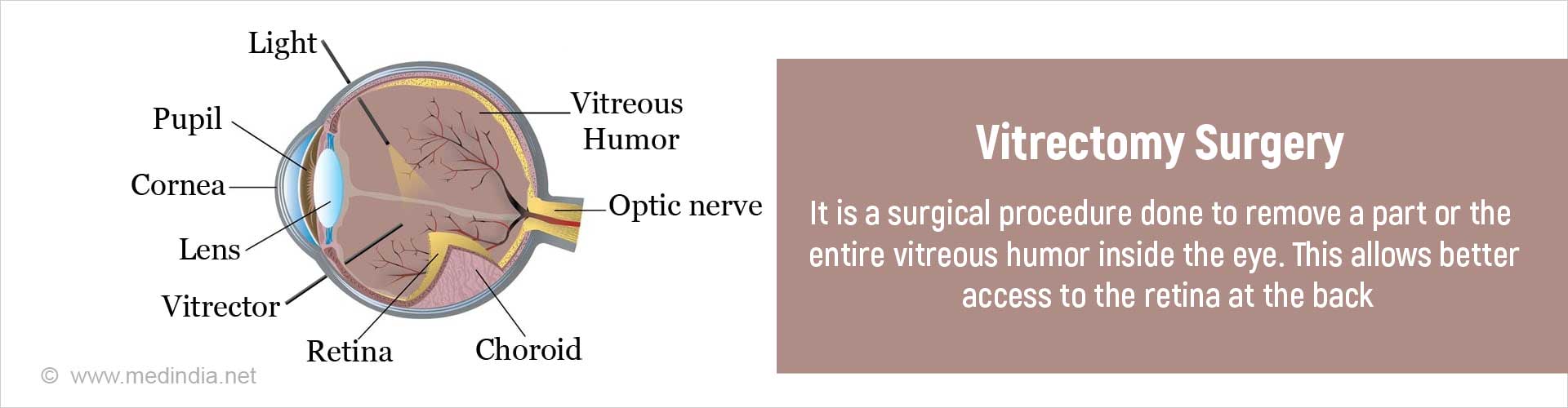
What is Vitrectomy?
Vitrectomy is a surgical procedure that involves removal of a part or whole of the vitreous humor inside the eye.
This is done either to remove a problem (such as non-resolving vitreous hemorrhage (bleeding) or an intraocular foreign body) in the vitreous, or to aid in retinal surgery.
After the procedure is completed, the removed vitreous gel is replaced by air, saline, silicone oil or a gas depending on the particular case. Gradually, aqueous which is naturally secreted by the eye takes the place of the vitreous after absorption or removal (silicone oil) of the vitreous substitute. Vitreous cannot regenerate.
What is Vitreous Humor?
The eyeball has 2 segments, an anterior segment and a posterior segment.
The anterior segment extends from the cornea to the back of the lens and is filled with a fluid called aqueous humor. The posterior segment is the part of the eye behind the lens. The space in the posterior segment between the lens and retina is filled with a clear gel called vitreous humor, commonly referred to as vitreous (4ml volume). Both the aquous and vitreous humors help to maintain the shape of the eyeball.
What are the Types of Vitrectomy?
There are 2 types of vitrectomy, based on the approach used to remove the vitreous gel; namely anterior and posterior vitrectomy.
The most common approach is the posterior or pars plana vitrectomy performed as mentioned previously in order to enable certain procedures to be done at the back of the eye. Pars plana vitrectomy vitrectomy is performed by a vitreoretinal surgeon.
Sometimes vitreous gel comes out through the pupil in the anterior segment of the eye. This may occur due to eye trauma or injury, lens problems or during cataract or glaucoma surgery. This vitreous is therefore removed via the anterior approach to prevent problems later on like retinal detachment and glaucoma and to promote recovery.
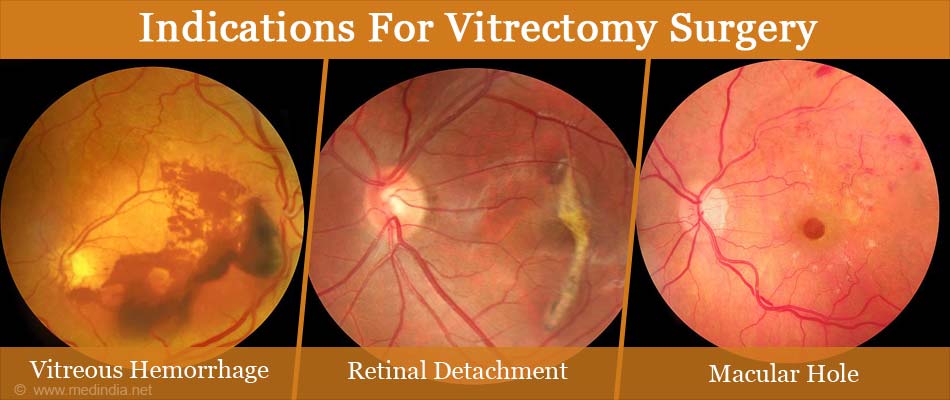
Why is a Vitrectomy Done?
Vitrectomy surgery refers to the most commonly performed pars plana vitrectomy.
Some of the conditions for which vitrectomy is indicated are given in the following table:
| Indication for vitrectomy | Purpose | |
| Complications of anterior segment surgery |
| To remove these from the vitreous |
| Following injuries that result in - |
| To remove the lens from the vitreous |
| To remove the bleeding in the vitreous, to repair tear in retina, and reattach retina | |
| To remove the foreign body and introduce antibiotics | |
| To repair tear in retina, and reattach retina if it is detached | |
| To relieve traction on the macula, and reattach retina if it is detached | |
| Retinal Detachment | Rhegmatogenous retinal detachment (detachment due to a break in the retina) | Laser to the edges of the break, removal of subretinal fluid, reattach the retina, and provide tamponade (provide pressure on the retina) till firm adhesion of retina to the underlying structures occurs. |
| Diabetic Retinopathy |
| Removal of the blood and reattach retina with tamponade |
| Disorders of the macula |
| Removal of traction and detachment repair if present |
| Removal of traction on macula | |
| Peeling of membranes off the retina | |
| Retinal Disorders in children |
| To relieve traction and repair retinal detachment |
| Ocular inflammations (Uveitis) |
| |
| Miscellaneous |
|
|
How do you Prepare for Vitrectomy Surgery?
Starting a Week Prior to Surgery
- Before surgery, you will undergo a complete eye examination that includes a slit lamp examination, examination of the fundus after dilating the eye and other diagnostic procedures such as ocular ultrasonography, fluorescein angiography(injection of contrast dye in to the veins and then observing the retinal blood vessels) and OCT or optical coherence tomography (an imaging technique that provides high quality cross sectional images of the eye).
- Your general health condition will be evaluated by doing routine blood tests and urinalysis.
- Once the decision to perform vitrectomy surgery is made, you will be advised to follow certain instructions to prepare for surgery.
- You need to inform the surgeon about any chronic health conditions such as chronic cough, hypertension, bleeding tendencies, diabetes or allergies that you may be having so that these can be controlled before the surgery to reduce complications.
- Ideally, you should stop taking anticoagulants at least a week prior to surgery, but if your systemic condition is such that stopping anticoagulants may be dangerous for your general health, then you might be asked to replace your anticoagulants with low molecular weight heparin a few days before the surgery. Leave this decision to your doctor.
- Vitrectomy is usually performed under local anesthesia. General anesthesia is used only in children, poorly cooperative patients who remain still during the procedure when the duration of the surgery is anticipated to be longer than about 3 hours.
- It would be advisable to finish pending household chores and routine activities such as paying bills, care of children or pets and shopping and stocking up on essential supplies before surgery, especially if you stay alone and do not have a full time help.
- Some patients may be asked to adopt a face down position after the surgery. Find out if this applies to you, and if so,it may be helpful to practise it for a while and get adjusted to any discomfort.
Morning of Surgery
- Most vitrectomy operations are simple and safe procedures and are performed on an outpatient basis under local anesthesia.
- You should avoid taking anything by mouth on the morning of surgery and for at least 6-8 hours prior to surgery if you are undergoing general anesthesia. You can have a light breakfast if the procedure is being done under local anesthesia.
- Follow the doctors’ advice regarding the dose or omission of certain drugs on the morning of surgery.
- Arrive on time for the procedure as this will help to reduce anxious moments.
- You will be asked to confirm the procedure and the side of the eye to be operated on, to the medical team.
- Eye drops will be instilled in your eye to dilate the pupil.
What Happens during the Surgery?
- Before the surgery, the patient is given a surgical gown to wear and asked to lie on an operating table especially designed for eye operations.
- The type of anesthesia depends on the patient’s preference as well as health status. In most cases local anesthesia is used where the anesthetic drugs are injected around the eyeball. With local anesthesia, you will be awake but sedated and feel no pain. However in anxious persons and children, general anesthesia may be given. If you are given general anesthesia, you will be asleep during the procedure.
- During the surgery the vital signs such as pulse, blood pressure and electrocardiogram (ECG) will be closely monitored.
- The eye is cleaned with antiseptic solution and covered with sterile surgical drapes. An eyelid speculum is used to keep the eye open during the surgery. 3 small openings are made in the sclera 3-3.5 mm behind the limbus (junction between cornea and sclera) roughly 1.4 mm in length. One is for introducing the infusion cannula (a thin tube through which fluid is introduced in to the eye to maintain the eye ball shape during vitreous removal), the second opening for the fiberoptic light pipe and the third for the vitrectomy instrument.
- Using a vitreous cutter, forceps and scissors, the thick vitreous gel is gently removed. A surgical microscope fitted with a special lens allows a clear and magnified view of the inside of the eye.
- Following this, the surgeon may treat other eye conditions such as retinal tear, retinal detachment, macular hole or vitreous hemorrhage.
- A laser probe may be introduced in to the vitreous to give photocoagulation to the margins of any breaks in the retina, and to the whole retina in cases like proliferative diabetic retinopathy. Drainage needles with silicone tips are used to remove fluid from the eye in retinal detachment. Forceps is used to peel and remove scar tissue and membranes over the retina.
At the end of the procedure, the vitreous needs to be replaced by a vitreous substitute. If there is no retinal detachment, then air or saline (which is absorbed in a couple of days) can be used. However, if there is a retinal detachment, the vitreous substitute is also required to maintain tamponade by keeping the retina in place till the breaks develop permanent adhesions, and retinal reattachment takes place. So either sulphur hexafluoride gas (which lasts for 10-14 days) is used, or in more complex detachments, a longer lasting gas like perfluorohexane or perfluoropropane is used. Alternately, silicone oil may also be used for longer lasting tamponade.
- The openings are closed with sutures.
- Nowadays, in selective cases, 23, 25 and 27 gauge needle vitrectomies are being done. These small incisions do not require suturing.
What Happens after Surgery and during Recovery
- After surgery, the eye is patched and a shield placed to protect the eye from injury. This shield should be used at night for a week after surgery.
- After ensuring the vital signs are stable, you will be shifted to your room.
- If a gas bubble or silicone bubble has been injected into the eye, you will be required to adopta particular head position depending on the position of the break. Since the bubble floats up, you will be asked to adopt a posture such that the bubble lies against the break. (this is so that the break is tamponaded to enable permanent sealing of the break.)
- Since the surgery is performed under local anesthesia, you can return home on the same day. However, if there are concerns about a raised intraocular pressure, you may be asked to stay one or two nights in the hospital.
- If the surgery is performed under general anesthesia, recovery takes longer and you may have to stay overnight at least in the hospital.
- It is advisable to arrange in advance your transport back home after surgery and the visit to the surgeon on the day after surgery
Recovery at Home
- You may be asked to return for a check up on the day after surgery and to renew instructions about routine activities, use of the eye patch, medications and eye position and to schedule the next visit.
- Eye drops to reduce infection and inflammation are routinely prescribed. If you need to put more than one type of eye drop at the same time of the day, wait at least 5 minutes between successive drops. Painkillers such as Ibuprofen and Paracetamol may be prescribed.

- Instructions on maintaining the head position have to be followed as indicated. The head position has to be maintained for atleast 45 minutes out of every 60 mintues. Those 15 minutes are for acitvies such as eating, visiting the rest room and stretching your feet.
- There may be an itchy sensation due to the use of sutures but these will be absorbed in 2-3 weeks. A lubricating eye ointment may be used as needed.
- You may experience floaters or light flashes for a few days after surgery. Vision will be blurry because of the gas, and will improve once the gas disappears.(about 3-8 weeks).
- Straining and lifting heavy weights should be avoided for at least a week after surgery.
- Regular medications and activities may be resumed as per the doctor’s advice.
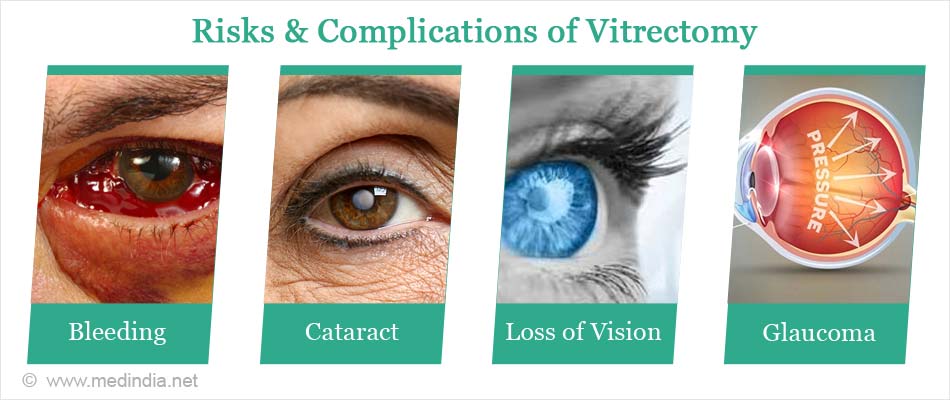
What are the Risks and Complications of Vitrectomy?
Vitrectomy is a very safe procedure and complications are rare. However reported complications include the following:
- Bleeding
- Infection
- Retinal detachment
- Scar tissue formation
- Loss of vision
- Increased eye pressure or glaucoma
- Progression of cataract needing cataract surgery at a later date.
When should Vitrectomy not be done?
A vitrectomy is contraindicated when the patient is not able to perceive any kind of light (described as “no light perception”)