- Kidney - (https://en.wikipedia.org/wiki/Kidney)
What do the Kidneys do?
The kidneys work as a filtering unit for the blood in our bodies and help in excreting waste products from the blood stream. The kidney filters out waste products from the blood stream. Approximately 200 litres of blood are filtered through the kidneys daily but the body passes only about 2 liters of urine.
Usually, there are two kidneys in each one of us. They are bean shaped and weigh between 125 and 170 grams (adults males) and 115 and 155 grams (adult females) and are 12 cm x 5 cms in size. They are located in the middle of the back, just below the rib cage. Each kidney is made up of small, complex filtering units called nephrons. Each kidney contains about one million nephrons. The nephrons work continuously to filter out waste products from the blood stream, which come from the food that one eats and the fluid that one drinks and from the normal metabolic activities of the body. The kidney also regulates the concentration of most of the constituents of body fluids.
They also retain certain substances that are needed by the body. In addition, the kidneys stimulate the body to produce red blood cells, regulate blood pressure, keep bones healthy by converting inactive vitamin D to its active form and maintain the water and pH (acidity / alkalinity) balance of the body.
What are the Symptoms of Kidney Disease?
Kidneys maybe damaged due to a sudden disease process resulting in acute kidney injury (AKI) or due to a slow progressive pathology resulting in chronic kidney disease (CKD) which, in its severest form is called end stage renal disease (ESRD). In either spectrum of injury the end result is the same. The waste products that are otherwise normally excreted in the kidney accumulate within the body and lead to different symptoms
This could result in a variety of symptoms like nausea, vomiting or loss of appetite that depend in part on the type of disease process that led to the renal injury. The patient could also feel weak and irritable. Often there is a decrease in urine output called oliguria or anuria (non-passage of urine) and this in turn results in fluid retention in the limbs or generally throughout the body called edema. The blood pressure can be raised (hypertension) and decreased production of red blood cells can lead to lowering of hemoglobin (anemia).
On testing blood and urine samples, the following changes may be seen:
- Increased Uremic Toxin Levels - The term uremic toxins refer to a wide variety of chemical substances that are normally excreted in the urine but accumulate in the body in kidney disease condition. Of these, the most commonly measured chemicals are urea and creatinine. Both of these substances are increased from normal levels in kidney disease.
- Albuminuria or Proteinuria - Albumin, a vital protein component is lost in the urine especially in diseases that damage the glomerulus (the main filter of the nephron)
- Hypoalbuminemia - Decreased amount of protein in the blood.
- Hyperlipidemia - Excess amount of fats in the blood.
- anemia - Decrease in the number of red blood corpuscles (RBCs).
- Hypocalcemia - Decreased level of calcium in the blood.
- Hyperkalemia - Increase in the level of potassium in the blood.
Kidney Disease:
The two most common causes of kidney disease are uncontrolled diabetes and high blood pressure. Pathologies of the glomeruli within the nephrons of the kidney called glomerulonephritis or infection of the kidney called pyelonephritis can also lead to kidney failure.
The kidney diseases of interest are briefly mentioned.
Diabetes & Kidney Disease
There are two types of diabetes mellitus. One is dependent on insulin and other is not dependent on insulin
Approximately 20-30% of all diabetics can get affected with diabetic nephropathy which is slowly progressive and at some stage will lead to kidney failure. Diabetic kidney disease is the most common cause of end stage renal failure worldwide. And early screening and aggressive management of diabetes can vastly decrease the burden of the disease. The incidence of kidney
Acute & Chronic Glomerulonephritis:
This is due to pathologies of the "glomerulus". Most kidney diseases attack the nephron causing them to loose their filtering capacity. This usually is a slow, gradual process and can sometimes take many years. Sometimes it can also happen in a short span of time. Glomeruli form the sieve part of the nephrons. Depending on the extent of the inflammation either the glomerulus can recover completely or partially or not at all. This inflammation usually can occur three to four weeks after an attack of sore throat or tonsillitis. If they are destroyed by this inflammation, kidney failure sets in. Usually an acute glomerulonephritis recovers in 2-3 weeks.
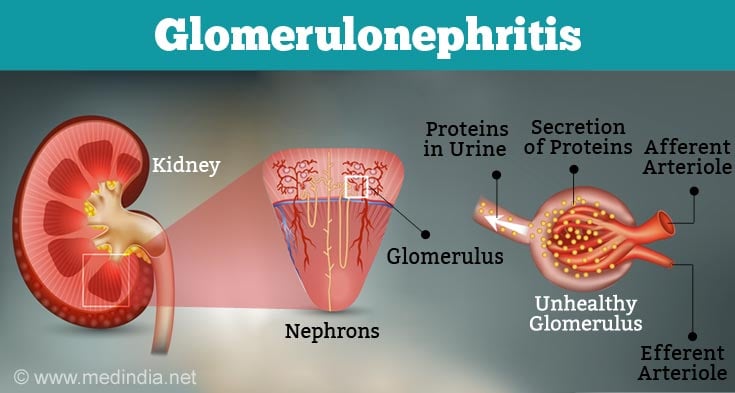
Acute glomerulonephritis can lead to long-term changes. If the glomeruli are damaged, they slowly become completely burnt out over months or years. This irrecoverable damage is called "chronic .
Nephrotic Syndrome versus Nephritis
A syndrome is a combination of signs and symptoms characteristic of a specific condition
Normally less than 150 mg of protein is lost in the urine per day whereas in Nephrotic syndrome more than 3 grams of protein can be lost in the urine every day. As a result, the level of protein in the blood falls and this produces swelling of the face and body due to retention of water or fluid. Nephrotic syndrome can happen if there is associated inflammation of kidney (glomerulonephritis). A variety of different diseases can trigger pathological processes within the glomeruli and result in nephrotic syndrome The glomerulus normally has a 'sieve' like structure and when blood passes through the glomerulus the water and minerals escape through this sieve. The sizes of holes in the sieve are very small and through this the larger protein molecules do not escape. In some types of glomerulonephritis the size of these holes increases leading to loss of protein or album in the urine. Diseases presenting with the nephrotic syndrome are usually not associated with a decrease in urine output, at least initially.
Nephritis is a term used to describe a variety of diseases of the glomerulus where the severity of the pathological process results in the loss of not only the protein in the urine but also blood and is often associated with decreased urine output and hypertension.
Pyelonephritis:
E. coli is the commonest organism causing urinary tract infection (UTI). The infection affects the kidney and the renal tubules are destroyed. Over years, the urine's concentrating capacity can be lost. This leads to dehydration and salt loss and eventually leading to kidney failure.
Polycystic Kidney Disease:
This is a fairly common condition that occurs due to an inherited genetic mutation. In this progressive and incurable disease, the normal renal tissue is slowly replaced by cysts (small bags filled with watery fluid) resulting in progressive loss of kidney function and eventually need for dialysis. This condition affects both the kidneys and usually the size of the kidney can be twice or thrice their normal size.
Polycystic kidney disease can present in children or adults. The disease can be silent for many years and first present after the age of forty years with increased blood pressure and anemia.
Other Causes of Kidney Failure:
Some commonly available medicines, which are taken to reduce pain, can cause kidneys to fail if taken regularly. If you are taking painkillers regularly you should check with your doctor and ask him if they are likely to affect the kidneys.
Biopsy means taking a small piece of tissue from the organ and examining it under the microscope to learn about the nature of the disease affecting the organ.
To find out about the exact nature and cause of kidney disease your doctor may want to remove a small piece of kidney tissue and examine it under the microscope. To obtain this tissue samples the doctor will perform a kidney (also called renal) biopsy. This is done as an in-hospital procedure in the radiology department although some centres also offer out-patient kidney biopsies. The needle used for biopsy is small in size and takes out a 2 to 3 cm piece of tissue. Before doing a biopsy the doctor will do a few blood tests and give local anesthesia so that you don't feel the pain. Post procedure bed rest is usually advised for at least 6-8 hours and overnight observation in hospital is the norm.
General Information About Dialysis
Dialysis is the process for removing excess water and waste from the blood and used as an artificial replacement for lost kidney function in chronic kidney failure condition. Hemodialysis involves the use of a machine into which blood is pumped from the body and cleaned before returning it to the body. Dialysis using the natural filtering membrane of the body called "peritoneum" is called peritoneal dialysis.
In serious kidney disease, kidney function is impaired or totally lost. In such a situation, it is by the process of "dialysis" that the function of the kidney is artificially replaced. Dialysis is done only to try and maintain normal blood chemistry in the face of renal failure. It is NOT a cure for kidney disease.
There are two types of dialysis:
- Hemodialysis
- Peritoneal dialysis
Each method has it own advantages and disadvantages but it is the medical condition & the individual patient’s needs that will decide which method will suit you best.
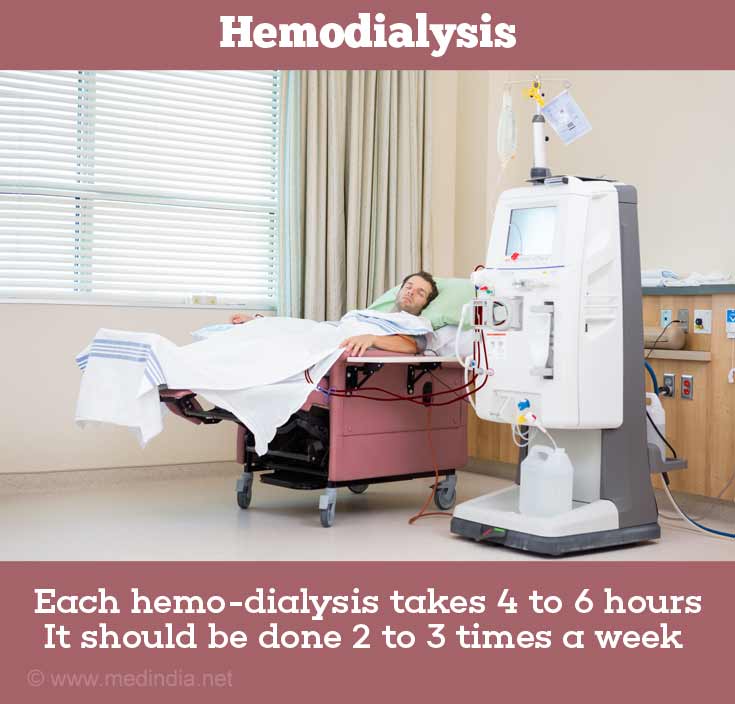
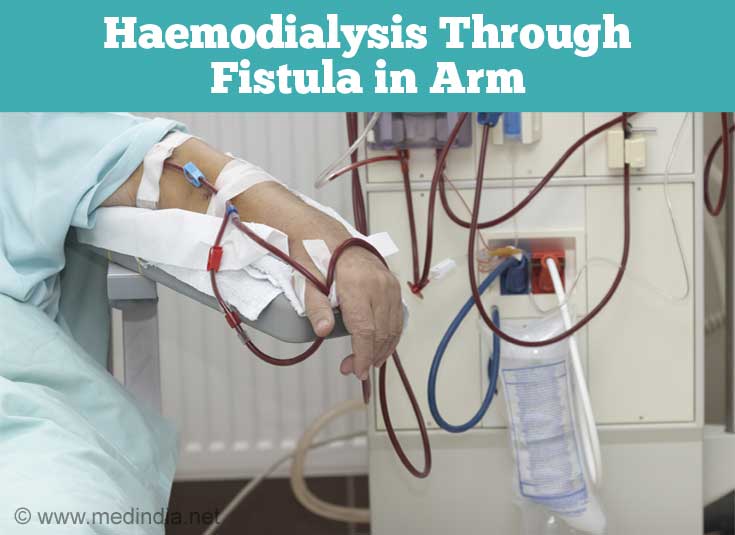
What is Hemodialysis?
Hemodialysis is done 2 to 3 times a week and takes 4 to 5 hours during each session.
In hemodialysis, the patient’s blood is pumped through a dialysis machine that filters away the waste products. This artificial kidney or dialyser is of various sizes and contains thousands of hollow fibres. These fibres act like a semi-permeable membrane, that is, they allow wastes to pass through but retain important substances like proteins. The blood circulates on one side of the membrane and the dialysate (a solution of water & electrolytes) on the other side. The toxic products and excess fluids pass through the dialyser and are carried away in the dialysate, and cleansed blood flows back into the body. The process of hemodialysis takes about 4 hours and it has to be done two to three times a week. Blood cannot be withdrawn from the body for hemodialysis via the smaller peripheral veins and requires a temporary catheter to be placed in the larger (ventral) veins or the creation of an arterio-venous fistula.
What is a "FISTULA" and How Can I Take Care of It?
An arterio-venous fistula establishes connection between a vein and an artery and is usually constructed in the forearm by a surgeon in the operation room usually under local anesthesia.
Before hemodialysis, an access to the circulation has to be created. If it is an emergency, the doctor puts in a central venous line temporarily either in the neck or in the chest or in the groin. When it is a question of long-term hemodialysis, the surgeon creates a fistula in the arm by joining up an artery and vein. This procedure can take about 45 minutes.
There are certain precautions that have to be taken with the "fistula hand" especially if it has been recently created.
Make sure that blood pressure is not taken on the fistula arm.
Regular exercise of the fistula arm should be done in the prescribed manner. Take a small rubber ball in your fistula hand and try to squeeze the ball every 5 minutes for an hour.
The fistula hand should be kept at a higher level, for example on pillows, especially when freshly created.
The fistula hand should not be kept below the level of the head when sleeping.
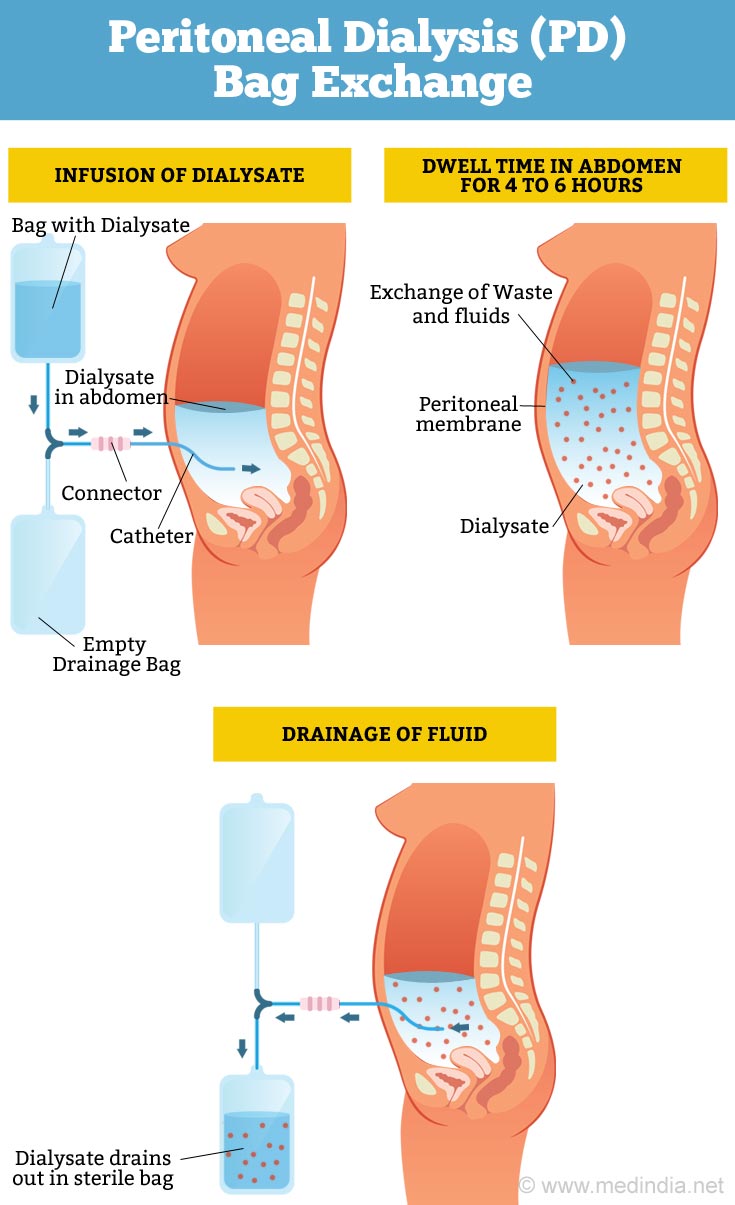
General Information About Peritoneal Dialysis
Peritoneal dialysis can be to be done in cycles throughout the day (continuous ambulatory peritoneal dialysis) or only at night via a machine (intermittent automated peritoneal dialysis).
Peritoneal dialysis is also a process by which waste products and excess fluids are removed from the blood, but unlike hemodialysis where the blood is removed from the body and passed through a machine, peritoneal dialysis is done inside the body. However peritoneal dialysis has to be done three to four times daily, unlike hemodialysis, which is done 2-3 times a week.
There are 2 types of peritoneal dialysis:
- Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Continuous Cycling Peritoneal Dialysis (CCPD)
How Does Continuous Ambulatory Peritoneal Dialysis (CAPD) Work?
Continuous ambulatory peritoneal dialysis (CAPD) works by using the peritoneal membrane of the body as a filtering unit for waste products elimination.
The peritoneal dialysis exchange procedure consists of 3 steps:
Infusion: A sterile, dialysis solution flows into the peritoneal cavity by gravity via a catheter or tube that has been surgically placed into the abdomen. The filling takes about 10 minutes. Once the filling is complete, the catheter is shut so that it does not leak.
Dwell: The lining of the peritoneal cavity called the peritoneum acts as a natural filter. It lets the waste products and excess fluids in the blood filter through into the dialysis solution, while holding back important substances that the body needs. The length of time varies from 3 - 6 hours. While the solution is in the body you can move about.
Drain: The dialysis solution containing the wastes is drained again by gravity from your body through the catheter into an empty bag. This takes about 10-20 minutes. A bag containing sterile dialysis solution replaces the bag containing waste products. The whole process is then repeated. Each of these replacements is called a 'bag exchange'.
How Does Continuous Cycling Peritoneal Dialysis (CCPD) Work?
CCPD is convenient but the cycler machine is expensive.
Continuous cycling peritoneal dialysis is done at night, while you sleep. The process takes 8-10 hours. Here, you would need to connect the catheter to a machine called the cycler. The cycler throughout the night does the bag exchanges automatically.
This is useful and a convenient form of dialysis especially for patients who are working. It also means that it is not necessary to do 3 to 4 exchanges in the daytime hence the chances of infections are less.
The cycler can cost about Rs. 1.25 lakhs, however the company could sometimes arrange a cheaper second hand machine.
How Do I Take Care Of My CATHETER-EXIT Site?
Meticulous sterility techniques like washing hands repeatedly with antiseptic solution should be followed when doing CAPD.
The catheter site needs to be carefully cleaned with:
Soap & water
Soap & water followed by povidone-iodine (PVP-I) solution
Check for:
- Any redness, bleeding, scab or crust formation at the exit site wound
- Fat necrosis (i.e. dead tissue) in the form of clear, sticky fluid
Avoid:
- Alcohol
- Powder
- Oil based ointments
- Pressure from tight clothes
- Scratching
- Tension on catheter
- Dirty skin
What Role Does Diet & Drugs Play In Dialysis?
A diet plan including fluid restrictions, if any, should be discussed with a trained renal nutritionist in conjunction with your doctor.
Either modality of dialysis are excellent methods of removing waste products from the body but they cannot act as a complete substitute to the normally functioning kidneys. So, you would need to follow a diet plan - eat the right kind of food and watch the quantity of fluid that you drink. You would also regularly need to take all the drugs that your doctor prescribes - blood pressure tablets, multi-vitamins and any others.
Certain drugs are removed by dialysis and might need supplemental doses to maintain therapeutic levels. Any new medications added to the treatment plan will have to be discussed with the nephrologist.