- Post Traumatic Stress Disorder - (http://www.nhs.uk/conditions/post-traumatic-stress-disorder/pages/introduction.aspx)
- Information on PTSD - (https://www.adaa.org/sites/default/files/adaa_ptsd.pdf)
- What is PTSD? - (http://www.apa.org/topics/ptsd/)
- PTSD - Risk Factors - (https://en.wikipedia.org/wiki/posttraumatic_stress_disorder#risk_factors)
- PTSD Fact Sheet - (http://www.dsm5.org/documents/ptsd%20fact%20sheet.pdf)
- PTSD Treatment Grow in Evidence - (http://www.apa.org/monitor/jan08/ptsd.aspx)
- FAQs about PTSD - (https://bbrfoundation.org/frequently-asked-questions-about-post-traumatic-stress-disorder-ptsd)
- Management of PTSD - (https://www.ncbi.nlm.nih.gov/books/nbk56494/pdf/bookshelf_nbk56494.pdf)
- Epidemiology of PTSD - (http://www.ptsd.va.gov/professional/ptsd-overview/epidemiological-facts-ptsd.asp)
- PTSD - A Growing Epidemic - (https://medlineplus.gov/magazine/issues/winter09/articles/winter09pg10-14.html)
What is Post-Traumatic Stress Disorder (PTSD)?
Post traumatic stress disorder (PTSD) is an anxiety disorder that occurs in people who have experienced or witnessed a traumatic event such as a crime, accident, natural calamity, sexual assault or domestic violence.
People who experience personal events like sexual assaults, domestic violence or a death of a loved one are more likely to develop PTSD than people who face events like accidents or natural disasters.
Victims experience recurrent flashbacks of the event.
The lingering and debilitating stress that occurs due to the illness can cause a series of psychological and biological changes like acute stress, anxiety, fear and panic in the victims.

Fear for life and a sense of acute danger develops because the event gets etched in their memory, haunting them incessantly. Victims are unable to lead a normal life.
Post-Traumatic Stress Disorder was formally recognized as a mental disorder after the famous Vietnam War, where soldiers appeared to be in ‘shell shock’ even after they left the war zone, fearfully recalling the trauma of combat, and unable to adjust to life afterwards.
Facts and Statistics about PTSD:
- Currently 260 million people worldwide suffer from PTSD.
- The average age of occurrence of PTSD is 23 years.
- In the U.S., 7.7 million people 18 years and older have PTSD.
- There is a lifetime prevalence of 7.8% of an American experiencing PTSD with women twice as likely to develop it (10.4) as compared to men (5%).
- In a given year, 3.6% of American adults between ages 18 and 54 (5.2 million people) are affected by PTSD.
- The one-month prevalence range using 2 different diagnostic tools are 1.5-1.8% and 3.4%.
- Mass violence causes PTSD at a much higher rate (67% of people exposed to it) than those exposed to natural disasters or other types of traumatic events.
- Children and adolescents are less likely to acquire PTSD (1%) than adults (1.5-3%) in non-war torn areas in developed countries. The percentage is lesser if they are less than 10 years old.
- 16% of children exposed to trauma develop PTSD depending on type and gender.
- PTSD shares 60% of the same genetic variance with panic and generalized anxiety disorder (GAD) and 40% with alcohol, nicotine and drug dependence.
- Among Americans PTSD afflicts 31 percent of Vietnam veterans, 10% of Gulf War veterans, 6% to 11% of Afghanistan veterans and 12 to 20% of those who served in Iraq.
- The estimated annual cost to the American society due to anxiety disorders is above $42.3 billion. This high rate is attributed to misdiagnosis and under treatment.
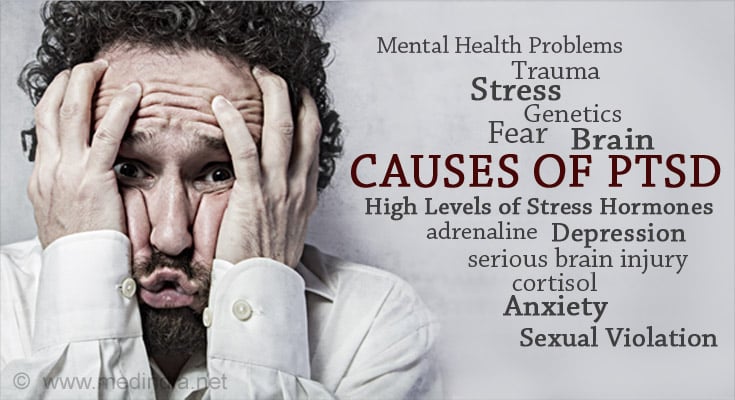
What are the Causes of PTSD?
People develop PTSD when they either experience or witness or learn about an event involving actual or threatened death, serious injury or sexual violation.
Like most mental health problems which do not have just one cause, PTSD is probably caused by a complex mix of:
- Inherited mental health risks, such as an increased risk of anxiety and depression.
- Life experiences, including the amount and severity of trauma dealt with since early childhood.
- Differences in the way the brain responds to stress by releasing certain chemicals and hormones. Brain scans reveal differences in the emotional processing centers of the brain.
- Genes that play a role in creating fear memories.
- Temperament or the nature of the person.
- Exposure to a severe, long-lasting traumatic event.
- Elevated levels of stress hormones like adrenaline under normal conditions even in the absence of threat. This may be responsible for the numbed emotions and the hyperarousal they constantly feel. Recalling their trauma, adrenaline is activated causing them more fear, stress and discomfort.
- Alterations in the levels of cortisol, another hormone that is released during this time to counter stress in the body. In case enough cortisol is not released, to put off the stress reaction, the effects of stress may continue to linger.
- A genetically smaller hippocampus (responsible for memory and emotions) might be related to the fear and anxiety, memory problems and flashbacks that occur with PTSD.
What are the Symptoms of PTSD?
Symptoms of PTSD can begin within 3 months after the stressful event has occurred or several years after the event.
Symptoms must last for more than a month
Symptoms are stronger when faced with a similar situation that remind the person of the event.
In Acute Stress Disorder or ASD - the symptoms immediately follow the experience of a traumatic event and lasts for a few weeks. It can seriously affect one’s ability to function and the symptoms are only due to the event and not due to any other reason like substance abuse.
In Chronic Stress Disorder or CSD the symptoms do not start for weeks or months and are associated with depression, substance abuse or other anxiety disorders.
There are four categories of symptoms:
Re-experiencing or Intrusive Symptoms:
- Consciously or subconsciously re-living the event either as recurring thoughts and memories, flashbacks or nightmares. Words, objects or situations can trigger these thoughts.
- Reacting emotionally or physically when reminded of the event.
- Experiencing physical symptoms like a racing heart or sweating.
Avoidance Symptoms:
- Avoiding thinking, feeling and talking about the traumatic event.
- Not going to similar places and events, not doing similar activities, and not meeting the same people involved in the event.
- For example, a person will avoid driving a car if the event had been a bad car accident.
Mood-based Symptoms Like Emotional Aloofness or Detachment:
- Having negative thoughts about themselves and others (in other words, not being capable of experiencing positive emotions).
- Feeling emotionally numb and hopeless about the future.
- Becoming isolated and withdrawn from friends and family.
- Not enjoying previously interested activities.
- Having memory issues.
- Having difficulty maintaining close relationships.
- Forgetting key features of the event.
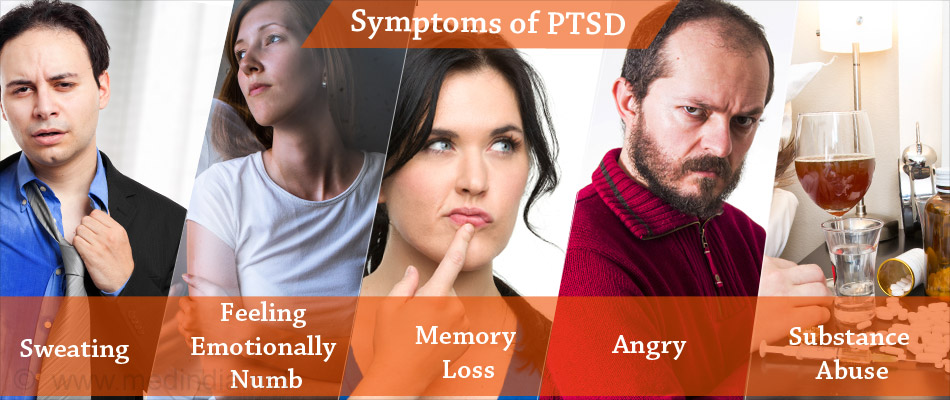
Reactivity and Arousal Symptoms:
- Always being in a state of alert and in anticipation of danger.
- Increased stress affecting concentration, eating and sleep.
- Overwhelming guilt and shame about the event; blaming themselves for it.
- Self-destructive behavior like alcohol and substance abuse.
- Easily startled or frightened, being on guard always; feeling jumpy or tense, always “on edge”.
- Feeling irritable, angry, aggressive or stressed.
What are the Symptoms of PTSD in Children?
A personal trauma like sexual abuse or extreme physical abuse can cause children to develop symptoms of post-traumatic stress disorder.
Intense personal trauma can damage a child’s psyche.
Children who face personal trauma have a tendency to internalize their feelings, experience guilt and even blame themselves for what has happened. This can lead to negative self-image and hamper their mental development gravely. They may be unable to develop social relationships and forge bonds.
A whopping 3 million children are exposed to domestic violence each year in the United States. Close to 5 million children face trauma every year in the United States- this translates into 1.8 million new cases of post-traumatic stress disorder each year.
If the following symptoms of PTSD in children lasts for more than a month, they may signal the need for medical care.
- Re-enacting the traumatic event through play.
- Bedwetting
- Not talking about the event or their feelings about it.
- Generalized fear.
- Sleep disturbances, nightmares that may even not relate to the event.
- Confusion.
- Heightened arousal or edginess.
- Separation anxiety (especially from a parent or adult).
- Loss of speech or motor skills.
- Stomach aches and headaches.
- Hyperactive starter reflex.
- Losing interest in activities previously enjoyed.
- Personality changes, mood changes.
- Withdrawal.
- Undue concern and worry.
- Extreme self- consciousness.
- Aggressive behaviors and angry outbursts.

What are the Risk Factors of PTSD?
Everyone experiences PTSD at least once in their lifetime. While men are more exposed to scenarios that put them at risk, women who experience trauma are more affected by it.
Who are the People at Risk?
- Military personnel exposed to war/combat and their family members.
- Victims of natural disorders and violent crimes.
- Concentration camp survivors.
- First responders like police officers, fire-fighters, ambulance and healthcare professionals.
- People who work as train drivers, divers, journalists and sailors.
- People who work in banks, post offices and in stores.
What are the Common Events that Put you at Risk to Develop PTSD?
- Military combat exposure.
- Natural calamities like severe floods, earthquakes or tsunamis.
- Unnatural events like car and plane crash.
- Life-threatening medical diagnosis.
- Terrorist attacks.
- Violent personal assaults like mugging, being threatened with a weapon and sexual assaults.
- Childhood neglect, violence and sexual abuse; prolonged sexual abuse for adults and children.
- Witnessing violent deaths.
- Being held hostage.
- Unexpected severe injury.
- Death of a close family member or friend.
What are the Factors that Puts you at More Risk to Develop PTSD?
- Trauma: Exposure to a traumatic event is very clearly linked to developing PTSD. Proximity to the scene of trauma, increased duration and intensity increase the risk. No predisposed conditions are necessary to develop PTSD if the trauma is very severe.

- Intrusive Thoughts and suppression of the thoughts play a role.
- Early Onset: Abuse, neglect and bullying as children and adults who were in foster care as children.
- Mental Health Issues: Pre-existing mental problems like anxiety or depression or having blood relatives who have these conditions and /or PTSD.
- Lack of Support System: Not having family and friends to support you after the trauma to console and discuss.
- Genetic Factors: Susceptibility to PTSD is hereditary. A genetically smaller hippocampus has been linked to developing PTSD after a traumatic attack, while a smaller hippocampus along with startle responses are biomarkers for the risk of developing PTSD.
What are the Complications or Concurrent Conditions that Usually Go Along With PTSD?
- Mental health problems – depression, anxiety or phobias.
- Self-harming behavior – such as drug or alcohol misuse; this prolongs their recovery time.
- Physical symptoms – such as headaches, dizziness, chest pains and stomach aches.
- Eating disorders.
- Suicidal thoughts.
- Work-related problems and the breakdown of relationships.
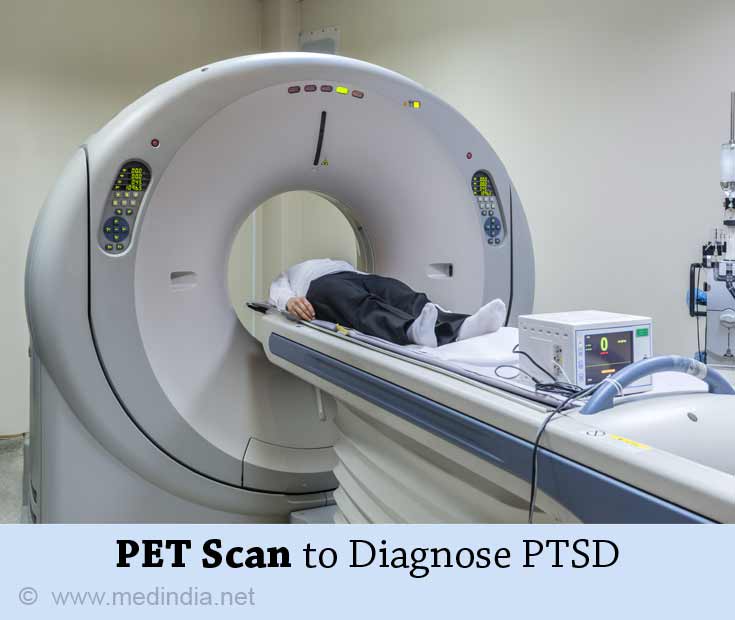
How Do You Diagnose PTSD?
Mental health professionals have now clearly defined symptoms which help them recognize cases of PTSD. Discussion with patients and their families help the specialist in the diagnosis.
Scientists say that post-traumatic stress disorder is the result of an environmental shock which can have a deep impact on the brain, visible through an MRI (magnetic resonance imaging) and PET (positron emission tomography).
PET scans of PTSD victims show alterations in the way memories are stored in the brain. It is still unclear if these changes are reversible.
The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) by the American Psychiatric Associations has certain criteria which a person has to check to be diagnosed with PTSD.
There must have been an exposure to an event involving death, violence or serious injury in one of the following ways:
- Either as the first person or as a witness or by hearing that someone close to you experienced it.
- Exposed to recurring graphic details of the event.
At least one or more of the following signs or symptoms must be experienced after one month of the event:
- One re-experiencing symptom.
- One avoidance symptom.
- Two arousal and reactivity symptoms.
- Two mood-based symptoms.
Two subtypes are also included in the DSM-5 - the PTSD Preschool subtype for children under 6 years and PTSD Dissociative subtype for those having symptoms of feeling detached from their own mind and body, or feeling that the world is unreal.
How Do You Treat PTSD?
Treatment for PTSD may involve psychotherapy, medication or a combination of medication and psychotherapy. Treatment has to be personalized depending on the symptoms and the severity of the condition.
Treatment will also help with other problems that develop during PTSD like anxiety, depression and substance abuse.
Psychotherapy:
Also called “talk therapy”, this involves helping the individual verbalize the trauma and associated fears. Therapy will involve assisting the victim with techniques to cope, as well as to alter their pattern of thinking.
The patient is educated about the illness, the manner of treatment and the expected outcome before commencement of the treatment.
Research says that Cognitive Behavioral Therapy (CBT) is the most effective counseling method for PTSD. This may consist of:
1. Cognitive Therapy: Helps sufferers remember and analyze the event and their thoughts about it in a realistic way. This new way of looking at the event eliminates negative or guilty feelings they might be harboring inside them regarding the event.

2. Exposure Therapy: Helps people face the trauma by exposing them to it in a safe way. The affected people are made to imagine, write or visit the same setting through computer simulated “virtual reality” programs. They thus learn to control their fear and cope with their feelings. The feared situation is faced entirely within the confines of the therapist’s office.
Cognitive and exposure therapies go hand in hand. Cognitive therapies can be done individually or in a group. It comprises of 12 sessions lasting 60 to 90 minutes each.
3. Eye Movement Desensitization and Reprocessing (EMDR):
The therapist urges the victim to think about the event while focusing all the while either on movements (like the therapist’s hand moving forward and backward) or sounds (like hand tapping or tones). When the memory becomes less upsetting to think about, a positive thought is added to it.
4. Stress Inoculation Training: Breathing, muscle relaxation and positive self-talk are methods used in this technique to reduce anxiety. They help in alleviating the sleep problems associated with PTSD and in the management of anxiety and aggression.
Counseling the family members, especially parents of children with PTSD is immensely beneficial. Parents are educated on how to help the child cope with the debilitating symptoms of PTSD.
The Veterans Association (VA) of America uses 2 kinds of CBT to veterans with PTSD called Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE) Therapy.
- Cognitive Processing Therapy (CPT) is another form of cognitive therapy that helps you handle the upsetting thoughts in a new way. Negative thoughts like guilt are discussed with the therapist who identifies and changes these thoughts. Changing how you think about the event changes the way you feel about it.
- In Prolonged Exposure (PE) Therapy, the therapist will persistently ask you to discuss about the trauma over and over again to control and overcome the fear of the event. In fact, things that are being avoided are brought to the forefront. Practically, the therapist will help you work your way up into doing something that you have avoided so far, like driving a car due to a bad accident.
Medications:
A psychiatrist has to be consulted when medication is the stand-alone option or when used in combination with psychotherapy.
The drug of choice will be prescribed at a low dose to start off with. Frequent visits will have to be made to slowly escalate the dose if the drug is working or to try another drug or a combination of drugs. Side effects will have to be discussed. With the correct drug(s), improvement will be seen in a few weeks.
- Selective Serotonin Reuptake Inhibitors or SSRIs are antidepressants that reduce panic, anxiety, fear and depression and improve sleep and concentration. They also relieve impulsivity, aggression and suicidal thoughts that may plague many victims. Examples of drugs approved by FDA for PTSD are Sertraline and Paroxetine.
- Fluoxetine, another SSRI and Venlafaxine are also used off-label as first-line mono therapy in patients but are not FDA-approved. Venlafaxine acts as a serotonin reuptake inhibitor and as a combined serotonin-norepinephrine reuptake inhibitor depending on its dose.
- Anti-anxiety medications like Benzodiazepines are used to treat short-term acute anxiety and insomnia. There is a potential abuse issue with these drugs and hence should not be taken for a long time.
- Prazosin, an inhibitor of the Sympathetic Nervous System is effective in treating severe nightmares in children and adults with PTSD symptoms. It is not FDA-approved for treating PTSD but has been successful in treating veterans for sleep disturbance related to PTSD at doses lesser than for use in hypertension.
Medications may help for quick relief but only psychotherapy helps in eliminating the underlying cause of the symptoms. Without psychotherapy, medications may have to be taken for a long time.

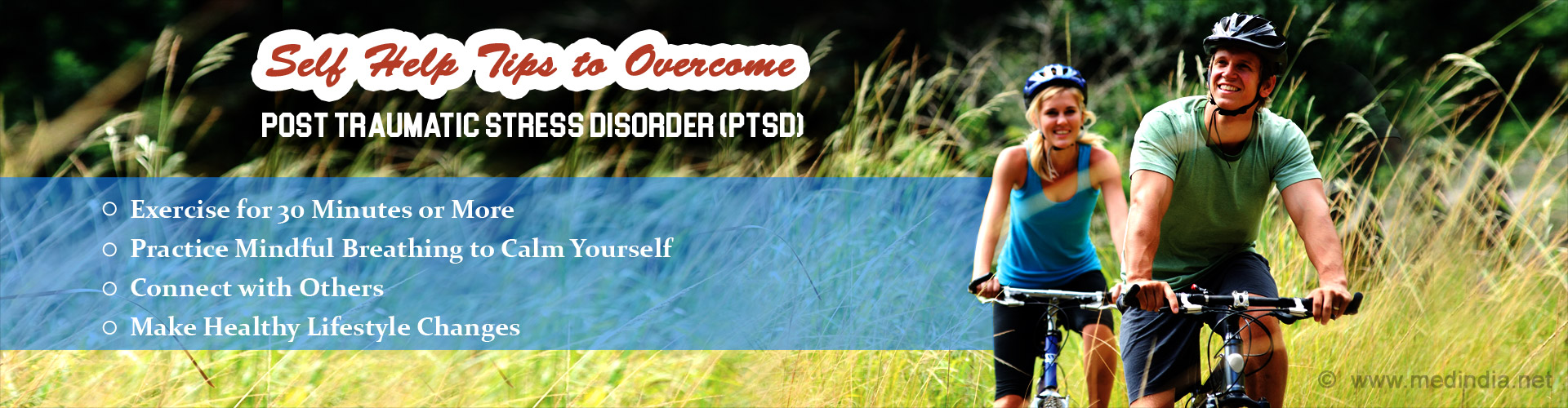
Apart from medication, the U.S. National Center for PTSD recommends moderate physical activity. The United States Marine Corps has programs that help military personnel to re-adjust to civilian life again and get better with family relationships.