- Nutrition and bone health in women after the menopause. - (https://journals.sagepub.com/doi/10.2217/WHE.14.40)
- Osteoporosis - (https://my.clevelandclinic.org/health/diseases/4443-osteoporosis)
- Nutrients and Dietary Patterns Related to Osteoporosis. - (https://www.mdpi.com/2072-6643/12/7/1986)
- Nutrition and osteoporosis prevention and treatment. - (http://bmrat.org/index.php/BMRAT/article/view/598)
- The Mediterranean Diet in Osteoporosis Prevention: An Insight in a Peri- and Post-Menopausal Population. - (https://www.mdpi.com/2072-6643/13/2/531)
- Does Panchatikta ghrita have anti-osteoporotic effect? Assessment in an experimental model in ovariectomized rats. - (https://www.sciencedirect.com/science/article/pii/S0975947619300336?via%3Dihub)
- Ayurveda medicinal plants for Asthikshaya (Osteoporosis): A Review. - (https://www.ayurvedjournal.com/JAHM_201626_08.pdf)
- Food and Your Bones - Osteoporosis Nutrition Guidelines. - (https://www.bonehealthandosteoporosis.org/patients/treatment/nutrition/)
- Mayo Clinic Q and A: Osteoporosis and a bone-healthy diet. - (https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-osteoporosis-and-a-bone-healthy-diet/)
- How is osteoporosis treated or managed? - (https://www.healthdirect.gov.au/osteoporosis#managed)
About
Osteoporosis is a progressive disease characterized by loss of bone mineral density, deterioration of bone structure and strength, and increased risk of bone fractures. The accelerated bone turnover associated with osteoporosis often results in fractures, frequently occurring in the hip, forearm, humerus, and spine.
The risk factors include age (>50 years), family history, medical conditions (like an overactive thyroid, celiac disease, bariatric surgery, hormonal treatment in cancer), dietary habits, sedentary lifestyle, and use of tobacco and alcohol(1✔ ✔Trusted Source
Nutrition and bone health in women after the menopause.
Go to source, 2✔ ✔Trusted Source
Osteoporosis
Go to source).
The Importance of Diet in Managing Osteoporosis
Diet for osteoporosis holds critical interest due to its benefits in prevention and condition management. Different dietary patterns have been researched to understand their effects on bone health. The best diet for bone health should comprise a higher intake of vegetables, fruits, whole grains, fish, poultry, nuts, and legumes.
Among Asians, it was found that increased intake of fruits, vegetables, and soy was linked with a reduced risk of osteoporosis and fractures. Therefore, following a healthy dietary pattern that includes bone strengthening foods is critical in managing osteoporosis(3✔ ✔Trusted Source
Nutrients and Dietary Patterns Related to Osteoporosis.
Go to source).
Nutritional Needs for Osteoporosis
The essential nutrients for stronger bones that play pivotal roles in osteoporosis prevention and pathogenesis are calcium, vitamin D, phosphorus, magnesium, potassium, vitamin K, vitamin C, protein, and many more.
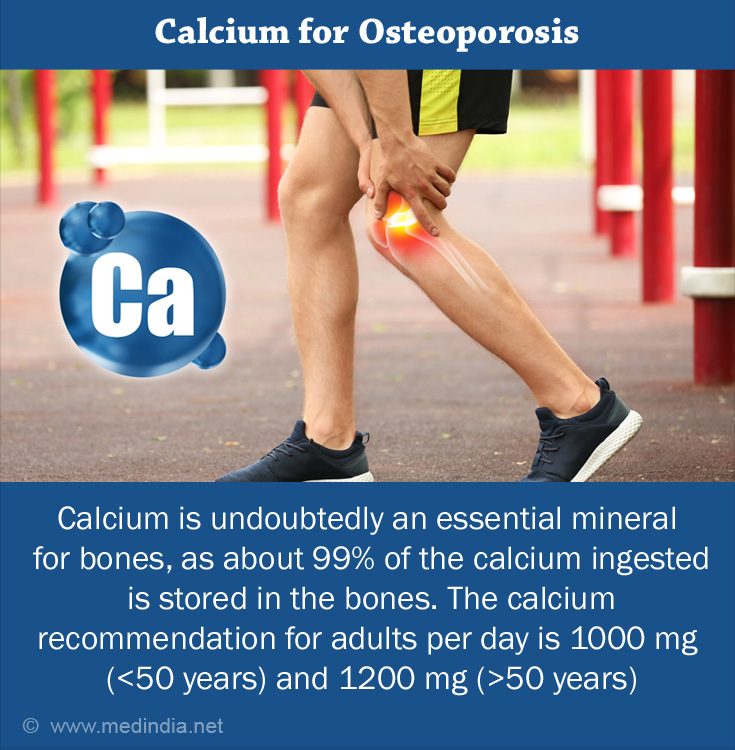
- Calcium is undoubtedly an essential mineral for bones, as about 99% of the calcium ingested is stored in the bones. About 67% of the bones have calcium as calcium phosphate (hydroxyapatite crystals) embedded in the collagen fibrils. Insufficiency in calcium shoots up the secretion of parathyroid hormone (PTH) which results in the resorption of calcium from bones. Continued resorption decreases the bone mineral density (BMD) thereby augmenting the risk for osteoporosis. Studies have shown that increased calcium intake in the growing stage slows down the loss of BMD in the elderly, and prevents osteoporosis. The calcium recommendation for adults per day is 1000 mg (<50 years) and 1200 mg (>50 years) for healthy bones. According to the European guidance for the diagnosis and management of osteoporosis, postmenopausal women should consume 1000mg of calcium per day(1✔ ✔Trusted Source
![Calcium for Osteoporosis Calcium for Osteoporosis]()
Nutrition and bone health in women after the menopause.
Go to source, 4✔ ✔Trusted Source
Nutrition and osteoporosis prevention and treatment.
Go to source). - Vitamin D is important for the homeostasis of calcium and phosphorus. Vitamin D3 in the bone stimulates osteoblasts (bone-building cells) and thereby increases the levels of osteocalcin and alkaline phosphatase. The recommended Vitamin D intake per day is 10 mcg (50-70 years) and 15 mcg (>70 years). However, studies demonstrated that a higher dose of about 800-1000 IU/day imparts benefits to bones.
- Levels of Protein: Both high and low levels of protein pose harm to bone health. A high protein intake causes an acidic environment that leads to urinary excretion of calcium and thereby loss of BMD. Whereas a low protein intake is also correlated with the risk of low BMD, osteoporosis, and fractures in the elderly. Adequate protein intake helps in the absorption of calcium and increases bone density and strength.
- Phosphorus imbalance in the body may end up limiting the mineralization and formation of bone by bringing down the activity of osteoblasts while increasing the activity of osteoclasts (bone-breaking cells), thereby increasing bone turnover.
- Magnesium plays a significant role in bone health. Lack of this nutrient can lead to endothelial dysfunction resulting in bone damage. Its deficiency stimulates the release of inflammatory cytokines, bone remodeling, poor cellular growth, and loss of BMD. Deficiency could also indirectly affect PTH and Vitamin D levels resulting in low calcium concentrations.
- Zinc is essential for osteoblasts formation, bone matrix formation, and preventing resorption.
- Copper is an integral mineral in lysyl oxidase, the enzyme performing functions in collagen and elastin, and superoxide dismutase, the enzyme responsible for bone resorption.
- Vitamin C has antioxidant activities, prevents the action of osteoclasts and also participates in collagen formation(3✔ ✔Trusted Source
Nutrients and Dietary Patterns Related to Osteoporosis.
Go to source, 4✔ ✔Trusted Source
Nutrition and osteoporosis prevention and treatment.
Go to source).
Bone-Healthy Diet for Osteoporosis
- The Mediterranean Diet exhibits protective effects against osteoporosis. A study found that good adherence to the Mediterranean diet showed a higher intake of calcium and high Vitamin D levels. In postmenopausal women, it was linked with higher BMD, muscle mass, and a lower incidence of fractures.
- Asian Dietary Pattern which includes soy, fish, vegetables, fruits, dairy products, white rice, and fermented foods like natto and kimchee was found to be positively associated with higher BMD, improved bone formation, and lowered risk for osteoporotic fractures(3✔ ✔Trusted Source
Nutrients and Dietary Patterns Related to Osteoporosis.
Go to source, 5✔ ✔Trusted Source
The Mediterranean Diet in Osteoporosis Prevention: An Insight in a Peri- and Post-Menopausal Population.
Go to source). - Ayurvedic Herbs have been researched to showcase protective effects on bone health. Panchatikta ghrita is a formulation made using five plants and is claimed to turn down bone degeneration in osteoporosis and improve bone-related parameters. Other popular ayurvedic preparations that pose anti-osteoporotic properties are ashwagandha, dadima, vidarikanda, vacha, and parushak(6✔ ✔Trusted Source
Does Panchatikta ghrita have anti-osteoporotic effect? Assessment in an experimental model in ovariectomized rats.
Go to source, 7✔ ✔Trusted Source
Ayurveda medicinal plants for Asthikshaya (Osteoporosis): A Review.
Go to source).
Foods to Include and Avoid in Your Everyday Diet
Foods that promote and impede bone health are discussed below:
- Dairy products (milk, yogurt, cheese) and vegetables like kale, broccoli, mustard greens, collard greens, and turnip greens are the primary calcium rich foods for bones. Some foods,like soy milk, fruit juices, cereals, rice milk, and bread, are fortified with vitamin D.
- Including fatty fish like tuna, mackerel, sardines, and salmon providesvitamin D, calcium, and protein.
- Vegetables like spinach, plantains, sweet potatoes, tomatoes, collard greens, lady’s finger, and beet greens are rich in magnesium.
- Potassium-rich foods include oranges, bananas, papaya, sweet potatoes, tomatoes, and plantains.
- Citrus fruits, berries, brussels sprouts, capsicum, papaya, grapefruits, and broccoli can be considered as the sources of Vitamin C. Eating plenty of fruits and vegetables will provide adequate Vitamin A and K.

- Protein sources like beans, nuts, sprouts, seeds, fish, skinless poultry, eggs, and lean cuts of meat can be consumed. However, a very high protein diet can also harm bones.
- Processed foods and beverages like soft drinks contain sugars, salt, and phosphorus which may interfere with calcium absorption and are best avoided.
- Alcohol and caffeine should be limited as they may reduce calcium absorption and increase calcium excretion.
- Beans, being good sources of magnesium and calcium, also contain phytates that prevent calcium absorption. Hence, it is advisable to soak the beans before cooking(8✔ ✔Trusted Source
Food and Your Bones - Osteoporosis Nutrition Guidelines.
Go to source, 9✔ ✔Trusted Source
Mayo Clinic Q and A: Osteoporosis and a bone-healthy diet.
Go to source).
Managing Osteoporosis Through a Healthy Lifestyle
Making lifestyle changes helps manage osteoporosis and prevent complications.
Cessation of smoking, limiting alcohol intake, following a healthy dietary pattern (rich in calcium, protein, magnesium, and other micronutrients), and adequate sunlight exposure can be adopted to follow a healthy lifestyle.
Exercise is highly valued for bone health. It can strengthen the bones and prevent falls. Strength training, jogging, brisk walking, and Tai chi can be practiced.
Falls should be prevented by taking the right precautions, including avoiding high heels, wearing non-slip footwear, having regular eye check-ups, reviewing drugs if experiencing dizziness frequently, and using a walking stick or hip protectors if needed(10✔ ✔Trusted Source
How is osteoporosis treated or managed?
Go to source).
Healthy Diet Builds Strong Bones
A well-planned, nutrient-rich diet is a rewarding tool for preventing and managing osteoporosis. A diet rich in calcium, vitamin D, protein, magnesium, potassium, vitamin C, zinc, phosphorus, and copper should be consumed. Regular intake of bone strengthening foods supports bone growth, prevents of bone diseases, and promotes stronger bones. Limiting alcohol intake, regular exercise, and preventing falls should be considered for strong bones.