Obinutuzumab Medication Information
Discover comprehensive details about Obinutuzumab, including its pronunciation, uses, dosage instructions, indications, and guidelines on how and when to take it or avoid it.
The updated prescription information covers potential side effects, precautions, warnings, and storage recommendations.
Additionally, explore the Obinutuzumab brands available in India and internationally, along with pricing information. For personalized advice, consult your healthcare provider.
Generic Name : Obinutuzumab Pronunciation : OH-bi-nue-TOOZ-ue-mab Therapeutic Classification : ChemotherapyBrand Names or Trade Names of Obinutuzumab
India :
Gazyva, Gazyvaro
Why is Obinutuzumab Prescribed? (Indications)
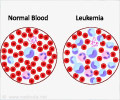
Obinutuzumab is prescribed to treat chronic lymphocytic leukemia (CLL) in combination with chlorambucil in adult patients who have not been previously treated for CLL.Obinutuzumab in combination with bendamustine is used to treat follicular lymphoma (FL) followed by obinutuzumab monotherapy in patients whose cancer condition has returned or not responded to other cancer treating medications.
Chronic lymphocytic leukemia (CLL) is one of the most common types of cancer of the blood and the bone marrow. Follicular lymphoma is a slow-growing form of non-Hodgkin’s lymphoma (NHL).
When should Obinutuzumab not be taken? (Contraindications)
Obinutuzumab should not be used in patients-• If there is an allergy to obinutuzumab
• Pregnancy and breastfeeding
• Children below 18 years of age
• Immunization with live viral vaccines (e.g., MMR, Polio, Typhoid)
• History of serum sickness or active infection
What is the dosage of Obinutuzumab?
Chronic lymphocytic leukemia: (CLL)Obinutuzumab should be administered for six 28-day treatment cycles.
The loading dose of obinutuzumab for the first cycle includes 100 mg on day 1 which can be increased to 900 mg on day 2 followed by 1000 mg of obinutuzumab on days 8 and 15.
The dose of obinutuzumab from cycles 2 to 6 is 1000 mg given on day 1.
Follicular lymphoma:
The dose of obinutuzumab should be given for 6 to 8 treatment cycles (28-day) followed by obinutuzumab monotherapy for every two months given for up to two years.
During cycle 1, the loading dose of obinutuzumab is 1000 mg given on days 1, 8, and 15. From cycles 2 to 8, the dose of obinutuzumab is 1000 mg given on day 1.
The maintenance dose is given with obinutuzumab alone after two months of the last dose of the 8th cycle followed by every two months for up to 2 years.
How should Obinutuzumab be taken?
Obinutuzumab is available in an injection form which should be given by a healthcare provider intravenously or deep into the vein slowly.Withdraw a required quantity of obinutuzumab from the vial and dilute with 0.9% sodium chloride and mix the diluted solution by gentle inversion.
The drug should be mixed in aseptic conditions and should not be combined with other drugs.
Patients can be premedicated with certain drugs to reduce the risk of infusion-related reactions (IRR) such as nausea, fever, breathing problems, vomiting, chills, chest pain, loose stools, and dizziness.
The drugs used for premedication include-
• Intravenous steroid (Dexamethasone 20 mg or Methylprednisolone 80 mg)
• Paracetamol or acetaminophen (650 mg to 1 gm)
• Antiallergic drug (Diphenhydramine 50 mg)
Hydrocortisone should not be used as it is not much effective against reducing the effect of infusion-related reactions.
Missed a Dose?
If a dose of obinutuzumab is missed, give the missed dose as soon as possible.The next dosing schedule of obinutuzumab can be adjusted to maintain an adequate time interval between the two doses.
What are the warnings and precautions for Obinutuzumab?
• Patients with a past history of hepatitis B virus infection should be carefully monitored for signs of fulminant hepatitis or liver damage. Lab values must be checked during and after the treatment with obinutuzumab as there is a possibility of reactivation of the hepatitis B virus.• Discontinue the treatment with obinutuzumab and provide appropriate medical care, if hypersensitivity reactions such as breathing difficulty, low blood pressure, and serum sickness occur.
• Patients should be monitored regularly for the counts of neutrophils and platelets along with any symptoms or signs of infections such as fever and cough.
• Symptoms of tumor lysis syndrome that include nausea, loose stools, vomiting, and weakness can occur during the treatment with obinutuzumab. Patients must be provided with proper supportive care by correcting water-electrolyte imbalance and monitoring the kidney function regularly.
• Patients must be monitored for any neurological changes such as confusion, dizziness, and loss of balance that could be symptoms of progressive multifocal leukoencephalopathy (PML) by performing brain MRI scan and lumbar puncture. The obinutuzumab dose can be reduced or the treatment can be discontinued based on the condition of the patient who develops PML.
What are the side effects of Obinutuzumab?
Gastrointestinal: Diarrhea, constipation, indigestion, loss of appetiteNervous system: Dizziness, confusion, difficulty in speech or to walk, loss of balance
Respiratory: Cough, nasal congestion, sneezing, inflammation of the sinuses, nasopharyngitis
Musculoskeletal: Joint pain, pain in the extremities, muscle pain or cramps
Blood: Low levels of neutrophils, lymphocytes, white blood cells
Lab abnormalities: Decreased levels of calcium, potassium, sodium, and phosphate in the blood, increased liver enzymes, and creatinine levels
Others: Headache, itching, fever, weakness, vision problems
What are the other precautions for Obinutuzumab?
Breastfeeding mothers should be advised not to breastfeed their babies during and 18 months after the obinutuzumab treatment is stopped.Women of reproductive potential living with active male partners should follow an effective contraceptive measure during obinutuzumab treatment and must continue the contraception for at least 18 months after the last dose of obinutuzumab.
Inspect the obinutuzumab vials and the diluted solution for the presence of any visible solid matter or discoloration before administering it to the patient.
What are the Drug Interactions of Obinutuzumab?
Patients on obinutuzumab treatment should avoid taking blood thinner medications such as warfarin, clopidogrel, dipyridamole, ticlopidine, cilostazol, and ticagrelor as these combinations may result in unusual bleeding episodes.Before the doctor prescribes obinutuzumab, patients must inform them about any prescription drugs, Over-The-Counter agents, and herbal supplements they are taking or plan to take to avoid dangerous drug-related side effects.
What are the storage conditions for Obinutuzumab?
Store obinutuzumab vials in a refrigerator at a temperature between 2°C and 8°C.Protect the obinutuzumab vials from light and do not freeze or shake.
The obinutuzumab diluted solution if not used immediately should be stored between 2°C and 8°C for up to 24 hours.
Keep obinutuzumab vials and the diluted solution away from the reach of children.