- Polymyalgia Rheumatica - (http://www.rheumatology.org/i-am-a/patient-caregiver/diseases-conditions/polymyalgia-rheumatica)
- Definition - Polymyalgia rheumatica - (http://www.mayoclinic.org/diseases-conditions/polymyalgia-rheumatica/basics/definition/con-20023162)
- About Polymyalgia rheumatica (PMR) - (http://www.arthritisresearchuk.org/arthritis-information/conditions/polymyalgia-rheumatica.aspx)
- What is Polymyalgia Rheumatica? - (http://www.arthritis.org/about-arthritis/types/polymyalgia-rheumatica/)
- Polymyalgia rheumatica and the risk of cerebrovascular accident. - (https://www.ncbi.nlm.nih.gov/pubmed/27625228)
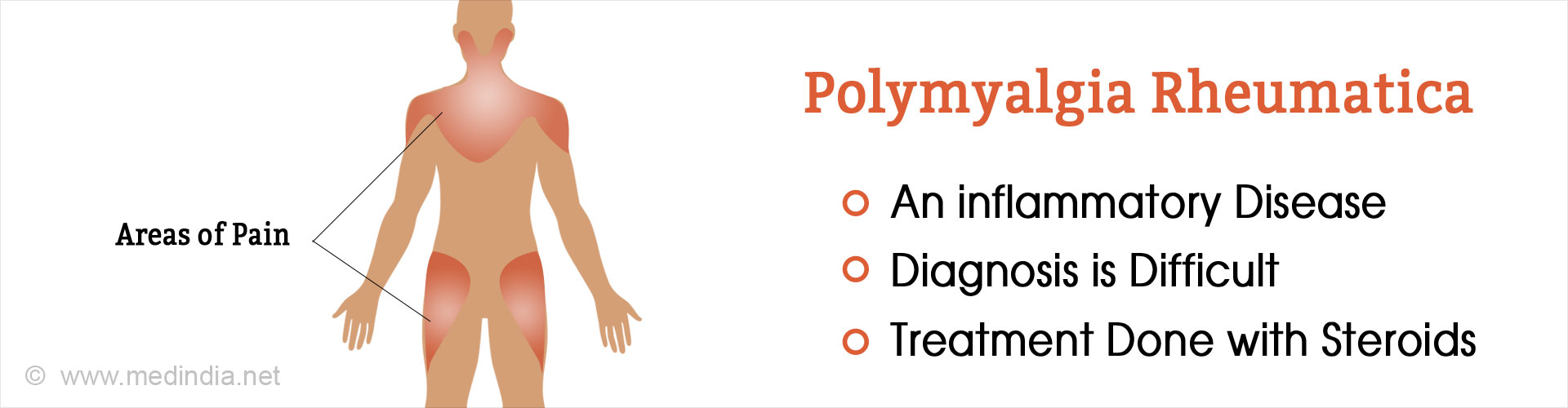
What is Polymyalgia Rheumatica?
Polymyalgia rheumatica (PMR) is an inflammatory disorder that causes severe muscle pain, muscle stiffness, muscle spasms and cramping on both sides of the body, particularly in the shoulders, neck, arms, thighs, and hips. It generally occurs in the elderly above 60 years of age, with women being affected more than men. The term “myalgia” is derived from the Greek word for “muscle pain” and since this occurs at various parts of the body, it is called “polymyalgia”. Additionally, since its symptoms resemble that of rheumatoid arthritis (inflammation, pain in the joints, muscles and fibrous tissues), the term “rheumatica” is used. Hence, the name “polymyalgia rheumatica”.
PMR can be associated with giant cell arteritis (GCA) (also called temporal arteritis) and the two disorders can be regarded as different manifestations of a shared disease process. This is supported by the fact that both PMR and GCA are associated with specific alleles on human leukocyte antigen (HLA)-DR4 and familial aggregation. It is interesting to note that approximately 15% of PMR patients develop GCA, while up to 50% of GCA patients can develop PMR.
What are the Causes of Polymyalgia Rheumatica?
The exact cause of PMR is uncertain. However, scientific evidence indicates that it could arise because of the interplay between several factors, which are highlighted below:
- Autoimmunity: An autoimmune process has been implicated in the pathogenesis of PMR wherein a person’s own immune cells attack his or her connective tissues and joints leading to disease.
- Genetic Predisposition: There is evidence to indicate that inherited factors could lead to increased susceptibility to PMR. Individuals having HLA-DR4 haplotype have been observed to be at greater risk for PMR. Importantly, people of Northern European and Scandinavian ancestry are at a greater risk for PMR.
- Viral Infections: Seasonal viral infections have been implicated in PMR. The sudden onset of symptoms with periodic abatement seen in PMR patients can be explained by cyclic replication patterns exhibited by viruses. Importantly certain viruses such as adenovirus, human parainfluenza virus and parvovirus B19 have been implicated in triggering PMR.
What are the Signs and Symptoms of Polymyalgia Rheumatica?
The cardinal symptoms of PMR are
- Muscle stiffness and spasms or cramps
- Muscle or joint pain
The pain may be so intense that it may hamper sleep. The symptoms may appear slowly or suddenly, usually occurring in the morning and slowly easing as the day progresses. The symptoms can become worse if the patient remains inactive or bed-ridden. The affected areas include the shoulder, neck, upper arms, thighs, buttocks, and hips.
It is noteworthy that the forearms, hands, legs and feet remain unaffected. PMR can also occur in conjunction with GCA or temporal arteritis, a dangerous condition which may result in stroke. It is characterized by swelling of the arteries of the temples, headache, scalp tenderness, vision changes or a painful jaw while chewing. The patient may also exhibit the following symptoms:
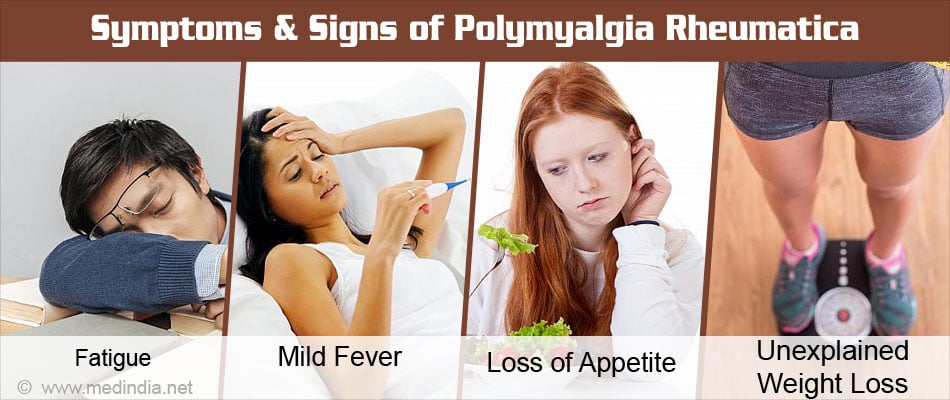
- Severe weakness, fatigue, and exhaustion
- Mild fever with an irregular pattern
- Loss of appetite
- Anxiety and depression
- Unexplained weight loss
- Mild anemia
- A general feeling of being unwell or malaise
- Loss of function of affected parts with limited mobility
How do you Diagnose Polymyalgia Rheumatica?
PMR usually occurs after the age of 60 years, but the average time before a definitive diagnosis can be made may take another 10 years. The symptoms of PMR such as inflammation can overlap with many other conditions such as rheumatoid arthritis osteoarthritis, fibromyalgia, and polymyositis. It is generally diagnosed by the following procedures:
- Detailed history and physical examination – to rule out other causes
- Blood tests - These include the measurement of erythrocyte sedimentation rate (ESR), a complete blood count (CBC), or estimation of C-reactive protein (CRP), which are indicators of infection and inflammation. Other blood tests may include the following:
- Rheumatoid factor (RF)
- Antinuclear antibody (ANA)
- Anticyclic citrullinated peptide (Anti-CCP)
Importantly, none of these blood tests are definitive for PMR. There are however, certain diagnostic criteria laid down to diagnose PMR.
PMR – Diagnostic Criteria
Several diagnostic criteria have been put forth to diagnose PMR though none of them have been universally accepted. These include
Any 3 factors listed below, or just one factor and a temporal artery biopsy positive for giant cell arteritis
- Age over 65 years
- Bilateral shoulder girdle pain
- Symptom onset <2 weeks
- ESR >40 mm/hour
- Depression/weight loss
- More than 1 hour morning stiffness
- Upper arm tenderness, bilateral
How do you Treat Polymyalgia Rheumatica?
The basic rationale of treatment is to manage inflammation and pain. The under-mentioned strategies are generally employed:
Corticosteroid Therapy
PMR is usually treated with corticosteroids such as prednisolone at low doses, starting with a dose of 10-20 mg daily. The medication should give relief from pain and muscle stiffness within 2-3 days; if not, the diagnosis should be reconsidered. After 2-4 weeks, the dose is slowly decreased with the aim of maintaining it at the lowest possible dose without triggering a relapse. Corticosteroid therapy usually lasts for about 2 years and the patient should be monitored for adverse effects of long-term steroid treatment.

Pain Killers and NSAIDs
Pain killers and non-steroidal anti-inflammatory drugs (NSAIDs) such as paracetamol, nimesulide, aceclofenac, diclofenac, and chlorzoxazone are usually employed to manage the pain and inflammation, as an adjunct to corticosteroid therapy. It should however be noted that NSAIDs such as ibuprofen and naproxen are usually ineffective for treating PMR.
Calcium and Vitamin D Supplementation
Since corticosteroids can cause osteoporosis, it is sometimes advised to take regular calcium and vitamin D supplementation to prevent bone loss. The recommended daily dose of calcium is 1000-1500 mg, while that for vitamin D is 800-1000 IU.
Disease-modifying anti-rheumatic drugs (DMARDs)
If the condition does not improve with corticosteroids or there are frequent relapses, a special category of drugs called DMARDs are prescribed along with the corticosteroids. Two common drugs belonging to this category include methotrexate and leflunomide. These are immunosuppressants that dampen the activity of the immune system so that the inflammation is reduced. This helps to lower the dose of the corticosteroids without the risk of flare-ups.
How do you Prevent Polymyalgia Rheumatica?
Prevention of PMR is difficult because if there is a family history of PMR or similar conditions, there will be a greater genetic propensity to develop the disease in old age. However, leading an active lifestyle, with a proper balanced diet and regular exercise will help to keep the disease at bay. Moreover, abstinence from smoking and alcohol consumption will lower the risk of PMR appreciably. Consumption of diets rich in calcium and vitamin D will be beneficial. Regular health check-ups for blood pressure, lipids, blood sugar and cataracts will also help avoid the disease.
Health Tips
- Lead an active lifestyle: Before you are affected with PMR, try to maintain an active lifestyle to keep your energy levels high and your heart and musculoskeletal system functioning properly.
- Do light exercises daily: Regular exercise is important for maintaining joint flexibility and optimal muscle and bone health. Good forms of light exercises include walking, cycling on a stationary bicycle, and yoga.

- Eat healthy: Healthy eating habits is a key to aging gracefully. A healthy diet will ensure a strong and robust immune system. Eat plenty of green vegetables, seasonal fruits, whole grains, poultry, fish and dairy products. But cut down on carbohydrates and fats. Since, PMR medication (corticosteroids) can cause high blood pressure, it is wise to cut down on table salt too.
- Maintain mobility: If you are already affected with PMR, try to keep your joints as flexible as possible and functioning properly. Move about around the house and avoid inactivity. But you should also use assistive devices to minimize the risk of falling.
- Take medications daily as prescribed: It is most important to take your medications daily as prescribed by your doctor. Be in touch with your doctor so that he may adjust the doses as and when required.
- Rest adequately: Rest and sleep are important for recuperation. Light exercise and adequate rest will help to maintain optimal health.