A recent study demonstrates the use of novel data mining approach to find a correlation between proton pump inhibitors exposure and risk of myocardial infarction in general population.

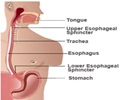
Some studies have shown that PPIs reduce the efficacy of the antiplatelet agent clopidogrel in patients with a history of acute coronary syndrome (ACS), which is typically prescribed for the risk reduction of subsequent ischemic events. One of the mechanisms in which PPIs cause increase in major adverse cardiovascular events (MACE) in patients with ACS is by inhibiting the clopidogrel-activating liver isoenzyme, CYP2C19. Thus, PPIs interfere with the anti-clotting capacity of clopidogrel, thereby potentially increasing the risk for coronary thrombosis and myocardial infarction.
Past research suggests the association of cardiovascular risk with the use of PPIs including in patients who are not taking antiplatelet agents as well as those without any vascular disease. Hence, a systematic study was undertaken to explore the association of PPIs and cardiovascular risk in general US population by using a novel and recently validated data-mining approach for pharmacovigilance. The study authors analyzed multiple electronic medical record datasets as well as examined a prospectively followed clinical cohort.
Two sources were used for the data mining analysis, out of which the primary source was from Stanford and a secondary source from Practice Fusion, as well as one prospective source for data analysis. The authors also examined the relation between PPI use at enrollment and cardiovascular mortality in GenePAD (the Genetic Determinants of Peripheral Arterial Disease) study.
Presence of GERD was used to define baseline population who were divided into two study groups. The primary study group consisted of patients taking PPIs, which included a subgroup of patients on clopidogrel. The second group had patients who were on H2 blockers or H2B (such as cimetidine, famotidine, nizatidine, and ranitidine) for the treatment of GERD. Controls were selected from the baseline population using propensity score matching.
The researchers studied over 16 million clinical documents on 2.9 million individuals to examine whether PPI usage was linked with cardiovascular risk in the general population.
Patients using PPIs were found to have a 1.16 fold increased association (95% CI 1.09–1.24) with MI. Results of survival analysis in the prospective cohort demonstrated a two-fold (HR = 2.00; 95% CI 1.07–3.78; P = 0.031) increase in cardiovascular mortality event. The study also did not find any correlation between MI and patients treated with H2 blockers for GERD in the same dataset.
One of the major limitations of the study was that it wasn’t able to take into account factors such as obesity and insulin resistance. There was also a possibility that PPIs were prescribed for angina, which was misdiagnosed as acid reflux.
The findings of the study along with the preclinical results show a need for further investigation.
Source-Medindia
 MEDINDIA
MEDINDIA



 Email
Email