A new technology developed by scientists helped revealed how the blood cancer cells responded to different anti-cancer medicines, even suggesting potential new treatment combinations.

‘The mass cytometry protocol when applied to current clinical trials helps better understand why some cancers are resistant to anti-cancer therapies, and to match these patients to other, potentially more effective, treatments.’





The research team hope that the new technique could be integrated into clinical trials both to understand why some patients are resistant to anti-cancer therapies, and to predict suitable 'biomarkers' for matching patients with the most effective therapies for their disease. The study was led by Walter and Eliza Hall Institute researchers Dr Charis Teh and Associate Professor Daniel Gray, in collaboration with Professor Garry Nolan and Dr Melissa Ko from Stanford University, US.
At a glance
A new technique called mass cytometry, or CyTOF, is providing new insights into a range of key proteins in blood cancer cells.
By studying the blood cancer myeloma, researchers were able to understand why some cells were not killed by standard anti-cancer drugs, and to devise a more effective therapy.
Advertisement
Cancers are made up of millions of individual cells which are all similar, but not exactly the same. Until recently almost all studies of cancers looked at the cells grouped together, missing any potential differences between individual cells, said Dr Teh.
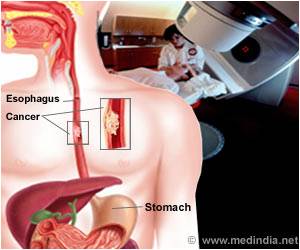
"Excitingly, there are already drugs in clinical trials that inhibit MCL-1 - and when we tested these against myeloma cells, we found the MCL-1 inhibitor made the cells more sensitive to dexamethasone. This was even the case in myeloma samples taken from a patient - our system had identified a potential new therapeutic approach for myeloma," Dr Teh said.
A new approach
Mass cytometry may even have a role in providing real-time detailed analysis of patient samples from clinical trials, Associate Professor Gray said.
"The panel of markers developed in this study gives researchers considerable scope to understand how cancer cells are responding to anti-cancer therapies - and as we found, it can even help to identify better drug combinations," he said.
"Adding mass cytometry to the analysis of clinical studies could reveal why some patients respond to therapies differently from others, and how resistance to anti-cancer medicines can develop in a small fraction of cancer cells.
"Mass cytometry could also identify a small number of proteins that can be used as specific 'biomarkers' that can predict a patient's response to therapy, and be used to match that patient with the most effective treatments. We've already started collaborations with our clinical colleagues to investigate this possibility further," Associate Professor Gray said. The research was published in the journal Cell Death & Differentiation.
The research was supported by the Australian National Health and Medical Research Council, a Fulbright Australia-America Postdoctoral Fellowship, Royal Australasian College of Physicians, Leukaemia Foundation of Australia, Cancer Council Victoria, US Leukemia and Lymphoma Society, US National Institutes of Health and the Victorian Government.
Source-Eurekalert