- Nephrotic Syndrome in Children - (https://www.niddk.nih.gov/health-information/kidney-disease/children/nephrotic-syndrome-children)
- Nephrotic Syndrome - (https://www.ncbi.nlm.nih.gov/books/NBK470444/)
- Nephrotic Syndrome in Children: From Bench to Treatment - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163400/)
- Nephrotic syndrome in childhood - (https://pubmed.ncbi.nlm.nih.gov/12944064/)
- Is there really an increase in non-minimal change nephrotic syndrome in children? - (https://pubmed.ncbi.nlm.nih.gov/14655180/)
- Congenital nephrotic syndrome - (https://pubmed.ncbi.nlm.nih.gov/17968594/)
- Risk factors for relapse in childhood nephrotic syndrome - (https://pubmed.ncbi.nlm.nih.gov/8971894/)
- Nephrotic Syndrome: Oedema Formation and Its Treatment With Diuretics - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6341062/)
- Disorders of lipid metabolism in nephrotic syndrome: mechanisms and consequences - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5812444/)
- Management of childhood onset nephrotic syndrome - (https://pubmed.ncbi.nlm.nih.gov/19651590/)
- Proteinuria - (https://www.ncbi.nlm.nih.gov/books/NBK705/)
- Methodological evaluation and comparison of five urinary albumin measurements - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6647735/)
- Congenital Nephrotic Syndrome - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6647735/)
- Corticosteroid therapy for nephrotic syndrome in children - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7025788/)
- Pediatric Immunization Practices in Nephrotic Syndrome: An Assessment of Provider and Parental Knowledge - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7901920/)
- Steroid-sensitive nephrotic syndrome in children: triggers of relapse and evolving hypotheses on pathogenesis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4379699/)
What is Childhood Nephrotic Syndrome?
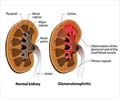
Childhood nephrotic syndrome (NS) is a complex condition consisting of distinct subtypes of glomerular histopathology and clinical courses in children. It is also called 'Nephrosis' and occurs when tiny structures in the kidneys called glomeruli stop working properly(1✔ ✔Trusted Source
Nephrotic Syndrome in Children
Go to source). Most commonly it is a condition that causes the kidneys to leak large amounts of protein into the urine. These glomeruli filter blood and allow excess water and waste products to pass into the urine while serving as a barrier for the passage of substances which are essential for the body such as proteins. In nephrotic syndrome, these glomeruli become leaky and allow the passage of proteins like albumin into urine. This loss of protein leads to low protein levels in the blood and the many symptoms of nephrotic syndrome as described below.
Nephrotic syndrome is defined as massive proteinuria (>40 mg/m2/hr), hypoalbuminemia (<2.5 g/dL), edema, and hyperlipidemia in most of the cases. It occurs mostly in young children between the ages of 1 and 6 years, although children of all ages and even adults can get affected. It has been reported to show a prevalence of nearly 16 cases per 100 000 children(2✔ ✔Trusted Source
Nephrotic Syndrome
Go to source).
What are the Causes of Childhood Nephrotic Syndrome?
The causes of Childhood Nephrotic Syndrome can be divided into three categories:
Primary Childhood Nephrotic Syndrome occurs without an identifiable cause such as infections, autoimmune diseases or drugs. Histologically, it mainly includes Minimal-change nephrotic syndrome (MCNS) and Focal segmental glomerulosclerosis (FSGS) which are collectively called Idiopathic Nephrotic Syndrome(3✔ ✔Trusted Source
Nephrotic Syndrome in Children: From Bench to Treatment
Go to source). About 80% children suffering with idiopathic nephrotic syndrome show remission of proteinuria following treatment with corticosteroids, and are therefore, classified as steroid–sensitive nephrotic syndrome.
Minimal-change nephrotic syndrome (MCNS) - In minimal change disease, there is damage to the glomeruli involved in urine formation. The damage is only visible under an electron microscope. It may be idiopathic or can be related to allergic reactions, use of non-steroidal anti-inflammatory drugs (NSAIDs), tumours, vaccinations (flu and pneumococcal) and viral infections. Many studies show that there is a high incidence of minimal change nephrotic syndrome in Asians(4✔ ✔Trusted Source
Nephrotic syndrome in childhood
Go to source).
Focal segmental glomerulosclerosis is described as scarring (sclerosis) in the kidney. Although it is much less common than MCD, it is increasing in incidence and can lead to permanent kidney damage(5✔ ✔Trusted Source
Is there really an increase in non-minimal change nephrotic syndrome in children?
Go to source).
Secondary Childhood Nephrotic Syndrome
This is caused by an underlying disease or infection that results in changes in kidney function. Some of the causes of secondary nephrotic syndrome include the following(2✔ ✔Trusted Source
Nephrotic Syndrome
Go to source):
- Systemic diseases such as lupus and vasculitis. Vasculitis is characterised by inflammation of the small blood vessels. IgA vasculitis (also called Henoch-Schönlein purpura) can cause nephrotic syndrome with rash in children.
- Drugs such as NSAIDs
- Infection related glomerulonephritis which can occur with streptococcal skin and throat infections
- Infections such as Hepatitis B and C and HIV
Congenital (Inherited) Nephrotic syndrome - It is a very rare form of nephrotic syndrome and develops shortly after birth affecting infants in the first 3 months of life. Most of these cases are related to genetic mutations. Mutations in the transmembrane protein known as nephrin cause congenital (Finnish-type) nephrotic syndrome(6✔ ✔Trusted Source
Congenital nephrotic syndrome
Go to source).
What are the Risk Factors for Childhood Nephrotic Syndrome?
Childhood nephrotic syndrome occurs mostly in children between the ages of 1 and 6. Some of the risk factors include the following(7✔ ✔Trusted Source
Risk factors for relapse in childhood nephrotic syndrome
Go to source):
- Family history of kidney disease:A family history of kidney disease is associated with an increased risk of childhood NS
- Gender: Boys are affected more often than girls
- Certain medications, such as NSAIDs (e.g. celecoxib) and some antibiotics
- Certain types of infections, such as HIV, Hepatitis B & C, and malaria.
- Environmental factors
What are the Symptoms and Signs of Childhood Nephrotic Syndrome?
The signs and symptoms of childhood nephrotic syndrome include:
- Edema- Edema is the prominent feature of nephrotic syndrome and initially develops with swelling around the eyes and legs, feet, or ankles and less often in the hands or face(8✔ ✔Trusted Source
Nephrotic Syndrome: Oedema Formation and Its Treatment With Diuretics
Go to source).
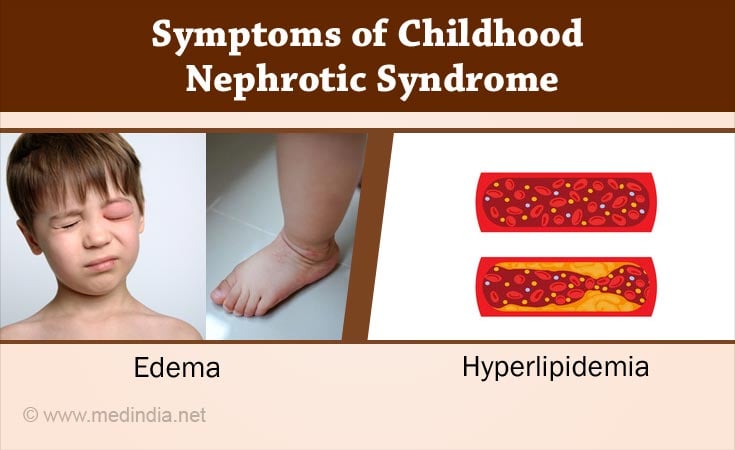
- Albuminuria - The child’s urine has high levels of albumin (>40 mg/m2/hr) which can be detected by a urine dipstick test(2✔ ✔Trusted Source
Nephrotic Syndrome
Go to source) - Hypoalbuminemia- In this condition, a child's blood has low levels of albumin (<2.5 g/dL)(2✔ ✔Trusted Source
Nephrotic Syndrome
Go to source). - Hyperlipidemia - This is characterized by raised serum cholesterol and triglyceride concentrations and is another major finding of nephrotic syndrome(9✔ ✔Trusted Source
Disorders of lipid metabolism in nephrotic syndrome: mechanisms and consequences
Go to source). In this case the child’s blood cholesterol and fat levels are higher than normal. This clinical manifestation occurs from interactions between disordered lipoprotein metabolism, medications, and dietary factors(10✔ ✔Trusted Source
Management of childhood onset nephrotic syndrome
Go to source).
How do you Diagnose Childhood Nephrotic Syndrome?
Following parameters should be considered for diagnosing Childhood Nephrotic Syndrome:
- Medical and family history - In most cases, a detailed and precise medical or family history is checked by the healthcare provider and it gives a definite clue to the diagnosis. Through this history, the doctor will gather more data about signs and symptoms, allergy or related diseases.
- Physical examination -During physical examination, a health care provider most often examines for abdominal distension and tenderness, patches on the skin, fever and blood pressure.
- Urine tests - The doctor performs following urine tests to help determine if a child has childhood nephrotic syndrome.
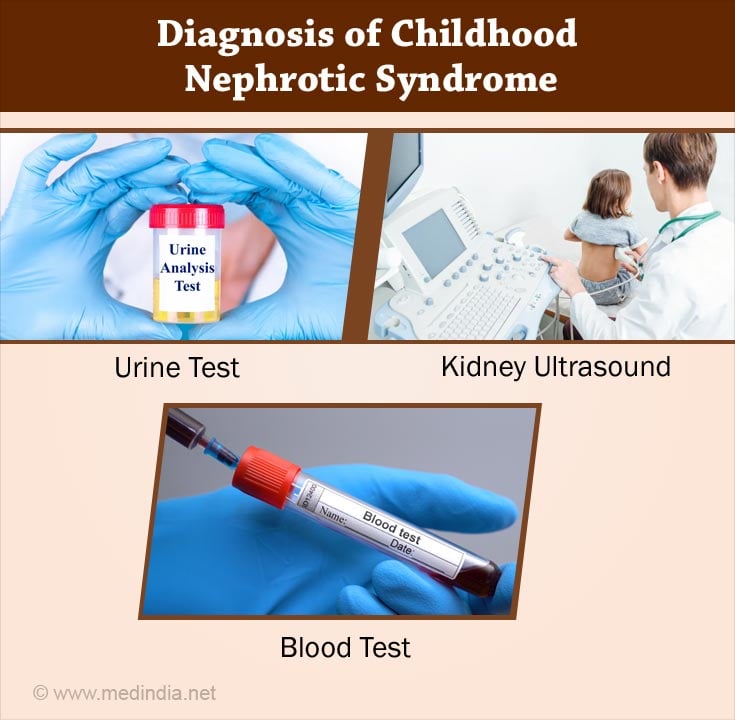
- The dipstick method (colorimetric reagent strip) - This test is based on the ability of proteins to alter the colour of specific acid-base indicators, like tetrabromophenol blue, without changing the pH. It detects the presence of albumin in the urine(11✔ ✔Trusted Source
Proteinuria
Go to source). When the dye is buffered at pH 3, it is yellow; on increasing the concentration of protein it changes the colour to green and then to blue. The developed color is compared with a color chart which allows the protein concentration to be graded from trace to 4 +, corresponding to concentrations from 1 to 10 mg/dl to greater than 500 mg/dl. It is a low cost and rapid method for screening children for proteinuria and also for the home monitoring of children with nephrotic syndrome who have been started on treatment and can often give a result within 2 minutes. - Sulfosalicylic acid test - It requires centrifugation of the urine followed by addition of 2.5 ml of the supernatant to 7.5 ml of 3% sulfosalicylic acid(2✔ ✔Trusted Source
Nephrotic Syndrome
Go to source). The degree of turbidity is quantified to the amount of albumin present in urine.Immunology-based methods which are used in most laboratories such as immunonephelometry and radioimmunoassay - These can give a quantitative measurement of the albumin in urine(12✔ ✔Trusted Source
Methodological evaluation and comparison of five urinary albumin measurements
Go to source) - Urine High Performance Liquid Chromatography - It is able to detect all the immunoreactive intact albumin and non-immunoreactive intact albumin (total intact albumin) in urine which are not detected by dipstick test. It is more accurate than the dipstick test.
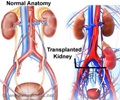
- Ultrasound of the kidney - Ultrasound is the preferred imaging modality to diagnose kidney damage due to paediatric nephrotic syndrome. The advantages of ultrasonography include high accuracy, the ability to detect lead points, and absence of radiation.
- Computed tomography (CT)and magnetic resonance imaging (MRI) or additional imaging may be needed in complex clinical situations like presence of lymphoma(13✔ ✔Trusted Source
Congenital Nephrotic Syndrome
Go to source). - Kidney biopsy - In spite of the new and less invasive tests available today, renal biopsy is still considered suitable by most nephrologists as an important tool in diagnosis and prognosis and in deciding therapy in many renal diseases. Most nephrologists refrain from doing a renal biopsy in the paediatric patients as most of them respond to therapy with steroids but in adults, almost everyone performs a biopsy before starting therapy.
- Blood test - In case of nephrotic syndrome, a blood test may show low levels of the protein albumin (hypoalbuminemia) (being below its normal range of 3.5-4.5 g/dL)(2✔ ✔Trusted Source
Nephrotic Syndrome
Go to source). Serum creatinine and blood urea also may be measured to assess your overall kidney function. The normal serum creatinine level of a child is approximately 0.5 mg/dL and values higher than this in children indicate reduced kidney function. - Genetic testing - This may be required in some cases such as congenital nephrotic syndrome, those with family history of nephrotic syndrome and some patients who do not respond to steroids to detect genetic mutations.
How do you Treat Childhood Nephrotic Syndrome?
- Corticosteroid therapy -The main treatment for childhood nephrotic syndrome is steroid therapy. A trial of corticosteroids is the first step in treatment of idiopathic nephrotic syndrome (INS). Children once diagnosed with nephrotic syndrome are treated for the first time with a 4-6 week course of steroids (prednisolone), followed by a smaller dose every other day for 4-6 more weeks(14✔ ✔Trusted Source
Corticosteroid therapy for nephrotic syndrome in children
Go to source). If the urine protein is negative or trace on dipstick testing for 3 consecutive days, it is called remission of proteinuria. Relapse is defined as reappearance of at proteinuria (3+ or more on dipstick) in a child who had previously attained remission. Some children who are steroid responsive require prolonged courses of prednisone to remain in remission or develop relapse when reducing the dose of steroids in which situation, they are said to have steroid dependent nephrotic syndrome.In steroid resistant nephrotic syndrome, the children do not respond to the 6 week course of daily steroids.The most common cause of steroid-resistant nephrotic syndromeis focal segmental glomerulosclerosis so these patients are treated with a specific protocol that involves prolonged courses of steroids and, in many cases, calcineurin inhibitors such as cyclosporine and tacrolimus and oral alkylating agent therapy such as cyclophosphamide are also used.

- Diuretics - Severe edema in children with nephrotic syndrome may be associated with volume contraction (VC) or volume expansion (VE). Metolazone may be beneficial in combination with furosemide (Lasix) for resistant edema(8✔ ✔Trusted Source
Nephrotic Syndrome: Oedema Formation and Its Treatment With Diuretics
Go to source). - Home monitoring- Regular weight record and urine examination should be done by parents for their children.
- Vaccinations- Children with nephrotic syndrome are advised to have the pneumococcal vaccine(15✔ ✔Trusted Source
Pediatric Immunization Practices in Nephrotic Syndrome: An Assessment of Provider and Parental Knowledge
Go to source). Some children may also be recommended the chickenpox vaccination between relapses.
How do you Prevent Childhood Nephrotic Syndrome?
The only way to prevent nephrotic syndrome is to control the diseases that can cause kidney infection or damage. Upper respiratory tract infections are often triggers for relapse in children with frequent relapse of nephrotic syndrome and in such children, their doctor may prescribe a short course of steroids for 5-7 days during the infection to prevent relapse(16✔ ✔Trusted Source
Steroid-sensitive nephrotic syndrome in children: triggers of relapse and evolving hypotheses on pathogenesis
Go to source).
How to care of children with Nephrotic Syndrome?
Children who have nephrotic syndrome may need to make changes to their eating habits and limit their salt (sodium), fat and cholesterol intake(17✔ ✔Trusted Source
Nephrotic Syndrome in Children
Go to source). They should maintain a healthy lifestyle and clean habits to prevent infections. During steroid therapy, the parents and caretakers should be aware of the side effects of steroids such as weight gain, puffiness of face, increased bruisability of skin as well of increased risk of complications of infections such as measles and chickenpox. They should ensure as far as possible that their child's vaccination status is up-to-date prior to the onset of illness. During the illness, they should get the guidance from their doctor regarding which vaccinations are suitable and which are to be avoided during the treatment period. In case of fever in the child or contact with persons with measles or chicken pox, they should report to their doctor immediately to seek therapy. Parents and caretakers can also learn to monitor proteinuria by home dipstick testing to detect disappearance and reappearance of proteinuria.