- Noonan Syndrome - (https://ghr.nlm.nih.gov/condition/noonan-syndrome)
- Noonan Syndrome - Rare Disease Database - (https://rarediseases.org/rare-diseases/noonan-syndrome/)
- Information About Noonan Syndrome - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4099190/)
- More Information About Noonan Syndrome - (https://www.ncbi.nlm.nih.gov/books/nbk1124/)
- About Noonan Syndrome - (https://www.genome.gov/genetic-disorders/noonan-syndrome)
- What is Noonan Syndrome? - (https://www.aafp.org/afp/2014/0101/p37.html)
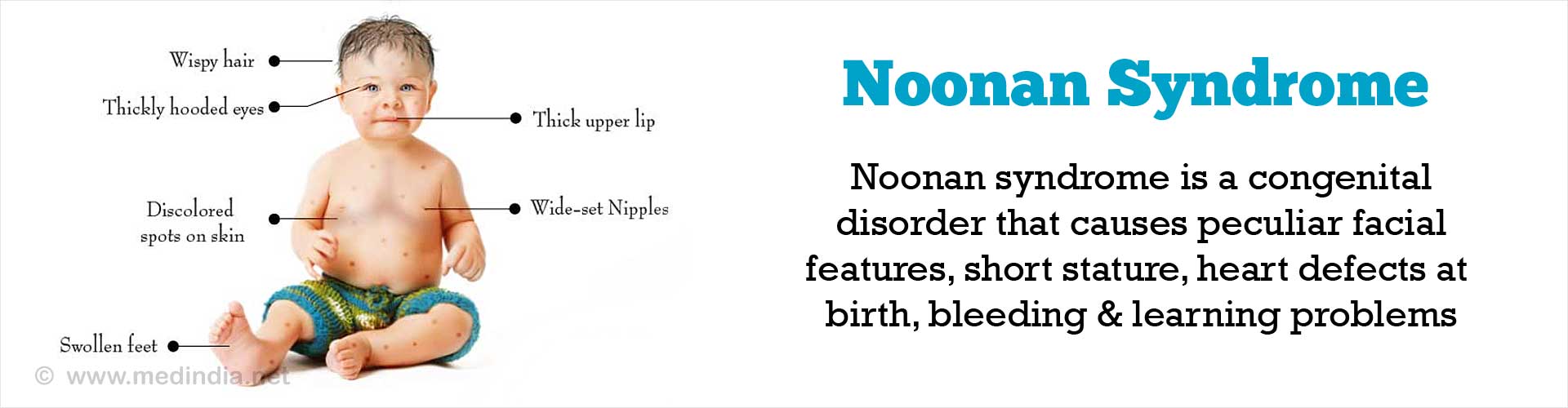
What is Noonan Syndrome?
Noonan syndrome is a congenital disorder that affects different parts of the body.
Heart defects at birth, peculiar facial features, short stature, bleeding problems, peculiar facial features, learning problems characterize it.(1✔ ✔Trusted Source
Noonan Syndrome
Go to source)
What are the Causes of Noonan Syndrome?
Noonan syndrome is caused by a defective gene that is usually inherited from one of the child’s parents. The most common genetic mutations associated with Noonan syndrome include PTPN11, SOS1, RAF1 and KRAS.(2✔ ✔Trusted Source
Noonan Syndrome - Rare Disease Database
Go to source)
What are the Symptoms of Noonan Syndrome?
Symptoms of Noonan syndrome may include the following:
- A characteristic facial appearance with features including webbed neck and a flat nose bridge (see the figure for a detailed list of features).
- Short stature- Approximately 50 to 70 percent of individuals with Noonan syndrome suffer from short stature. At birth, they are usually of normal length and weight, but as time passes, the growth slows down. Abnormally low levels of growth hormone may contribute to the short stature.
- Heart defect present at birth (congenital disorder)- The most common heart defect is a narrowing of the valve that directs the blood to the lungs from the heart, this is called pulmonary stenosis. Another condition is hypertrophic Cardiomyopathy where the heart muscles enlarge. Atrial and ventricular septal defects have been noted in some cases of Noonan syndrome that occur along with Downs syndrome.
- Learning disability occurs in 15-35%, but is usually mild and most children function well in schools. Verbal performance is more often affected and therefore, there is a requirement of speech therapy very frequently.
- Issues with the eyes such as strabismus or squint in up to 90 percent of people suffering the disease.
- Bleeding problems such as increased tendency to bleed from wounds, abnormal menstruation, nosebleeds, bruises or cuts which fail to heal.
- A varying shape of the chest with widely spaced and low set nipples called pectus excavatum. Problems in breathing due to structural alterations in the rib cartilage.
- Undescended testes in case of males, which may be related to delayed puberty or to infertility (inability to produce enough sperms to make a child) later in life. Adolescent males with Noonan syndrome typically experience a delay in the puberty. Males generally attain puberty by age 13 to 14 years. Affected females are spared from the issue of delayed puberty.
- Early milestones are often delayed, with low muscle tone and joint laxity contributing to a part of the motor system delay.
- The incidence of attention deficit hyperactivity disorder (ADHD) is reported to be higher in children with Noonan syndrome compared to the unaffected ones.(3✔ ✔Trusted Source
About Noonan Syndrome
Go to source)
How do you Diagnose Noonan Syndrome?
The basis of diagnosing Noonan Syndrome depends on prenatal and genetic karyotyping studies.
- About fifty percent of individuals with Noonan syndrome have mutations in the PTPN11 gene.
- Twenty percent of those with Noonan Syndrome have mutations in the SOS1gene.
- Mutations in the RAF1 gene occur in 10 to 15 percent of Noonan syndrome cases.
- About 5 percent of people with Noonan syndrome have mutations in the KRAS gene and these people usually have a more severe form of the disorder
- The remaining 10-15 percent of the cases doesn’t have an actual cause for the disease.(4✔ ✔Trusted Source
Information About Noonan Syndrome
Go to source)
How do you Treat Noonan Syndrome?
Management guidelines have been developed by an international guideline development group under the guidance of Noonan Syndrome Support Group (NSSG), and age-specific screening and testing is advised for certain problems.
Key recommendations of these guidelines cover all organ systems, which can be involved in the body:
- Genetic Counseling along with Follow-up for the Same: A positive genetic screening test confirms the diagnosis. However if it comes negative, it doesn’t rule out the diagnosis.
- Cardiovascular Problems: An expert cardiologist opinion should be taken, further followed by ECG and echocardiogram checking. Followed by a checkup of ejection fraction and certain after evaluation surgical or medical corrections, if any.(5✔ ✔Trusted Source
More Information About Noonan Syndrome
Go to source) - Growth and Endocrine System Problems: Children should be weighed and their heights measured and the same should be plotted on appropriate growth charts.
- Children with evidence of growth failure should have baseline investigations and nutrition correction by appropriate methods.
- Thyroid function tests and antibodies should be done in those with symptoms of hypothyroidism or a goiter.
- Children with delayed puberty should be referred to an endocrinologist for expert opinion.
- Therapeutic interventions as indicated - growth hormone treatment for growth failure, thyroxine for hypothyroidism, estrogen or testosterone for pubertal growth delays.
- Growth hormone has been successfully used in the treatment of short stature associated with Noonan syndrome.
- Problems with the Renal and Genitourinary System: Renal ultrasonography is mandatory, to diagnose undescended testes and corrective surgery for the same should be done at 1 year of age.
- Nutrition: Consultation for feeding difficulties or recurrent vomiting, with or without bile in the vomitus should be made as early as possible to prevent malnourishment
- Hematology: A complete blood count should be done to spot problems with the hematological system.
- Neurological, Cognitive and Behavioral Problems: Developmental screening annually with complete neuropsychological testing if the screening result is not satisfactory.
- Problems with the Eyes and Ears: A full eye checkup followed by a full audiology and speech checkup should be done.
- Orthopedic and Dental Problems: Annual examination of the chest and back should be done. Oral examination is done during each visit.
- Problems with the Lymphatic System: Those with peripheral lymphoedema should be referred to specialty lymphoedema clinics and associated hospitals.
- Risk while Undergoing Anesthesia: Individuals with Noonan syndrome are at an increased risk of malignant hyperthermia when receiving general anesthesia compared to the unaffected ones, and certain anesthetic agents need to be stopped and avoided.(6✔ ✔Trusted Source
What is Noonan Syndrome?
Go to source)