- Cystic Fibrosis: Prenatal Screening and Diagnosis - (http://www.acog.org/~/media/For%20Patients/faq171.pdf)
- How Is Cystic Fibrosis Diagnosed? - (https://www.nhlbi.nih.gov/health/health-topics/topics/cf/diagnosis)
What is Cystic Fibrosis?
Cystic Fibrosis is a genetic disorder caused by CFTR genetic mutation. Symptoms include accumulation of sticky mucus in the lungs and excessively salty sweat. Cystic Fibrosis has no cure but can be managed symptomatically.
It was first described by American doctor Dorothy Andersen in 1938.
Cystic fibrosis (CF) is an inherited or genetic disease involving the secretory glands, such as the mucus and sweat glands. People with the disease inherit mutant CFTR genes from parents who may not have the disease themselves.
The World Health Organization statistics show that "In the European Union, 1 in 2000–3000 newborns is found to be affected by CF" In the United States, 1 in 3,500 children are born with CF.
In 1997, about 1 in 3,300 Caucasian children in the United States were born with cystic fibrosis. In contrast, only 1 in 15,000 African American children suffered from cystic fibrosis, and in Asian Americans the rate was even lower at 1 in 32,000.
The prevalence of CF in the Indian subcontinent is not clearly known but may vary from 1 in 10,000 to 1 in 40,000. The issue is complicated by the fact that facilities for diagnosis and testing are not widely available. At least some of the infants dying of pneumonia and/or malnutrition may be suffering from CF going unrecognized.
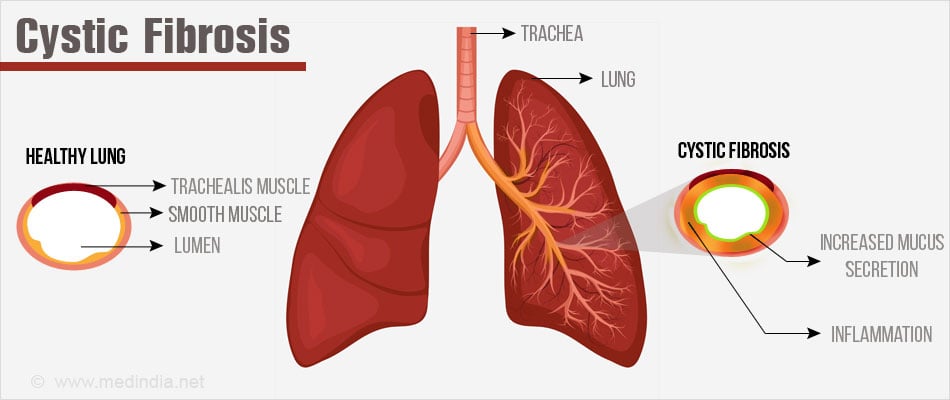
Mucus is a slippery, watery substance, secreted by the tissue that lines certain organs, keeping them moist and preventing infections.
In CF patients, thick, sticky mucus accumulates in the lungs and acts like a plug to blocks the air passages. This mucus also creates an ideal ambience for excessive bacterial growth, which leads to frequent infections that eventually damage the lung.
CF mostly affects the sinuses, pancreas, lungs, liver, intestines and the sex organs. It does not affect the brain.
In people with CF the decline of lung function sets in during childhood. Over time the lungs are irreversibly damaged and breathing becomes severely laborious
Another feature is the salty sweat of the CF patients. There is excessive salt loss which results in mineral imbalance which in turn leads to a number of health problems including dehydration.
What is the Cause of Cystic Fibrosis?
As mentioned previously CF occurs due to mutation of a gene on chromosome 7 called the Cystic Fibrosis Transmembrane conductance Regulator (CFTR). This gene regulates transport of chloride ions in and out of cells. The normal transport of chloride ions ensures formation of thin, freely flowing mucus. As a result of the faulty gene, chloride transport is disrupted and mucus becomes unusually thick and sticky. This leads to the distinctive signs and symptoms of the disease.
Genetics of Cystic Fibrosis
The mutation in the CFTR (cystic fibrosis trans-membrane regulator) gene produces a protein that controls the transport of chloride ions and water across the cellular membranes. Hence the name CFTR gene / protein.
CFTR protein is found to be present in cells lining the organs such as lungs, pancreas, colon and the uro-genital tract. In CF-affected individuals, the aberrant gene in turn makes a faulty protein whose function is impaired.
Scientists assert that the CFTR protein affects other body functions too which explains the other symptoms and complications associated with CF.
The CFTR gene is known to be impaired in several different ways in the affected persons and the type of defect is known to influence the severity of the disease in a person. The most common error is the loss of 3 base pairs from the CFTR gene resulting in the loss of an amino acid, phenylalanine, in the protein formed. However, this type of mutation accounts for only 70-80% of CF cases.
Other genes have also been discovered that play a role in disease progression.
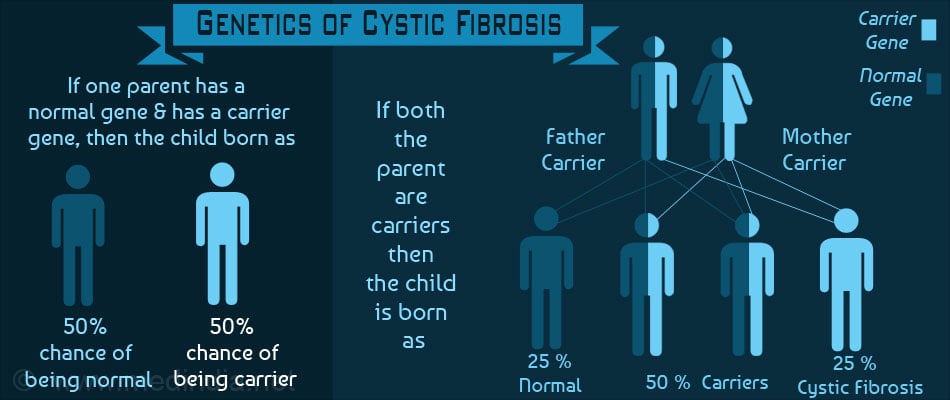
Being an autosomal recessive condition, both copies of the gene (one from each parent) have to be faulty for the disease to become manifest clinically.
It goes without saying that both parents have one defective copy of the gene each. They are termed ‘carriers, but are clinically normal. They can however pass the faulty gene to their offspring.
If one parent has normal CFTR genes and another is a ‘carrier’ then each child born has a -
- 50% chance of being normal, and
- 50% chance of being a carrier
If both parents are ‘carriers’ the following is the hereditary pattern. Each child has a -
- 25 % chance of inheriting two normal CFTR genes (normal)
- 50 % chance of inheriting one normal CFTR gene and one faulty CFTR genes (carriers)
- 25 % chance of inheriting two faulty CFTR genes (cystic fibrosis)
With advances in modern medicine, tests are available to detect carriers and offer them genetic counselling.
What are the Symptoms and Signs of Cystic Fibrosis?
The severity of the symptoms of Cystic Fibrosis (CF) varies between individuals. In some CF is very severe and manifests in early childhood while in others the disease is mild and does not reveal itself until adolescence or early adulthood sets in.
The symptoms of CF can vary between mild and severe, with time. As the disease progresses, the severity of the disease increases too.
The first signs of cystic fibrosis may be detected by the parents who, on kissing the baby, discover that the baby's skin tastes salty. Another evidence appears when the new born baby does not pass stool due to an intestinal block common to babies with CF.
Toddlers may present with frequent respiratory infections, wheeze and cough. Involvement of pancreas may present as passing greasy and fatty stools (steatorrhea), and or failure to thrive.
Most of the symptoms and signs will eventually appear by adolescence, some of which are listed below -
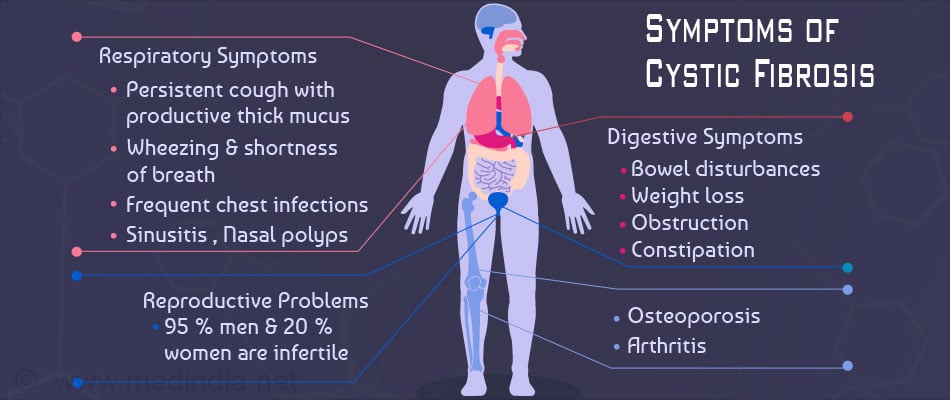
a) Respiratory:
- Chronic, persistent cough with production of thick viscid sputum
- Breathlessness and wheeze
- Frequent respiratory tract infections
- Frequent nasal block and stuffy nose
- Intolerance to exercise
b) Digestive:
- Failure to gain weight or thrive among infants and toddlers
- Foul smelling greasy stools
- Newborns may have a condition called Meconium ileus that leads to intestinal obstruction
- Constipation
c) Other Signs
- Salty Sweat
What are the Complications of Cystic Fibrosis?
Complications occur in long standing cases of cystic fibrosis due to organ damage. The complications are most often seen in the organs primarily affected by the disease.
Respiratory System
- Recurrent attacks of bronchitis and pneumonia
- Damage to the airways resulting in a condition called bronchiectasis.
- Nasal polyps that cause difficulty in breathing.
- Coughing of blood or hemoptysis due to thinning of the airways.
- Pneumothorax (collection of air in the pleural cavity surrounding the lungs).
- Respiratory failure due to severe lung tissue damage.
Digestive System
- Malabsorption of nutrients due to lack of pancreatic enzymes. This in turn leads to nutritional deficiencies.
- Diabetes mellitus due to pancreatic damage.
- Blockage of bile duct (tube connecting the liver and small intestine) leading to gallstones and liver disease.
- Intestinal obstruction and a higher risk for intussusception.
- Distal intestinal obstruction syndrome (DIOS) - a partial or total obstruction occurring at the region where the small intestine ends and the large intestine begins.
Reproductive System
- Infertility in men due to blocked or absent vas deferens (tube connecting the testis and prostate), a common occurrence in CF.
- Infertility in women (not as common as in men) due to cervix containing thick mucus making it difficult for sperm to swim through.
- Pregnancy may exacerbate the clinical features of the disease and cause complications.
Other Systems
- Increased risk of osteoporosis
- Dehydration and electrolyte imbalance due to loss of minerals in sweat
- Clubbing of fingers and toes.
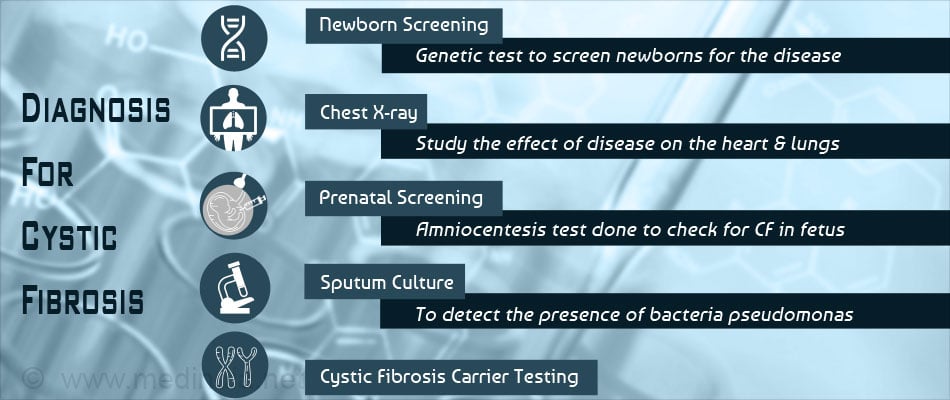
How is Cystic Fibrosis Diagnosed?
Cystic fibrosis may be diagnosed at any age. Carrier couples may want to get the fetus tested during pregnancy and others can get themselves tested before they plan a pregnancy.
Newborns, infants and young children can be tested for cystic fibrosis if there is a positive family history or a clinical suspicion.
The tests may be screening tests such as immunoreactive trypsinogen (IRT) test or confirmatory tests such as genetic testing and sweat test.
1. Testing the Fetus – Prenatal Diagnosis
This is usually carried out when both the parents are carriers of the faulty CFTR gene. In such a scenario, the baby has a 25% chance of suffering from CF. Parents may want to know if the child will inherit the disease so that they could plan for the care of a child with special health needs. Some couples may decide to end the pregnancy.
Chorionic villus sampling or amniocentesis can be done to detect the presence of the disease in the fetus. Chorionic villus sampling is usually done after 9 weeks of pregnancy. Amniocentesis is carried out between 15 – 20 weeks of pregnancy.
2. Newborn Screening
Newborns may be screened for high levels of immunoreactive trypsinogen (IRT) in their blood. High levels suggest a diagnosis of CF. Further genetic testing and sweat testing are necessary to confirm the diagnosis.
Sweat testing is done when the infant is about a month old to ensure adequate sampling. The test measures the salt content of the sweat. It is high in carriers as well as sufferers of the disease. A sweat test can detect if the infant has the disease or is a carrier of the CFTR gene.
The test is repeated on two separate occasions in a specialised center.
Genetic testing on newborn may be done on the blood sample to check for the presence of the faulty CFTR gene. If both genes are faulty, the baby has the disease. If one gene is faulty, then the baby is a carrier.
If both genes are faulty, then a single sweat chloride may be sufficient to confirm the diagnosis.
3. Screening of Older Children or Adults
A CF sweat test or genetic testing may be recommended if they suffer from recurrent infections, failure to gain weight, nasal polyps, sinusitis or infertility.
Another test namely the nasal potential difference test may be done to determine the flow of salts in and out of the cells lining the nose.
4. Other Tests to Monitor the Disease
- Lung function tests
- Throat or sputum culture to determine the type of microbes causing infection
- Chest x-ray to inspect the status of the lungs
- CT scan of lungs, pancreas and other organs to look for evidence of serious disease
- Blood sugar levels and liver function tests
- Stool fat analysis
- Arterial blood gas analysis to determine how well the lungs are functioning
How do you Treat Cystic Fibrosis?
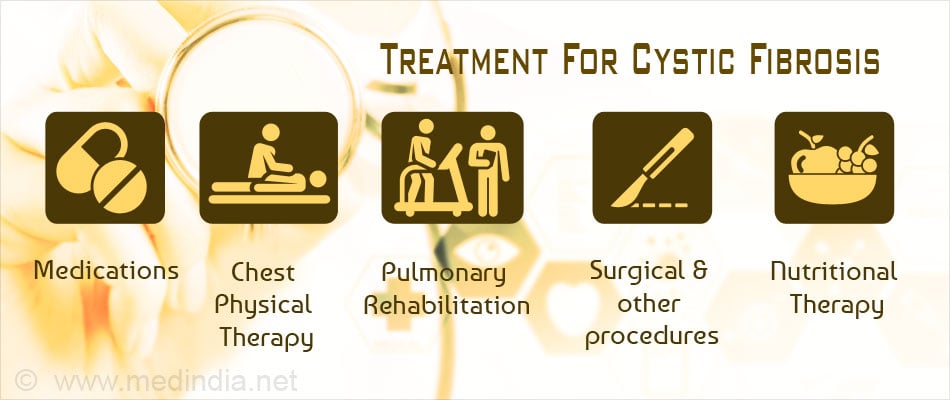
At present there is no cure for CF. Treatment aims at alleviating the symptoms and reducing the incidence of complications. Careful follow up and early and aggressive intervention is essential. It is advisable to obtain treatment at a center that specializes in CF.
Aims of Treatment
- Reducing incidence and successful treatment of respiratory infections
- Providing sufficient nutrition
- Removal of and loosening mucus plugs in lung and airways
- Avoiding and treating intestinal obstruction
a) Chest Physical Therapy
Done to loosen the thick mucus and aid expectoration. It is done by tapping the front and back of the chest with cupped hands. May be done up to four times a day depending on severity. This can be done with the patient sitting or, lying on his abdomen. Breathing exercises too can loosen the phlegm and help to relax.
‘Chest Clapping’ or percussion: It involves pounding the patient’s chest with hands, or with devices such as electric chest clapper or a vibrating vest, to release the accumulated mucus from the lungs so that the patient can cough it out.
Exercise
Aerobic exercises too help to loosen the mucus and to improve the general physical condition. But while exercising, a lot of salty sweat is generated which leads to a loss of salt and minerals from the body. This can be countered by taking a high-salt diet.
Medications
Medications to prevent or treat infections and inflammations, to open the airways and to thin mucus are usually administered. These drugs include antibiotics, anti-inflammatory medicines, bronchodilators or mucus-thinning medicines and they are usually administered orally or intravenous methods. Inhaled antibiotics are used to treat infections caused by the bacteria Pseudomonas.
b) Digestive Problems
Nutritional therapy can take care of the malnutrition and vitamin deficiency that is common to CF patients. It involves -
- Taking a well-balanced diet
- Intake of oral pancreatic enzymes to help in digestion and absorption
- Vitamin A, D, E, and K supplements
- High-calorie nutrient-filled shakes
- A high-salt diet or salt supplements usually taken before exercise
- A feeding tube may also be used in the night to give more calories
Some children with CF might present with celiac disease. In children with failure to thrive due to malabsorption it is advised to screen for serum antigliadlin. Gluten based diet should be avoided in such cases. Some develop diabetes and require different diet regimen.
Diet requires pancreatic enzyme supplementation, a high fat, high salt, and calorie dense diet helps with the child’s growth.
Digestive problems may also be treated with enemas and mucus-thinning medicines to remove intestinal blockages. In extreme cases a surgery may be required.
c) Diabetes and osteoporosis which are complications associated with cystic fibrosis are also treated with suitable medications.
Improved methods of treatment have contributed to increased life span of the affected individuals. The affected individuals are now living well into their forties and even fifties-a thing which was unheard of in the past.
Usual Medications used in CF
- Antibiotics for treating and preventing respiratory infections.
- Mucolytics (mucus thinning agents) that aid in coughing out the mucus. This helps in better lung function. Inhalation of hypertonic saline has been found to improve lung function and increase the hydration of airway surface liquid.
- Bronchodilators to keep the airways patent and facilitate easier breathing.
- Pancreatic enzyme supplements to improve absorption and digestion.
- Vitamin supplements including fat soluble vitamins A,D,E and K.
- Recently developed agents that improve chloride transport include Ivacaftor.
d) Surgical Treatment of Complications
- Removal of nasal polyps to overcome obstruction to breathing
- Removal of mucus obstructing the airways by suction via an endoscope
- Oxygen therapy if arterial oxygen saturation levels fall
- Alimentation through a feeding tube to improve the nutritional status
- Relieving intestinal obstruction caused by meconium ileus or intussusception
- Lung transplant if lung damage is severe with breathing difficulties and both lungs are affected.
Other measures to reduce infections and complications
- Regular handwashing before eating and after using the bathroom
- Regular exercise regimen
- Being up to date on immunizations including flu vaccines
- Avoid smoke inhalation which may damage lungs further
e) Gene Therapy - Much has been anticipated in terms of gene therapy as a cure for cystic fibrosis. However, it has still not been proven to be a cure. Scientists have taken nasal cells from CF patients and incorporated normal CFTR genes in them. The new gene has been able to produce the normal form of the CFTR protein too.
However, all this experimentation has been in vitro as a proper system to deliver the modified gene in vivo is still not in place. Besides it has been found that the cells into which the new gene is delivered find it difficult to assimilate the carrier molecule and to express the modified gene.
All these obstacles will have to be overcome for gene therapy to take off successfully. A lot of work is going on. Hopefully the day is not too far off when a complete cure is possible!
f) Recent Research - Scientists at the Perinatal and Pulmonary Biology at Cincinnati Children's Hospital Medical Center, USA, have discovered the basic mechanism or “switch” that controls excessive mucus production in lung diseases such CF, asthma and even the humble common cold.
Healthy lungs produce a fair amount of mucus (that are sugar–coated proteins) to get rid of contaminants and protect the body. In those with respiratory illnesses, the lungs get clogged, due to excessive mucus secretion and accumulation, the reason(s) for which is not clearly known. Understanding the underlying mechanism of this mucus hyper production could pave way to new treatment modalities.
Current studies have revealed that the beneficial Clara cells of the lungs transform to goblet cells, through a process called metaplasia, and cause excessive mucus production. Metaplasia has been found to be controlled by a specific genetic switch. Research has revealed that metaplasia can be reversed and that the goblet cells can even be reversed to Clara cells if the genetic switch is blocked. This information holds a lot of scope for future therapies.
The gene SPDEF has been discovered to be involved in normal mucus production in healthy lungs and other organs. An inflammatory response induced in experimental mice increased SPDEF expression dramatically in the lung tissue, resulting in the excessive production of thick mucus. Switching off the SPDEF gene in the mice lungs ensured that there was no inflammatory response or excess mucus production.
The discovery of this genetic ‘switch’ is bound to benefit scores of patients suffering from mucus hyper-production due to diseases such as cystic fibrosis. Although the work has been a breakthrough in mice it will be some years before it can be translated to a therapy for CF patients.
Scientists at the University of Pennsylvania School of Medicine have discovered that a dietary antioxidant thiocyanate, found in vegetables such as broccoli and cauliflower, can offer protection to cells from chemicals generated during the body's inflammatory response. This finding has special implications for inflammation-based disorders such as cystic fibrosis (CF), heart diseases, diabetes, and neurodegeneration. The study has been published in the Proceedings of the National Academy of Sciences.
Health tips
- If there is a history of CF in the family, get yourself tested for the presence of the faulty gene.
- If you or your partner is a carrier of the defective CFTR gene, consider genetic counselling and advice on prevention of the disease in the child before planning a pregnancy.
- It is recommended that parents of children suffering from CF join a support group. It will help in coping with your difficulties and fears when other children and parents share their experiences.