- J Dig Dis. 2009 Feb;10(1):1-6
Inflammatory bowel disease: A survey of the epidemiology in Asia.
Goh K, Xiao SD. University of Malaya, Kuala Lumpur, Malaysia - Am J Gastroenterol. 2009 Feb 24. [Epub ahead of print]
Differentiating Intestinal Tuberculosis From Crohn's Disease: A Diagnostic Challenge. - Expert Opin Ther Targets. 2009 Feb;13(2):259-63.
Inflammatory bowel diseases: highlights from the United European Gastroenterology Week 2008.
Kaser A, Tilg H.
About
Crohn’s disease and Ulcerative Colitis are categorized as Inflammatory Bowel Disease.
Crohn’s disease also known as regional enteritis or granulomatous enteritis is an inflammation of the small intestine. Along with ulcerative colitis it is grouped under the category of inflammatory bowel disease. The two diseases have some differences but have much in common between them.
Both are characterized by bouts of abdominal pain, diarrhea and bleeding from the rectum. The disease usually subsides on its own or with treatment only to recur after some weeks or months (remissions and relapses). The disease also reveals itself outside the intestines in the form of back pain, uveiitis (red eye), and skin nodules.
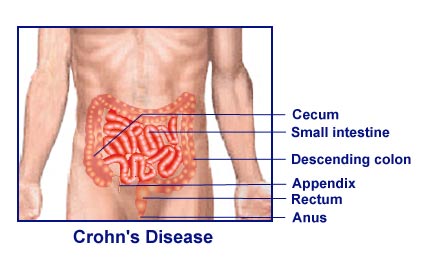
Regional enteritis, as the name suggests, involves the terminal ileum and at times a portion of the large intestine. It may however occur anywhere along the gastro-intestinal tract from the mouth (causing mouth ulcers) to the rectum where it reveals its presence in the form of peri-anal fistulas, anal abscesses and so on.
What causes Crohn’s disease? As in ulcerative colitis, the cause of the disease is suspected to be a deranged immune system that overshoots the inflammatory response to an unknown causative agent. The tendency to develop Crohn’s disease may be inherited as it is known to occur in close relatives. Sometimes a particular type of food may trigger the attack, but there is no singularly identified causative factor in the diet or otherwise that has been implicated in this problem.
The term ‘granulomatous enteritis’ enlightens us about the pathological feature of this illness. Initially small ulcers of the lining mucosa occur, which extend deeper and form granulomas. These granulomas have to be differentiated from intestinal tuberculosis, particularly in endemic areas, where TB is common. As the disease process progresses, it forms strictures or narrowing of the intestine leading to obstruction and even perforation of the bowel. Abnormal connections or fistulae between affected portions of the intestines and adjacent structures like urinary bladder, vagina and peri-anal skin also may occur.
There is no cure for regional enteritis and treatment is aimed at relieving the symptoms and controlling the inflammation. Crohn’s disease medications include anti inflammatory agents like salazopyrine, steroids. Immuno-modulators like Azathioprine, Infliximab and the newest Adalimumab are used in those patients not responding to steroids or suffering from undesirable side-effects of steroids. Methotrexate, another immuno-modulator has also joined the fray of new Crohn’s disease treatments.
Long-standing disease leaves the patient malnourished and anemic, and treatment has to be directed towards maintaining nutrition by tube-feeds, if necessary and improving the hemoglobin. Certain diets are known to trigger an attack, but it varies from one individual to the other. Probiotics are also touted to prevent relapses.
Going under the knife is an option for complications such as fistula formation, perforation, intestinal obstruction and also if the chronic disease is not responding to medication. The diseased portion is resected and joined to the adjacent non-affected portion. Recurrences after surgery can also occur, although it may take a while.