Bone marrow transplant was first done successfully in 1968. The surgical procedure is required for treating those suffering from leukemia, aplastic anemia, Hodgkin’s disease.
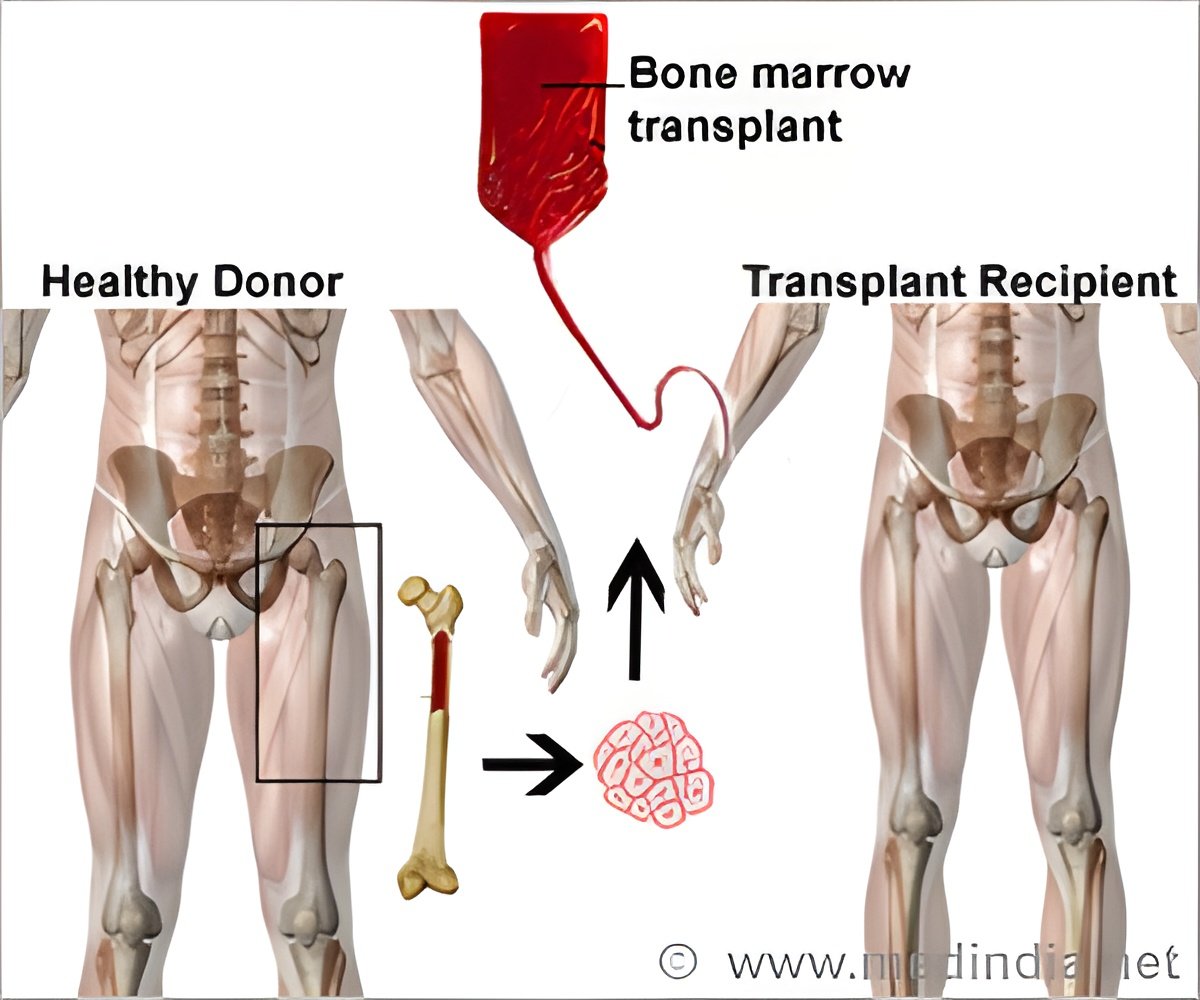
Blood and bone marrow transplant is a highly specialized procedure that is done “when special cells called the stem cells (found in the bone marrow) are taken out, filtered and given back to either the same person or the other individual.”
Bone marrow transplantation is needed in patients suffering from blood cancers including leukemia.
There are two types of bone marrow transplants. They are namely:
1. Autologous bone marrow transplant – In this transplant, the donor’s cells are re-introduced into the same person.
2. Allogenic bone marrow transplant – In this transplant, the donor is a person whose ‘tissue has the same genetic type as the person needing the transplant (recipient). Because tissue types are inherited, similar to hair or eye color, it is more likely that the recipient will find a suitable donor in a brother or sister. This, however, happens only 25 to 30 percent of the time.’
Peripheral blood stem cells are the blood cells that have moved from the bone marrow into the blood following administration of special drugs like filgrastim or lenograstim, a process that is identical to routine blood donation ‘which collects the peripheral blood stem cells through a tube inserted in a vein. A critical step before the transplant involves finding a donor that is tissue matched to the recipient.’
The study showed no significant variations in the relapse rates, overall survival or acute graft-versus-host disease (GHVD) between recipient and unrelated donor. Engraftment was quick in recipients of peripheral blood stem cells. These patients also reported high rates of chronic graft-versus-host disease (GHVD).
Anasetti, the lead author of the study mentioned, “Although peripheral blood stem cells from related donors have demonstrated clinical benefits, our trial demonstrates that when these stem cells originate from unrelated donors, they are not superior to bone marrow stem cells in terms of patient survival, and they increase the risk for chronic GVHD."
The author further added, "More effective strategies to prevent GVHD are needed to improve outcomes for all patients receiving unrelated donor transplants."
The scientists firmly believed, “There is a need to develop transplantation approaches that decrease the risk of graft failure when bone marrow is used and that decrease the risks of acute and extensive chronic GVHD when either stem-cell source is used.”
The study was financially supported by the National Heart, Lung and Blood Institute (U10HL069294), the National Cancer Institute and the National Marrow Donor Program.
Reference:
Peripheral-Blood Stem Cells versus Bone Marrow from Unrelated Donors; Claudio Anasetti et al; N Engl J Med 2012; 367:1487-1496, 2012DOI: 10.1056/NEJMoa1203517
Source-Medindia














