DEFINITION
Lupus is a disorder of the autoimmune disease. In autoimmune
diseases, the body harms its own healthy cells and tissues. This
leads to inflammation mage to various body tissues. Lupus can affect
many parts of the body, including the joints, skin, kidneys, heart,
lungs, blood vessels, and brain. Lupus is characterized by periods
of illness, called flares, and periods of wellness (remission).
Although lupus is used as a broad term, several kinds of lupus
exist.
Systemic lupus erythematosus is the most
common form of the disease. The symptoms of SLE may be mild or
serious.
Discoid lupus erythematosus refers to a skin
disorder in which a red, raised rash appears on the face, scalp, or
elsewhere. The raised areas may become thick and scaly and may cause
scarring. The rash may last for days or years and may recur. A small
percentage of persons with discoid lupus have or develop SLE.
Drug-induced lupus refers to a form of lupus caused
by specific medications. Symptoms are similar to those of SLE and
typically resolve when the drug is stopped.
Neonatal
lupus is a rare form of lupus affecting newborn babies of women
with SLE or certain other immune-system disorders. At birth, the
babies have a skin rash, liver abnormalities, or low blood counts,
which resolve entirely over several months. However, babies with
neonatal lupus may have a serious heart defect. Physicians can now
identify most at-risk mothers, allowing for prompt treatment of the
infant at or before birth. Neonatal lupus is very rare, and most
infants of mothers with SLE are entirely healthy.
At
present, no cure for lupus exists. However, lupus can be very
successfully treated with appropriate drugs, and most persons with
the disease can lead active, healthy lives.
ETIOLOGY
Lupus is a
complex disease, the cause of which is unknown. In addition, some
autoantibodies join with substances from the body's own cells or
tissues to form molecules called immune complexes. A buildup of
these immune complexes in the body also contributes to inflammation
and tissue injury in persons with lupus. Researchers do not yet
understand all the factors that cause inflammation and tissue damage
in lupus.
SYMPTOMS
Each person's experience
with lupus is different, though patterns exist that permit accurate
diagnosis. Symptoms can range from mild to severe and may come and
go over time.
Common symptoms of lupus include painful or
swollen joints, muscle pain, unexplained fever, skin rashes, and
extreme fatigue. A characteristic skin rash may appear across
the nose and cheeks-the so-called butterfly or malar rash. Other
rashes may occur elsewhere on the face and ears, upper arms,
shoulders, chest, and hands.
Other symptoms of lupus include
chest pain, unusual hair loss, sensitivity to the sun, anemia, and
pale or purple fingers or toes from cold and stress (Raynaud's
phenomenon). Some persons also experience headaches, dizziness,
depression, or seizures. New symptoms may continue to appear years
after the initial diagnosis, and different symptoms can occur at
different times.
The following systems in the body also can
be affected by lupus.
 Kidneys:
Inflammation of the kidneys can impair their ability to get rid of
waste products and other toxins from the body effectively. Usually
no pain is associated with kidney involvement, though some persons
may notice that their ankles swell. Most often the only indication
of kidney disease is an abnormal urine or blood test. Kidneys:
Inflammation of the kidneys can impair their ability to get rid of
waste products and other toxins from the body effectively. Usually
no pain is associated with kidney involvement, though some persons
may notice that their ankles swell. Most often the only indication
of kidney disease is an abnormal urine or blood test.
 Lungs: Some persons with lupus
develop pleuritis. Persons with lupus also may get pneumonia. Lungs: Some persons with lupus
develop pleuritis. Persons with lupus also may get pneumonia.
 Central nervous system : In some
persons, lupus affects the brain or central nervous system. This can
cause headaches, dizziness, memory disturbances, vision problems,
stroke, or changes in behavior. Central nervous system : In some
persons, lupus affects the brain or central nervous system. This can
cause headaches, dizziness, memory disturbances, vision problems,
stroke, or changes in behavior.
 Blood
vessels: Blood vessels may become inflamed, affecting the way
blood circulates through the body. The inflammation may be mild or
severe. Blood
vessels: Blood vessels may become inflamed, affecting the way
blood circulates through the body. The inflammation may be mild or
severe.
 Blood: Persons with lupus may
develop anemia, leukopenia, or thrombocytopenia. Some persons with
lupus may have abnormalities that cause an increased risk for blood
clots. Blood: Persons with lupus may
develop anemia, leukopenia, or thrombocytopenia. Some persons with
lupus may have abnormalities that cause an increased risk for blood
clots.
 Heart: In some persons with lupus, myocarditis, endocarditis,
or pericarditis can occur, causing chest pains or other symptoms.
Lupus can also increase the risk of atherosclerosis
Heart: In some persons with lupus, myocarditis, endocarditis,
or pericarditis can occur, causing chest pains or other symptoms.
Lupus can also increase the risk of atherosclerosis
Despite
the symptoms persons with lupus can maintain a high quality of life
overall. One key to managing lupus is understanding the disease and
its impact.
Learning to recognize the warning signs of a
flare can help a person take steps to ward it off or reduce its
intensity. Many persons with lupus experience increased fatigue,
pain, a rash, fever, abdominal discomfort, headache, or dizziness
just before a flare.
DIAGNOSIS
The diagnosis of lupus
can be difficult. It may take months or even years for physicians to
piece together the symptoms to diagnose this complex disease
accurately.
No single test can determine whether a person
has lupus, but several laboratory tests may aid in the diagnosis.
Most persons with lupus test positive for ANA.
However, there are a number of other causes of positive ANA results,
including infections and other rheumatic or immune
diseases-occasionally they even are found in healthy adults. The ANA
test simply provides another clue for the physician to consider in
making a diagnosis.
In
addition, blood tests for individual types of autoantibodies exist
that are more specific to persons with lupus, though not all persons
with lupus test positive for these, and not all persons with these
antibodies have lupus. These antibodies include anti-DNA,
anti-Sm, anti-RNP, anti-Ro (SSA), and anti-La (SSB). These
antibody tests may help in the diagnosis of lupus.
Some
tests are used less frequently but may be helpful if the cause of a
person's symptoms remains unclear. A biopsy of the skin or
kidneys may be indicated if those body systems are
affected. A test for syphilis or the anticardiolipin
antibody may also be useful. Positive test results do not mean that
a person has syphilis; however, the presence of this antibody may
increase the risk of blood clotting and can increase the risk of
miscarriages in pregnant women with lupus. Again, all these tests
merely serve as tools in making a diagnosis.
Other
laboratory tests are used to monitor the progress of the disease
once it has been diagnosed. A complete blood count, urinalysis,
blood chemistries, and erythrocyte sedimentation rate test can
provide valuable information. Another common test measures the blood
level of a group of substances called complement. Persons with lupus often
have increased erythrocyte sedimentation rates and low complement
levels, especially during flares of the disease.
Persons
diagnosed with systemic lupus erythematosus (SLE) have
autoantibodies in their blood years before any symptoms appear,
according to an article in the October 16, 2003, issue of The New
England Journal of Medicine.
The early detection of
autoantibodies may facilitate the recognition of those persons who
will develop SLE and may allow physicians to monitor them before the
disease might otherwise be noticed.
THINK ABOUT
THESE
A cataract cannot return
because all or part of the lens has been removed. However, in some
people who have had extracapsular surgery or phacoemulsification,
the lens capsule becomes cloudy after a year. It causes the same
vision problems as a cataract does. To correct this, laser
capsulotomy can be performed. In laser (YAG) capsulotomy a laser
(light) beam is used to make a tiny hole in the capsule to let light
pass. This surgery is painless and does not require stay in the
hospital.
Full Source Title:American Journal of
Medicine
Abstract
PURPOSE:We sought to assess the nephritogenic
antibody profile of patients with systemic lupus erythematosus (SLE), and to determine which
antibodies were most useful in identifying patients at risk of
nephritis. METHODS: We studied 199 patients with SLE, 78 of whom had
lupus nephritis. We assayed serum samples for antibodies against
chromatin components (double-stranded deoxyribonucleic acid [dsDNA],
nucleosome, and histone), C1q, basement membrane components (laminin,
fibronectin, and type IV collagen), ribonucleoprotein, and
phospholipids. Correlations of these antibodies with disease
activity (SLE Disease Activity Index) and nephropathy were assessed.
Patients with no initial evidence of nephropathy were followed
prospectively for 6 years. RESULTS: Antibodies against dsDNA,
nucleosomes, histone, C1q, and basement membrane components were
associated with disease activity (P <0.05). In a multivariate
analysis, anti-dsDNA antibodies (odds ratio [OR] = 6; 95% confidence
interval [CI]: 2 to 24) and antihistone antibodies (OR = 9.4; 95%
CI: 4 to 26) were associated with the presence of proliferative
glomerulonephritis. In the prospective study, 7 (6%) of the 121
patients developed proliferative lupus glomerulonephritis after a
mean of 6 years of follow-up. Patients with initial antihistone (26%
[5/19] vs. 2% [2/95], P = 0.0004) and anti-dsDNA reactivity (6%
[2/33] vs. 0% [0/67], P = 0.048) had a greater risk of developing
proliferative glomerulonephritis than patients without these
autoantibodies.
CONCLUSION: In addition to
routine anti-dsDNA antibody assay, antihistone antibody measurement
may be useful for identifying patients at increased risk of
proliferative glomerulonephritis.
Full Source Title:Arthritis and Rheumatism
Abstract:
OBJECTIVE: To
determine the degree to which changes in C3 and C4 precede or
coincide with changes in systemic lupus erythematosus (SLE)
activity, as measured by 5 global activity indices, the physician's
global assessment (PGA), modified SLE Disease Activity Index
(M-SLEDAI), modified Lupus Activity Index (M-LAI), Systemic Lupus
Activity Measure (SLAM), and the modified British Isles Lupus
Assessment Group (M-BILAG), and to evaluate the association between
changes in C3 and C4 levels and SLE activity in individual organ
systems. RESULTS: Lupus flares occurred at 12% of visits based on
the PGA, 19% based on the M-SLEDAI, 25% based on the M-LAI, 13%
based on the SLAM, and 12% based on the M-BILAG. Recent changes in
C3 and C4 levels were not associated with flares based on 3 of the 5
activity indices. Flares defined by the M-LAI were more frequent
when there was a concurrent decrease in C3 (odds ratio [OR] 1.9, 95%
confidence interval [95% CI] 1.1-3.1) or C4 (OR 2.1, 95% CI
1.3-3.6). Higher flare rates, as defined by the SLAM, were
associated with previous increases in C3 (OR 1.6, 95% CI 1.0-2.6)
and C4 (OR 2.2, 95% CI 1.2-3.9). When individual organ systems were
analyzed, decreases in C3 and C4 were associated with a concurrent
increase in renal disease activity (OR 2.2, 95% CI 1.4-3.5 and OR
1.9, 95% CI 1.1-3.4, respectively). Decreases in C3 were also
associated with concurrent decreases in the hematocrit (OR 4.6, 95%
CI 1.7-12.3), platelet (OR 2.5, 95% CI 1.5-4.1), and white blood
cell (OR 2.2, 95% CI 1.3-3.6) counts. Previous increases in C3
levels were associated with a decrease in platelets (OR 1.7, 95% CI
1.1-2.7). A decrease in C4 was associated with a concurrent decrease
in the hematocrit level (OR 3.2, 95% CI 1.3-7.5) and platelet count
(OR 1.6, 95% CI 1.0-2.5).
CONCLUSION: Decreases in complement levels were
not consistently associated with SLE flares, as defined by global
measures of disease activity. However, decreasing complement was
associated with a concurrent increase in renal and hematologic SLE
activity
TREATMENT OF SLE
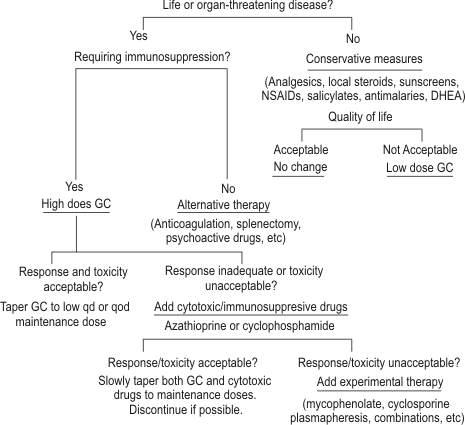
CONSERVATIVE MANAGEMENT
Arthritis, Arthralgia, and
Myalgia
Arthritis, arthralgia, and myalgia are the most
common manifestations of SLE. Severity ranges from mild to disabling. For
patients with mild symptoms, administration of analgesics,
nonsteroidal anti-inflammatory drugs (NSAIDs), or salicylates may
provide adequate relief, although none of these is as effective as
glucocorticoids.
In many SLE patients, musculoskeletal symptoms are
not well controlled by salicylate or NSAID therapy. A trial of
antimalarial drugs may be useful in such
individuals.
Hydroxychloroquine is the preferred
antimalarial agent in the United States (chloroquine may be more effective
but has a higher incidence of retinal toxicity: quinacrine is often
effective but rarely can cause aplastic anemia). The usual dose of
hydroxychloroquine for SLE patients with arthritis is 400 mg
daily. If response does not occur within 6 months, the patient
can be considered a nonresponder and the drug stopped. If
hydroxychloroquine is used for more than 6 months or chloroquine is used
for more than 3 months, regular examination by an ophthalmologist for
retinal damage is mandatory. If antimalarials are effective, the
maintenance dose should be reduced periodically if possible, or the drug
should be withdrawn when a patient is doing well, because the retinal
toxicity is cumulative.
Some patients with arthritis or arthralgia
do not benefit from NSAIDs or salicylates with or without antimalarials.
Administration of dihydroandrosterone (DHEA), 100 to 200
mg daily, lowers activity of SLE in some patients, including arthritis/arthralgias.
Methotrexate in weekly oral or parenteral
doses of 10 to 20 mg may also be considered, because there are reports of
its efficacy in some cases.
However, none of these
interventions is as reliable as glucocorticoid therapy in suppressing
lupus arthritis and arthralgia. If quality of life is seriously
impaired by pain (or by the deformities that develop in about 10 percent
of individuals with lupus arthritis), the physician should consider
institution of low-dose glucocorticoids, not to exceed 15 mg each
morning.
Rare patients require high-dose
glucocorticoids or even cytotoxic drugs. Such interventions should be
avoided if possible. In fact, if arthritis is the major
manifestation of disease that compels the physician to choose high-dose
immunosuppressive treatments, it may be preferable to use around-the-clock
non-narcotic or narcotic analgesics to control pain, rather than to risk
life-threatening side effects of aggressive immunosuppression.
Cutaneous
Lupus
As
many as 70 percent of patients with SLE are photosensitive..Patients
should begin with preparations that block UVA and UVB.
Sunscreens can be locally irritating (especially those
that contain PABA); patients may need to try several preparations to find
one that is not irritating.
Local
glucocorticoids, including topical creams and ointments and
injections into severe skin lesions, are also helpful in lupus dermatitis.
[ Patients with disfiguring (discoid) or extensive lesions should be seen
by a dermatologist, because management of severe lupus dermatitis can be
difficult.
Antimalarial agents are useful in some
patients with lupus dermatitis, whether the lesions are those of SLE,
subacute cutaneous lupus, or discoid lupus. Antimalarials have multiple
sunblocking, anti-inflammatory, and immunosuppressive effects. They also
bind melanin and serve as sunscreens, and they have antiplatelet and
cholesterol-lowering effects. All these properties may be beneficial to
patients with SLE.
Responses to chloroquine and quinacrine are
usually demonstrable within 1 to 3 months; responses to hydroxychloroquine
may require 3 to 6 months. Antimalarials may be steroid sparing.
Recommended initial doses of antimalarials are hydroxychloroquine, 400 mg
daily, chloroquine phosphate, 500 mg daily, and quinacrine, 100 mg daily.
Higher doses can be given for brief periods (2 to 4 weeks). After disease
is well controlled, the drugs can be slowly tapered. Daily doses can be
reduced, or the drug can be given less frequently (e.g., a few days each
week). The combination of hydroxychloroquine (or chloroquine) and
quinacrine is probably synergistic and can be used in patients refractory
to single-drug therapy.
Toxicities of these agents are important
but infrequent in comparison with other agents used to treat SLE. Retinal
damage is the most important; it can occur in up to 10 percent of patients
receiving chronic chloroquine therapy but is much less frequent in those
receiving hydroxychloroquine. Regular ophthalmologic examinations
with appropriate special testing identify retinal changes early.
If changes occur, antimalarial therapy should be stopped or the daily dose
decreased. This strategy substantially lowers the incidence of clinically
important retinal toxicity. Retinopathy is rare in patients treated with
quinacrine.
For individuals with lupus rash resistant to
antimalarials and other conservative strategies, etretinate has been
beneficial. The retinates are teratogenic, cause cheilitis in
most patients, and elevate cholesterol and triglyceride levels in some.
Patients resistant to antimalarials and retinates may require systemic
glucocorticoids, which improve lupus skin lesions of any type. Additional
treatments, which should be considered experimental for dermatologic
lupus, include dapsone, thalidomide, and cytotoxic drugs.
Dapsone has been used in discoid lupus,
urticarial vasculitis, and bullous LE lesions with some success. It has
significant hematologic toxicities (including methemoglobinemia,
sulfhemoglobinemia, and hemolytic anemia) and can occasionally worsen the
rashes of LE. Some steroid-resistant cases have improved when treated with
cytotoxic drugs such as azathioprine or methotrexate.
Successful treatment of refractory lupus rashes with
thalidomide has been reported. Development of peripheral
neuropathy associated with thalidomide is not uncommon. This highly
teratogenic drug is available on special request from the manufacturer,
with appropriate assurances that the patient cannot become pregnant.
Fatigue
and Systemic Complaints
Fatigue is common in patients with SLE and may be the
major disabling complaint. It reflects multiple problems, including
depression, sleep deprivation, and fibromyalgia. Fever and weight loss, if
mild, can be managed with the conservative approaches
outlined in the preceding paragraphs. When severe, systemic
glucocorticoid therapy is necessary.
Serositis
Episodes of chest and abdominal pain may be
secondary to lupus serositis. In some patients, complaints respond to
salicylates, NSAIDs (indomethacin may be best), or antimalarial therapies,
or to low doses of systemic glucocorticoids, such as 15
mg/day In others, systemic glucocorticoids must be given in high
doses to achieve disease remission.
RECENT ADVANCES
TABLE 1
-- APPROACHES IN THE MANAGEMENT OF SYSTEMIC LUPUS
ERYTHEMATOSUS
|
| Agent |
Target |
| Anti-CD40L (gp 39)
mAbs |
T-cell activation/T-cell-B-cell
collaboration |
| CTLA-4Ig |
|
| 3E10 mAb vaccine |
Inhibition of Ab
production |
| LJP 394: B-cell
toleragen |
Inhibition of Ab
production |
| rHuDNAse |
Inhibition of Ab
production |
| Anti-C5 mAb |
Complement activation/immune
complex deposition |
| Anti-IL-10 mAbs |
Cytokine
activation/modulation |
| AS101 (anti-IL-10) |
Cytokine
activation/modulation |
| Gene therapy |
Cytokine
activation/modulation |
| Thalidomide (anti-tumor necrosis
factor-alpha) |
Cytokine
activation/modulation |
| IVIg |
Immunomodulation |
| Bindarit |
Immunomodulation |
| Plasmapheresis |
Immunomodulation |
| *Mycophenolate
mofetil |
Immunomodulation |
| Immunoadsorption |
Immunomodulation |
| 2CdA |
Immunomodulation |
| Fludaribine |
Immunomodulation |
| Methimazole |
Immunomodulation |
| Stem cell
transplantation |
Stem cells |
| Immunoablative
treatment |
|
| DHEA |
Sex hormones |
| Selective estrogen receptor
modulators |
Sex
hormone | |
|
*Mycophenolate mofetil has been tried
as a treatment for several autoimmune diseases, on the basis of the
positive experience with this drug in recipients of solid-organ
transplants. The parent compound is hydrolyzed to mycophenolic acid,
an inhibitor of inosine monophosphate dehydrogenase, which blocks
several steps in the effector arm of the immune system. In mice with
lupus, mycophenolate mofetil prolonged overall survival and delayed
the onset and severity of nephritis.7 In small studies of patients
with lupus nephritis that was resistant to cyclophosphamide,
mycophenolate mofetil appeared to be effective in controlling renal
disease.
Treatment of Lupus Nephritis
The standard of care for the treatment of
aggressive forms of the disorder is the administration of
intravenous cyclophosphamide.3 In addition to oral
glucocorticoids, cyclophosphamide is given in monthly
intravenous pulses for at least six consecutive months. In
one study, exacerbations of lupus nephritis were reduced when
intravenous cyclophosphamide was given every three months for an
additional two years.
Chan et al. present the results of a
study in Hong Kong in which patients with diffuse proliferative
lupus nephritis were treated with prednisolone and mycophenolate
mofetil or with prednisolone and cyclophosphamide followed by
prednisolone and azathioprine.The study provides evidence
that treatment with mycophenolate mofetil is as effective as and has
fewer side effects than sequential treatment with cyclophosphamide
and azathioprine. There are several reasons for caution in
generalizing these findings to other patients with diffuse
proliferative lupus glomerulonephritis.
*Prophylactic anticoagulation therapy is not
justified in patients with high titer anticardiolipin antibodies
with no history of thrombosis.
*However, if
a history of recurrent deep vein thrombosis or pulmonary embolism is
established, long-term anticoagulant therapy with international
normalized ratio (INR) of approximately 3 is needed.
Antiphospholipid syndrome
The
syndrome occurs most commonly in young to middle-aged adults;
however, it also can occur in children and the elderly. Among
patients with SLE, the prevalence of antiphospholipid antibodies is
high, ranging from 12% to 30% for anticardiolipin
antibodies, and 15% to 34% for lupus anticoagulant
antibodies. In general, anticardiolipin antibodies occur
approximately five times more often then lupus anticoagulant in
patients with antiphospholipid syndrome. This syndrome is
the most common cause of acquired thrombophilia, associated
with either venous or arterial thrombosis or both. It is
characterized by the presence of antiphospholipid antibodies,
recurrent arterial and venous thrombosis, and spontaneous abortion.
Rarely, patients with antiphospholipid syndrome may have fulminate
multiple organ failure, or catastrophic antiphospholipid syndrome.
This is caused by widespread microthrombi in multiple vascular beds,
and can be devastating. Patients with catastrophic antiphospholipid
syndrome may have massive venous thromboembolism, along with
respiratory failure, stroke, abnormal liver enzyme concentrations,
renal impairment, adrenal insufficiency, and areas of cutaneous
infarction.
According to the international consensus
statement, at least one clinical criterion (vascular thrombosis,
pregnancy complications) and one laboratory criterion (lupus
anticoagulant, antipcardiolipin antibodies) should be present for a
diagnosis of antiphospholipid syndrome.
The
hallmark result from laboratory tests that defines antiphospholipid
syndrome is the presence of antibodies or abnormalities in
phospholipid-dependent tests of coagulation, such as dilute
Russell viper venom time. There is no consensus for
treatment among physicians. Overall, there is general agreement that
patients with recurrent thrombotic episodes require
life-long anticoagulation therapy and that those with recurrent
spontaneous abortion require anticoagulation therapy and low- dose
aspirin therapy during most of gestation.
|
|
| CONCLUSIONS
|
|
An
appreciation of the many facets of SLE is essential, including a
recognition of the current limit of our knowledge about the disease
and its management. A better understanding of the pathogenesis of
SLE promises to provide much information about the nature and the
role of the immune response in this and other diseases.
|
|