- Gynaecological Cancer Leaflets - (https://eveappeal.org.uk/supporting-you/gynaecological-cancer-leaflets/)
- Inside Knowledge Fact Sheets - (https://www.cdc.gov/cancer/knowledge/publications/fact_sheets.htm)
What are Gynecologic Cancers?
Gynecologic cancers are cancers arising from the organs of the female reproductive tract. These include the uterus, ovary, cervix, vulva and vagina.
It is estimated that every year in the US alone, nearly 90,000 women are diagnosed with gynecologic cancer and nearly 30,000 die from the disease. Although all women are at risk of developing gynecologic cancer, the risk increases with age.
It is important that every woman is aware and is able to recognize signs and symptoms which may be suggestive of gynecologic cancer and seek immediate medical advice for the same.
Like all cancers, early diagnosis and treatment offer a better chance of cure.
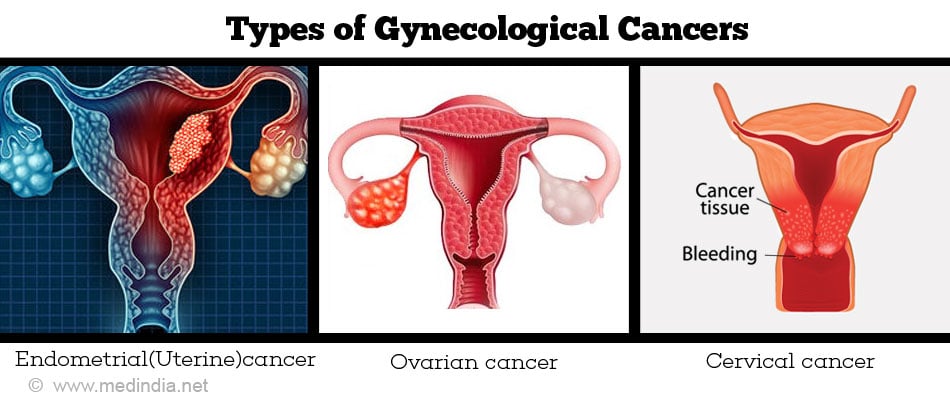
What are the Types of Gynecologic Cancers?
The five types of gynecologic cancer include the following:
1. Uterine or womb cancer – Arises from the lining of the uterus (endometrium), the pear shaped organ in which the baby grows.
2. Ovarian cancer – Begins in the ovaries, which are 2 in number and which are tiny almond shaped organs located on either side of the uterus.
3. Cervical cancer – It is also termed cancer cervix and is the lower part of the uterus.
4. Vaginal cancer – This cancer arises from the vagina, the hollow tubular organ that connects the cervix to the outside of the body. It is also referred to as the birth canal.
5. Vulval cancer – The vulva forms part of the woman’s external genitalia and includes the inner and outer lips of the vagina, the clitoris, and the opening of the vagina and its glands.
What are the Risk Factors of Gynecological Cancer?
| Cancer Type | Risk factors |
| Cervical cancer |
|
| Uterine cancer |
|
| Ovarian cancer |
|
| Vulvar cancer |
|
| Vaginal cancer |
|
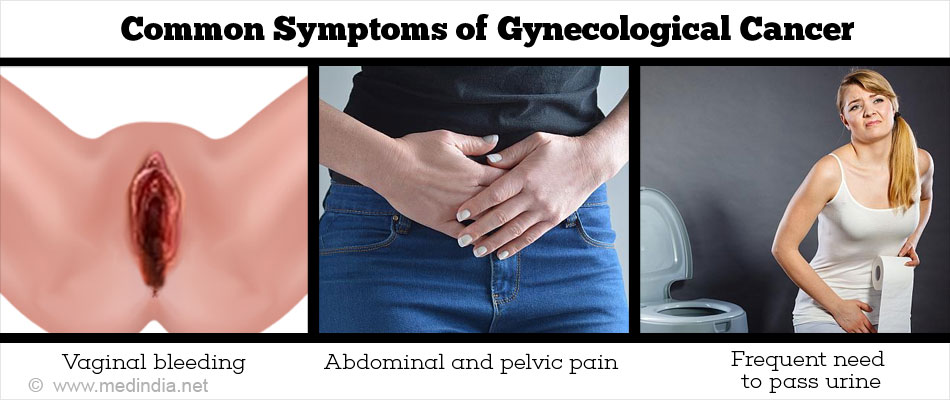
What are the Common Symptoms of Gynecologic Cancer that Women Should Know About?
| Cancer Type | Clinical features |
| Cervical cancer |
|
| Uterine cancer |
|
| Ovarian cancer |
|
| Vulvar cancer |
|
| Vaginal cancer |
|
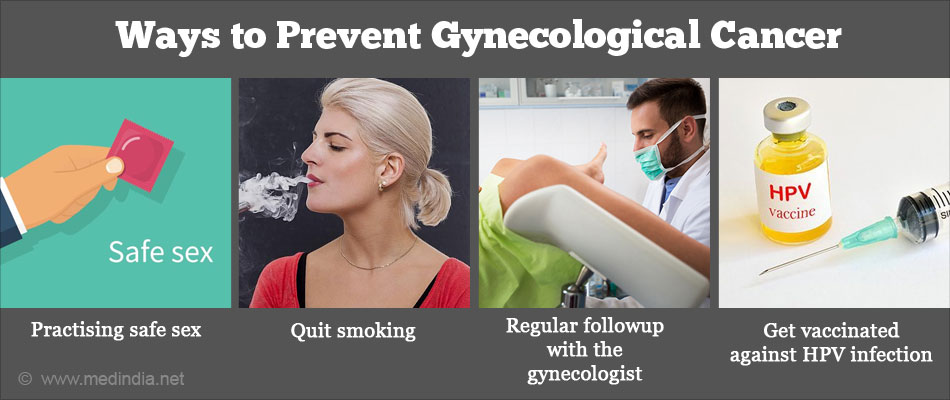
What are the Ways to Prevent Gynecologic Cancer or Early Detection?
| Cancer Type | Methods of Prevention |
| Cervical cancer |
|
| Uterine Cancer | There is no method known to prevent uterine cancer. However you can reduce your risk by the following measures:
|
| Ovarian Cancer | Seek immediate medical attention if –
|
| Vulvar Cancer and Vaginal Cancer | Protect from HPV infection by practising safe sex, and limiting number of sexual partners HPV vaccine of all girls aged 9-11 years; if you are older consult your doctor for further advice Quit smoking |
Tips to Take Charge of Your Health when You Have Gynecologic Cancer
The following measures will help to ensure that you receive optimal treatment associated with a better outcome and longterm prognosis.
Ensuring Referral to a Gynecologic Oncologist
If a woman is suspected to have gynecologic cancer, she should immediately be referred to a gynecologic oncologist. A gynecologic oncologist is an obstetrician/gynecologist who has specialized in the diagnosis and treatment of cancers of the female reproductive system, such as cervical, ovarian, uterine, vaginal and vulvar cancers.
With a gynecologic oncologist, the woman and her family can be confident of receiving the most optimal treatment that includes performing accurate staging surgery, debulking surgery to remove tumors that have spread to the abdomen and pelvis, knowledge of administering chemotherapy and radiotherapy, taking into consideration the woman’s concerns on sexual life and childbearing, and her emotional and physical well-being.
Studies indicate that patients treated by gynecologic oncologists have a better outcome when compared to patients not treated by cancer specialists.
Addressing Concerns Regarding Fertility and Emotional Issues
The woman should feel free to discuss fertility preserving options, sperm banks, referral to reproductive endocrinologists, and adoption agencies.
The woman and her family should enquire about availability of a psychologist to address their emotional needs and spiritual support and resources available. Ask about availability of financial help if needed.
Choosing the Right Center for Treatment
When choosing the center to undergo treatment, it is essential to choose a hospital where specialist gynecologic oncologists and their team are available and the center handles a good volume of gynecologic cancer patients. The center should have facilities to address the emotional and mental issues of the patient and her family as well such as psychotherapy and counseling.
Knowing the Disease Stage
Staging systems are clinically used to assess the severity of an ongoing cancer and generally divided into four stages. The first stage refers to the early phases of the disease, when malignant cells occur in a relatively limited region and are easy to treat, while the fourth stage denotes a very advanced condition in which cancerous cells have spread to adjacent organs and tissues and are more challenging to treat.
The treatment modalities offered will vary depending on the stage of the cancer and the patient’s condition.
Knowing about Treatment Options Available
The various treatment options available include surgery chemotherapy, radiotherapy and immunotherapy. The ideal treatment options or treatment combinations will vary for each patient depending on the stage of the disease and other considerations. You should discuss with your doctor about the expected duration of treatment, and the possible side effects.
Surgery is done in early stages to remove the tumor and adjacent lymph nodes; in later stages, debulking surgery is performed to reduce tumor burden when cancer has spread to other organs and sites.
Chemotherapy involves administration of drugs that kill cancer cells. Chemotherapy may be given before or after surgery depending on each case. Chemotherapy is associated with side effects such as nausea, vomiting, hair loss, and decreased immunity with increased susceptibility to infections. Your doctor will discuss these with you.
Radiotherapy involves administration of radiation either externally (external radiotherapy), or internally called intracavitary brachytherapy/radiotherapy (administering radiation into the body cavity such as vagina). Brachytherapy or internal radiation therapy, enables giving a higher total dose of radiation to treat a smaller area and in a shorter time than is possible with external beam radiotherapy. In interstitial radiotherapy, radiation needles are placed directly into the cancer and surrounding tissues.
Latest modalities in gynecologic cancer treatment include immunotherapy where immunotherapeutic agents are given to activate the body’s immunity to fight the tumor; immunotherapy also works by reversing tumor immunosuppressive mechanisms that have enabled the tumor to escape - the tumors can then be overcome by the patient’s immune system.
Learning How the Prognosis or Outcome is Determined
The prognosis is determined by evaluating the results of various tests such as biopsies, ultrasounds or PET-CT scans that determine the size, extent, genetic makeup, degree of spread and the aggressiveness of the tumor. Other factors taken into consideration include the age, overall health condition and fitness of the patient.
Health Tips
- Be aware of and recognize symptoms and signs of gynecologic cancer and seek prompt medical attention
- Protect yourself from HPV infection by practising safe sex (using condoms) and limiting number of sexual partners
- Consult your gynecologist regarding HPV vaccine
- Get regular Pap smears if you are between the age of 21-65 years
- Maintain a healthy weight and exercise regularly
- Eat healthy and sleep well
- Avoid smoking
- If you have a family history of gynecologic cancer, consult a gynecologist to learn about precautions to take to prevent gynecologic cancer









