Improved outcomes of newer drug in some patients could be due to a more complete reversal of the effects of muscle relaxants used during surgery.

‘muscle paralysis drugs work sort of like earplugs on nerve endings. If acetylcholine is a loud noise in this analogy, neostigmine increases how much acetylcholine is available to amplify the signal, similar to yelling louder to be heard through the earplugs.’





What many people don’t realize is that without anesthesia and operating room ventilators, the millions of surgeries normally performed each year in the U.S. would be impossible. Being "put under" anesthesia is accomplished with a cocktail of drugs used to render a patient unconscious and pain free with their muscles relaxed, enabling safe surgeries.
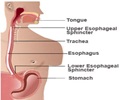
As minimally invasive techniques such as laparoscopic surgery have gained widespread use, keeping a patient’s muscles relaxed and preventing movement during surgery has become increasingly important. A breathing machine, known as a ventilator, is used to help the surgical patient breathe during anesthesia while their muscles are relaxed.
For decades, surgical anesthesia has relied on the drug neostigmine, considered an essential medicine by the World Health Organization, to reverse this muscle relaxation when waking a patient following a procedure. However, researchers have suspected that some of the more serious post-surgical complications, such as pneumonia and respiratory failure, are the result of residual effects of the muscle relaxants.
"For example, pneumonia may be related to the inability to take a deep breath or cough due to residual muscle weakness," says Sachin Kheterpal, M.D. MBA, professor of anesthesiology at U-M Medical School. Five percent of patients undergoing major non-cardiac inpatient surgery have major pulmonary complications, resulting in $100,000 in additional medical costs per patient, he notes.
Advertisement
They found the newer drug was associated with significantly reduced rates of these complications.
Advertisement
To put it another way, says Kheterpal, "muscle paralysis drugs work sort of like earplugs on nerve endings. If acetylcholine is a loud noise in this analogy, neostigmine increases how much acetylcholine is available to amplify the signal, similar to yelling louder to be heard through the earplugs." Sugammadex, on the other hand, "takes the molecule of rocuronium out of the muscle receptor, removing the earplugs." As a result, he says, there are fewer side effects throughout the body and a more complete reversal of the muscle relaxant effect.
For the observational study, the team compared the medical records of 22,856 patients receiving sugammadex to 22,856 patients receiving neostigmine in 12 hospitals in the U.S. The data for the study came from the Multicenter Perioperative Outcomes Group, a national consortium of more than 50 hospitals across 30 states, which Kheterpal and Michigan Medicine lead.
Bridion, which is the brand name for the drug sugammadex, is currently more expensive than neostigmine and typically reserved for sicker patients or patients who may have risks associated with increased acetylcholine.
To account for the effect of the different patient populations, the team matched people who were the same age, had the same medical conditions, and who were having the same type of surgery before and after sugammadex became available in 2017.
"When we looked at documentation of respiratory failure or pneumonia, we saw a 37% decrease across all pulmonary complications and 55 percent decrease in respiratory failure," says Kheterpal. "This is a dramatic decrease in rates of complications."
He notes that some of the limitations of the study include the fact that it was not a randomized controlled trial and it didn’t include many young healthy patients or certain types of surgeries, such as emergency surgery.
"The decision for each patient has to be left up to the providers. But in many practices, neostigmine is no longer used in high risk patients or procedures," he says.
Source-Eurekalert