Lowering the dosage of estrogen and progesterone may give insights into optimal formulations of hormonal contraceptives and the schedule of therapy for menstrual problems.

‘New model for hormonal control of the menstrual cycle may minimize total exogenous estrogen and/or progesterone dose, and determine the timing of administration that led to contraception.’





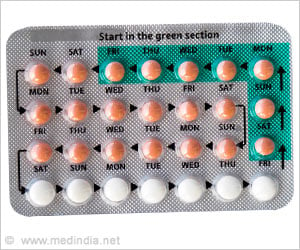
Independent of the administration method, almost all hormonal contraceptives including exogenous progesterone and/or estrogen act by blocking ovulation, changing the cervical mucus, which hinders sperm transport, and/or modifying endometrium which prevents implantation.While optimal control theory for hormonal contraceptives has not been used to simulate contraception, the theory has a long tradition in biology to find strategies that optimize an outcome.
New Model Suggests Lowering Hormone Doses in Contraceptives is Effective
In a new study, the computational model is modified to include mechanisms depicting the contraceptive effect of exogenous progesterone on the menstrual cycle. This new model shows the principal mechanisms behind the transition to contraception.It is calibrated to the patient data extracted and predicts the daily levels of pituitary hormones LH and FSH, and ovarian hormones averaged during a normal menstrual cycle in 23 women. The model output also predicts a reduction in pituitary and ovarian hormone levels caused by exogenous estrogen and/or progesterone.
The model provided evidence that it is possible to reduce the total dose by 92% in estrogen-only contraceptives, or the total dose by 43% in progesterone-only contraceptives, and still prevent ovulation. By combining estrogen and progesterone, the doses of each hormone could be reduced even further.
In addition, the model showed the importance of timing the hormones during the cycle, pointing toward ways that exogenous estrogen and progesterone could be given during only certain phases of the menstrual cycle rather than at steady constant doses. These results may give clinicians insights into optimal dosing formulations and schedules of therapy that can suppress ovulation.
Advertisement
Source-Eurekalert