- Persistent Depressive Disorder - (https://medlineplus.gov/ency/article/000918.htm)
- Dysthymia - (https://www.health.harvard.edu/newsletter_article/dysthymia)
- Persistent Depressive Disorder - (https://familydoctor.org/condition/dysthymic-disorder/)
- Persistent Depressive Disorder (Dysthymia) - (https://www.mayoclinic.org/diseases-conditions/persistent-depressive-disorder/symptoms-causes/syc-20350929)
What is Dysthymia or Persistent Depressive Disorder (PDD)?
Dysthymia or persistent depressive disorder (PDD) is a type of chronic depression where the person more often experiences low mood and self-esteem.
- Symptoms include fatigue, low self-esteem and pessimism.
- The essential feature of PDD is the occurrence of low mood for most of the day, for most days of the year and lasting for at least 2 years in adults and at least one year in children and adolescents.
- However, the symptoms range from mild to moderate and are not as severe when compared to major depression. Due to the milder symptoms, family and friends may not be aware that the individual is depressed.
The incidence of PDD is 4% in the population and is higher in adolescent and adult women and in psychiatric patients. Formerly known as dysthymia or dysthymic disorder, PDD is a condition that affects young and old people. In children, both girls and boys are affected with PDD in a similar ratio.
How Does Dysthymia or PDD Differ From Major Depression?
Very often distinguishing between PDD and major depression is not easy. However, there are subtle differences which will be evident on careful questioning.
- Major depression is of sudden onset, usually preceded by a stressor such as loss of job or a divorce. PDD is a chronic longterm condition and symptoms are present almost every day for at least two years.
- To qualify for diagnosis of major depression, the episode of depressive symptoms must be present for at least two weeks unlike PDD which is more longterm.
- An episode of major depression may completely go away once the person learns to cope with the stressor and he may become normal or be in remission. In PDD on the other hand the symptoms are present to a less severe degree for much longer
- Importantly the intensity of symptoms is different. In major depression, the symptoms are severe and significant enough to affect daily functioning. In PDD, the symptoms are not that severe and can easily be overlooked by the patient and his family.
- Thus PDD (dysthymia) is low level depression that is more chronic but there is always a risk of developing into a major depressive episode at the slightest trigger.
- Both conditions are characterized by similar symptoms (albeit differing intensity) and may both respond well to medication and/or counseling.
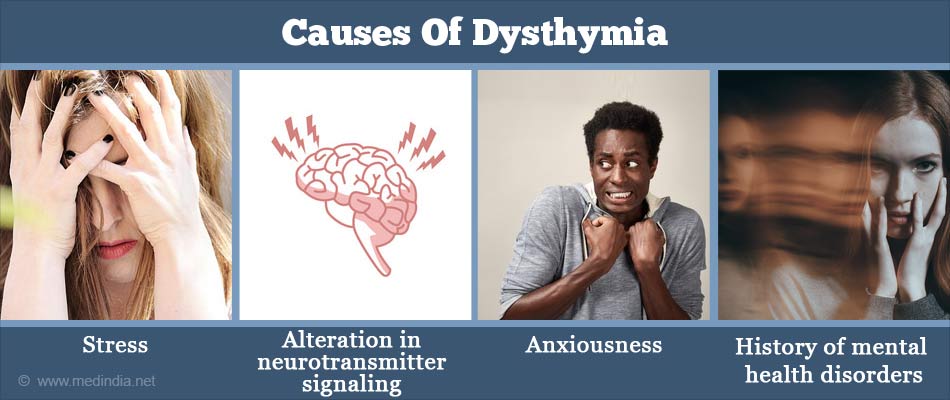
What are the Causes of Dysthymia or PDD?
The exact cause of PDD is unclear and there are some recognized risk factors that might cause dysthymia to develop
- Traits of PDD tend to be observed in different generations in affected families. This indicates a genetic susceptibility in these affected individuals.
- Environmental factors such as stress, loss of parent, abuse, financial difficulties may trigger dysthymia
- Brain chemicals called neurotransmitters are responsible for the functioning of the intricate brain signaling network. When there is an alteration in neurotransmitter signaling (e.g. serotonin), PDD could occur.
- Personality traits of the person – low self-esteem, pessimistic, timid and anxious
- Physical differences in the brains of such persons that are yet to be precisely pinpointed
- Previous history of mental health disorders
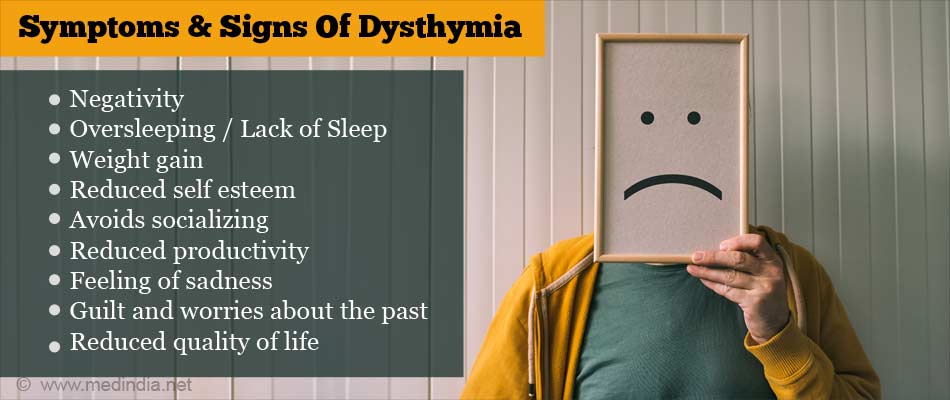
What are the Signs and Symptoms of Dysthymia or PDD?
The symptoms of PDD are listed below:
- Negativity or pessimistic outlook
- Oversleeping or insufficient sleep
- Reduced self-esteem
- Reduced or increased appetite
- Weight gain
- Inability to take decisions
- Exhaustion and becoming tired easily
- Inability to focus or concentrate
- Feeling of sadness
- Excessive anger or irritability
- Avoids socializing
- Reduced productivity
- Lack of interest in daily routine and reduced quality of life
- Guilt and worries about the past
Children may not demonstrate the classic signs and symptoms described above. However, they tend to exhibit irritable mood swings resulting in disobedient behavior.
How do you Diagnose Dysthymia or PDD?
The Diagnostic and Statistic Manual of Mental Health (DSM-5) criteria are used to diagnose PDD. Early onset of PDD indicates symptoms that manifest in an individual below 21 years of age and late onset occurs in older individuals.
In children, PDD is diagnosed as symptoms that persist for nearly the whole day for at least a year.
For adults, PDD is diagnosed as persistence of symptoms for the most part of the day for either 2 or more years.
To diagnose PDD, the primary care physician will conduct a detailed history and medical examination of the patient to determine the cause of depression. Medications or any related illness may be the cause of PDD. Symptoms, such as sleep issues, trouble to focus, fatigue, may also assist in diagnosing PDD.
Psychological assessment of the patient can give a clearer picture of the type of depression affecting the individual, e.g. major depression, PDD or bipolar disorder.
Lab tests, such as blood or urine tests are performed to assess the functioning of organs, such as thyroid because reduced thyroid function (hypothyroidism) can lead to depressive symptoms.
How do you Treat Dysthymia or PDD?
Dysthymia can be treated with a combination of medications and psychotherapy. This strategy is more effective compared with implementing either strategy in isolation. The choice of treatment depends on the severity of symptoms, ability to tolerate the medications, previous treatment responses, other associated mental health issues and personal preference.
Psychotherapy:
Cognitive behavioral analysis system of psychotherapy (CBASP) can help in tackling interpersonal behavioral issues. Other forms of psychotherapy include psychodynamic therapy, cognitive therapy, manualized group therapy and interpersonal or insight-oriented psychotherapy.
Usually psychotherapy is recommended as first line of management in children and adolescents.
Medications or pharmacotherapy:
Tricyclic antidepressants (TCA), serotonin norepinephrine reuptake inhibitors (SNRI), selective serotonin reuptake inhibitors (SSRI), and monoamine oxidase inhibitors show a beneficial effect in dysthymia.
Medications, such as venlafaxine, bupropion, nefazodone, duloxetine, amisulpride, and second-generation drugs are effective in treating dysthymia.
Improvement with medications normally takes effect in 2 to 4 weeks and the positive impact of the medications on dysthymia can be observed in a few months. However, patients may experience reduced drug effectiveness with time.
Patients may also experience relapses on continued treatment with one drug. Hence, medications will need to be changed to maintain treatment efficiency.
How do you Prevent Dysthymia or PDD?
It is difficult to prevent the onset of PDD. However, one can address the symptoms and obtain treatment at the earliest. Children who are diagnosed with PDD, if treated early, can avoid a relapse. Some ways to prevent PDD are:
- Talk to friends and family who provide ample support during tough times
- Avoid stress and any conditions that lead to stress. This measure will boost the patient’s confidence and self-esteem. Practise relaxation techniques such as meditation and yoga
- Access long-term treatment strategy to prevent a relapse of PDD
- Treat PDD at the earliest to prevent the exacerbation of symptoms
- Lifestyle changes such as regular sleep habits, regular exercise and healthy diet
- Avoid alcohol and other habit forming drugs