- What is MDS? - (https://www.mds-foundation.org/wp-content/uploads/2012/04/pages63-64-commonquestions.pdf)
- Understanding Myelodysplastic Syndromes (MDS) - (https://www.mds-foundation.org/what-is-mds/)
- Pathogenesis of myelodysplastic syndromes: an overview of molecular and non-molecular aspects of the disease - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4278002/)
- Tests and diagnosis myelodysplastic syndrome - (http://www.mayoclinic.org/diseases-conditions/myelodysplastic-syndromes/basics/tests-diagnosis/con-20027168)
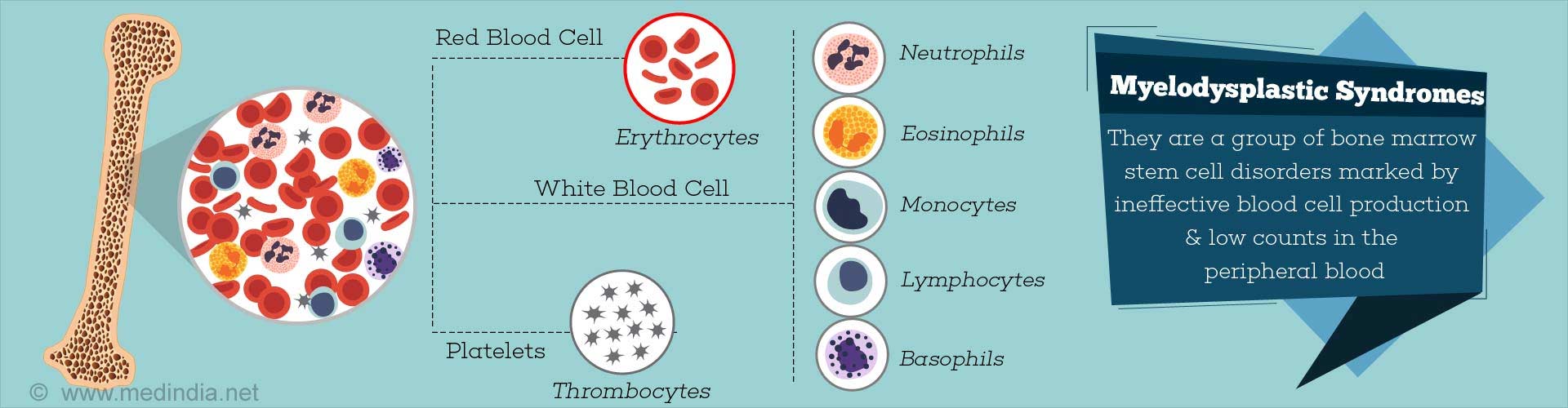
What are Myelodysplastic Syndromes?
In a normal bone marrow, the precursors (stem cells) of blood cells, namely the red cells, white cells (especially the neutrophils) and the platelets undergo a process of maturation and form mature cells which get released into the peripheral blood. The process of formation of mature blood cells from precursors in the marrow is referred to as hematopoiesis.
- Myelodysplastic syndromes (MDS) refer to a group of bone marrow hematopoietic stem cell disorders characterized by insufficient production of mature blood cells, namely the red cells (RBC), white cells (WBC) and platelets.
- The precursors of the blood cells fail to mature normally within the marrow. In addition, these precursors show abnormal forms (dysplasia) in their size and shape. These stem cells have also been shown to have a reduced lifespan.
- In effect, there is a defect in the maturation process with low counts of mature RBCs, WBCs and platelets in the peripheral blood. The low blood counts of mature cells is referred to as cytopenias.
- Also there may be increased numbers of immature blood cells or blasts in the peripheral blood.
- MDS is predominantly a disease of the elderly and typically affects persons over the age of 65. The disease tends to occur at a younger age in Asian populations.
- There is an increased risk of progression from MDS to acute myeloid leukemia (AML).
What are the Types of Myelodysplastic Syndromes?
The World Health Organization has evolved a classification of MDS that is undertaken by hematologists at the time of diagnosis. The classification of MDS carries some prognostic significance. The various types of MDS include:
- Refractory cytopenias with unilineage dysplasia (RCUD)
- Refractory anemia with ring sideroblasts (RARS)
- Refractory cytopenia with multi-lineage dysplasia (RCMD)
- Refractory anemia with excess blasts-1 (RAEB-1) – less than 5% blasts in peripheral blood
- Refractory anemia with excess blasts-2 (RAEB-2) – 5-19% blasts in peripheral blood
- Myelodysplastic syndrome: unclassified (MDS-U)
- MDS associated with isolated del (5q)
Among the MDS types, RARS is associated with an overall good prognosis.
What are the Causes and Risk Factors of Myelodysplastic Syndromes?
The cause of MDS is known in only about 15% of cases. The rest of the cases have no known identifiable cause and are referred to as ‘de novo’ or primary MDS. MDS with an identifiable cause is termed secondary MDS.
Risk factors for MDS development
- Inherited predisposition - Down's syndrome, Fanconi anemia and neurofibromatosis.
- Family history of MDS, aplastic anemia or acute myeloid leukaemia.
- Environmental factors/Therapy related – Exposure to previous chemotherapy, radiotherapy, ionizing radiation, alkylating agents, purine analogues.
- Occupation related – Exposure to benzene, agricultural workers, industrial workers.
In general, the secondary forms of MDS are more difficult to treat and carry a poor prognosis, though there may be variations. In contrast primary MDS is easier to treat.
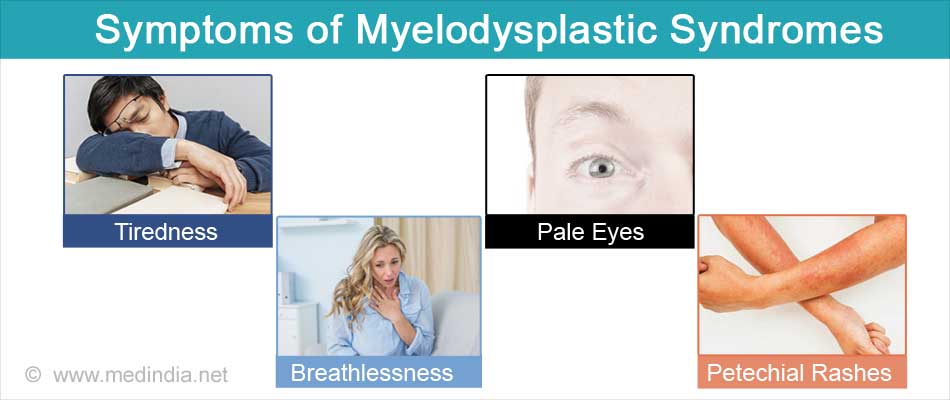
What are the Symptoms of Myelodysplastic Syndromes?
MDS develops gradually and rarely is symptomatic in the early stages. With progression, the clinical features are related to low levels of mature cells (cytopenias) in the peripheral blood, namely anemia (low RBCs), leucopenia (low WBCs) and platelets (thrombocytopenia).
- Tiredness and easy fatigability
- Breathlessness on exertion
- Pale eyes and mucous membranes due to anemia
- Recurrent infections
- Easy bruising and bleeding
- Reddish spots on the skin due to minor bleeds (Petechial rashes)
How do you Diagnose Myelodysplastic Syndromes?
MDS is usually a diagnosis of exclusion and obtaining a detailed history of the patient. Physical examinations and tests are essential to rule out other conditions such as renal failure, chronic infections, aplastic anemia, medications and alcohol ingestion.
If the diagnosis is suspected clinically, further tests such as blood tests and bone marrow tests including cytogenetics are done to confirm the diagnosis.
It should be emphasized that every case should be classified according to the WHO criteria mentioned above and prognosis of each case assessed by the International Prognostic Scoring System (IPSS).
Blood tests:
- Peripheral blood counts may show cytopenias in one or more lineages i.e. in RBC, WBC or platelets.
- Abnormal forms of red cells, white cells and platelets can be identified on a blood film examination.
- Increased numbers of immature cells or blasts may be seen in the blood film.
- Biochemical tests such as lactate dehydrogenase (LDH), ferritin, transferrin and transferrin saturation, vitamin B12 and folate concentrations, reticulocyte counts, haptoglobin, creatinine and endogenous erythropoietin (EPO) levels may help in excluding or supporting a diagnosis of MDS.
- If the diagnosis of MDS is established, LDH and ferritin levels have a prognostic value.
- Levels of EPO can help to decide whether or not to treat with erythropoietin stimulating agents.
Bone marrow tests: Bone marrow aspirate
During a bone marrow aspirate, a needle is introduced into the marrow usually on the back of the hip bone. A small amount of liquid marrow is drawn out and spread on a glass slide for microscopic analysis.
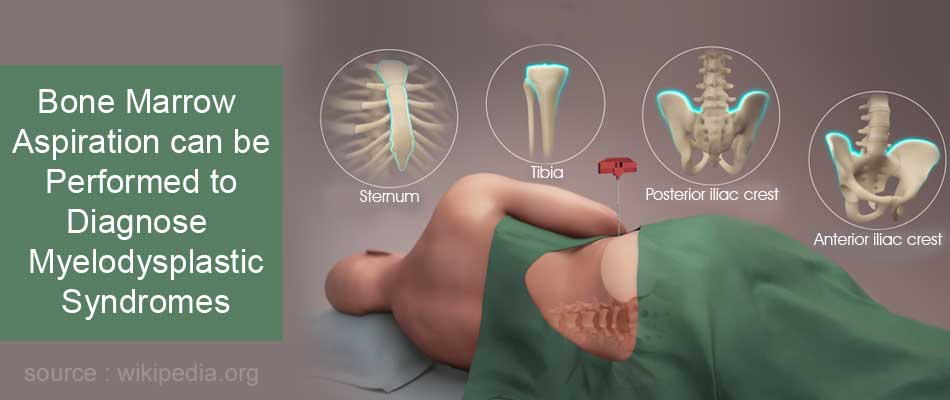
- Typically the bone marrow shows increased number of precursor cells (hypercellularity), although it may rarely be hypocellular.
- Abnormal forms of RBC precursors include megaloblasts (abnormally large red cell precursors), and ringed sideroblasts (RBC precursors with increased iron content).
- Platelet precursors may be small (micro-megakaryocytes), mononuclear megakaryocytes, and megakaryocytes with dumbbell shaped nuclei.
- Neutrophil precursors show nuclear abnormalities. The precursors are predominantly immature precursors with a failure to mature as shown by decreased numbers of maturing forms in the marrow.
Bone marrow biopsy
Alongside a bone marrow aspirate, a piece of bone may also be removed (bone marrow biopsy) and examined to assess for any abnormality.
Bone marrow biopsy is useful when the aspirate is dry and shows scant cells (hypocellular). It is thus useful in making a diagnosis of hypoplastic or fibrotic MDS. In addition, a bone marrow biopsy may show evidence of fibrosis and carry prognostic value.
Cytogenetics
Clonal chromosomal abnormalities are noted in about 70% of the cases at diagnosis depending on the subtype and whether it is primary or secondary MDS. Even in those patients with a normal clonal karyotype at diagnosis, abnormal clones can develop during the course of the disease usually indicating a graver outcome.
There are several cytogenetic abnormalities associated with MDS that affect the outcome of the disease in different ways. Some of the common abnormalities include −7 or del(7q), −5 or del(5q), i(17q) or t(17p), −13 or del(13q), and del(11q).
Cytogenetic abnormalities carry the highest prognostic weight as per the Revised-IPSS.
How do you Treat Myelodysplastic Syndromes?
The management of MDS varies depending on the IPSS risk score, degree of cytopenias, type of cytogenetic abnormality and degree of immature precursors. High risk MDS necessitates more aggressive management.
- The treatment of MDS aims to combat the symptoms of cytopenias by supportive management. This may be the preferred line of treatment in low risk MDS with less chance for progression to AML.
- Medications are given that promote maturation of the immature precursors.
- In some cases immunosuppressive agents are prescribed.
- Certain MDS with specific cytogenetic abnormalities are managed differently.
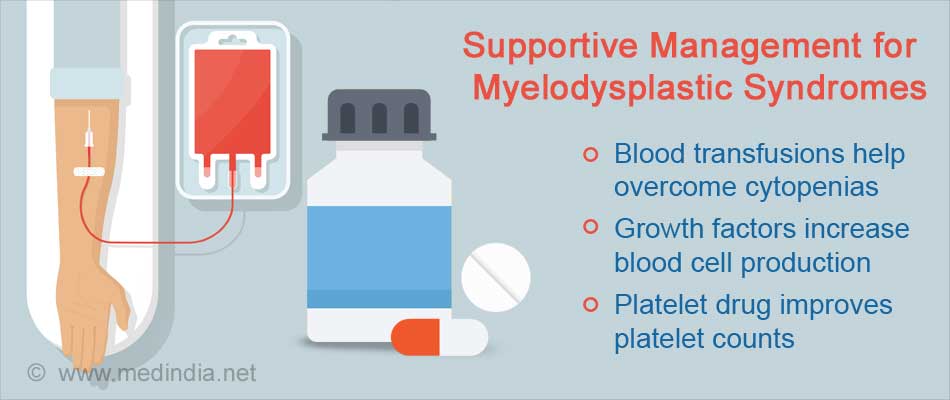
Supportive management
- Blood transfusions may be given on a regular basis to overcome the cytopenias.
- Medications called growth factors are given to increase the production of blood cells. Epoetin alfa (Epogen) or Darbepoetin alfa (Aranesp), decrease the need for blood transfusions by increasing red blood cell formation.
- Another medication called granulocyte-colony stimulating factor (G-CSF) is given to increase white cell production in certain types of MDS.
- Prophylactic antibiotics are prescribed in some cases with recurrent infections.
- For low platelet counts medications to improve platelet counts or platelet transfusions may be given as appropriate.
Medications to promote maturation of immature precursors
Medications such as Azacitidine (Vidaza) and Decitabine (Dacogen) reduce the risk of progression to acute myelogenous leukemia and may improve the quality of life of people with certain types of MDS.
Treatment in 5q deletion cases
If there is isolated del(5q) associated MDS, the doctor may recommend Lenalidomide (Revlimid). Lenalidomide decreases need for blood transfusion in these patients.
Bone marrow transplant
Allogeneic bone marrow transplant might be considered as an option in high risk MDS as the only potentially curative measure. All high risk MDS patients less than 70 years should undergo evaluation and HLA typing and matching with a suitable donor preferably a sibling or a suitably matched unrelated donor.
The major argument against bone marrow transplant in the elderly patients would be nderlying co-morbidities and the state of their general health.
What is the Prognosis of Myelodysplastic Syndromes?
The prognosis of MDS is determined in each case by analyzing pre-defined parameters and assigning a score to it. Based on the scoring system, MDS is classified into 5 risk groups, namely, very low, low, intermediate, high and very high risk with clear differences in the rate of progression to AML and overall survival.
For treatment purposes, IPSS low and intermediate-1 patients are generally considered ‘lower risk’ MDS, and intermediate-2 and high-risk patients are ‘higher risk’ MDS.
The parameters assessed in the scoring system include bone marrow cytogenetics, marrow blast percentage, and degree of cytopenias.
Patient age, performance status, serum ferritin, and lactate dehydrogenase are important additional features for survival but not for transformation into AML.
Patients with MDS-RARS have an overall better prognosis. Primary MDS types are easier to treat and carry a better prognosis.