 and Pregnancy
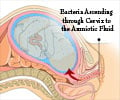
Pregnancy causes physiological, immunomodulatory, and mechanical changes that make women more susceptible to certain disorders, such as COVID-19, and their severe consequences. According to one meta-analysis of 47 studies, this patient population is at a higher risk of death, intensive care unit (ICU) admission, preterm delivery, stillbirth, and neonatal care unit admission than pregnant women who do not have COVID-19. Another recent study discovered that women who were diagnosed with COVID-19 at the time of the birth of their child were more likely to require prolonged hospitalization that included critical care for both mother and child. Despite these findings, researchers are unable to integrate available information on the impact of COVID-19 during pregnancy due to significant differences in outcome definitions, population-specific baseline risks, and methodologies used to diagnose COVID-19. Furthermore, pregnant women in low-income nations have received little attention.Research Data
The current investigation includes pooling data from independent studies utilizing harmonized data definitions and a meta-analytical methodology for individual participant data (IPD). Registries, single- and multi-site cohorts, and case-control studies involving pregnant women with suspected or confirmed COVID-19 were all eligible. Notably, a COVID-19 diagnosis was verified using a polymerase chain reaction (PCR) assay, antigen tests, serology testing after a known exposure, or according to the World Health Organization's suspected case classification (WHO).The researchers detected any potential outliers and inconsistent values for critical data points such as gestational age at birth, mother's age, and neonatal birth weight to assure the integrity of IPD for the study. The research looked at four types of patient outcomes: maternal mortality and morbidity, fetal and neonatal mortality and morbidity, poor birth outcomes, and severe COVID-19 outcomes.
The final analysis included a total of 12 investigations carried out between February 2020 and July 2021. Ghana, China-Hong Kong, Italy, Kenya, Nigeria, South Africa, Spain, Sweden, the Democratic Republic of the Congo, Turkey, Uganda, and the United States participated in these investigations. As a result, 1,942 pregnant women with COVID-19 and 11,194 pregnant women who were negative for COVID-19 were included.
COVID-19 Raises the Likelihood of Maternal Morbidity and Mortality
A diagnosis of COVID-19 at any stage during pregnancy enhanced the woman's risk for all crucial COVID-19 indications when compared to pregnant women who were negative for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). ICU admission, any type of ventilation, and clinician-diagnosed pneumonia were among the worst COVID-19 side effects.COVID-19, in particular, raised a pregnant woman's absolute risk of ICU admission and critical care needs by 3% and 4%, respectively. Pregnant women with COVID-19 were five times more likely to require critical care than SARS-CoV-2-negative pregnant women.
These negative consequences were more common in pregnant women with symptomatic COVID-19. Furthermore, pregnant women with symptomatic infections had a considerably increased risk of maternal death.
COVID-19 enhanced the risk of maternal death in the three included studies that reported deaths during the research period. Pregnant women with COVID-19 had a higher risk of pre-eclampsia, thromboembolic illness, and hypertensive disorders of pregnancy. Pregnant women with COVID-19 had a slightly greater risk of cesarean section. There was no discernible difference in the risk of premature labor, hemorrhage, placental abruption, eclampsia, or intrapartum cesarean delivery.
COVID-19 Worsens Neonatal Outcomes
Infants born to moms who have COVID-19 have an elevated risk of neonatal ICU (NICU) admission. These findings are consistent with previous research, such as the INTERCOVID trial, which found a higher risk of premature birth in SARS-CoV-2-infected women. In addition, infants born to infected women were more likely to be born prematurely or moderately prematurely, as well as with low birth weight.To conclude, although a COVID-19 diagnosis raised the chance of a variety of maternal morbidity and mortality markers, as well as a variety of newborn outcomes, symptomatic infections were an even larger risk factor for these negative impacts. These findings highlight the significance of sustained monitoring among pregnant women to prevent SARS-CoV-2 infection through vaccination and non-pharmaceutical measures such as masks and social distancing.
Reference :
- Adverse maternal, fetal, and newborn outcomes among pregnant women with SARS-CoV-2 infection: an individual participant data meta-analysis - ( https://gh.bmj.com/content/8/1/e009495)
Source-Medindia