- Kunmam (Acid Peptic Disease) - (https://www.nhp.gov.in/Kunmam-(Acid-Peptic-Disease)_mtl)
- American College of Gastroenterology guideline on the management of Helicobacter pylori infection. - (https://www.ncbi.nlm.nih.gov/pubmed/17608775)
- The prevalence of Helicobacter pylori in acid peptic disease - (http://www.archintsurg.org/article.asp?issn=2278-9596;year=2014;volume=4;issue=2;spage=91;epage=95;aulast=Gupta)
- Long-term stress and Helicobacter pylori infection independently induce gastric mucosal lesions in C57BL/6 mice. - (https://www.ncbi.nlm.nih.gov/pubmed/12465722 )
- Peptic Ulcer Disease and Helicobacter pylori infection - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140150/)
- Peptic Ulcer - (http://research.omicsgroup.org/index.php/Peptic_ulcer)
- Peptic Ulcers: Causes, Prevention, Perforation and Treatment - (https://pdfs.semanticscholar.org/2743/c9faddd49671362f2fe2e4d45dac181089fe.pdf)
- Peptic Ulcer: Causes and Therapy - (https://www.pharmatutor.org/articles/peptic-ulcer-causes-and-therapy?page=5%2C4)
- Peptic Ulcer: Peptic Disorders: Merck Manual Home Edition.
- Chey WD, Wong BC. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. Aug 2007;102(8):1808-25.
- Kato, Ikuko; Abraham M. Y. Nomura, Grant N. Stemmermann and Po-Huang Chyou (1992). "A Prospective Study of Gastric and Duodenal Ulcer and Its Relation to Smoking, Alcohol, and Diet". American Journal of Epidemiology 135 (5): 521-530. PMID 1570818.
- Malagelada JR, Kuipers EJ, Blaser MJ. Acid peptic disease: clinical manifestations, diagnosis, treatment, and prognosis. In: Goldman L, Ausiello D, eds. Cecil Medicine. 23rd ed. Philadelphia, Pa: Saunders Elsevier; 2007:chap 142.
- Kim YH, Lee JH, Lee SS, et al. (2002). "Long-term stress and Helicobacter pylori infection independently induce gastric mucosal lesions in C57BL/6 mice". Scand. J. Gastroenterol. 37 (11): 1259-64. doi:10.1080/003655202761020515. PMID 12465722.
About
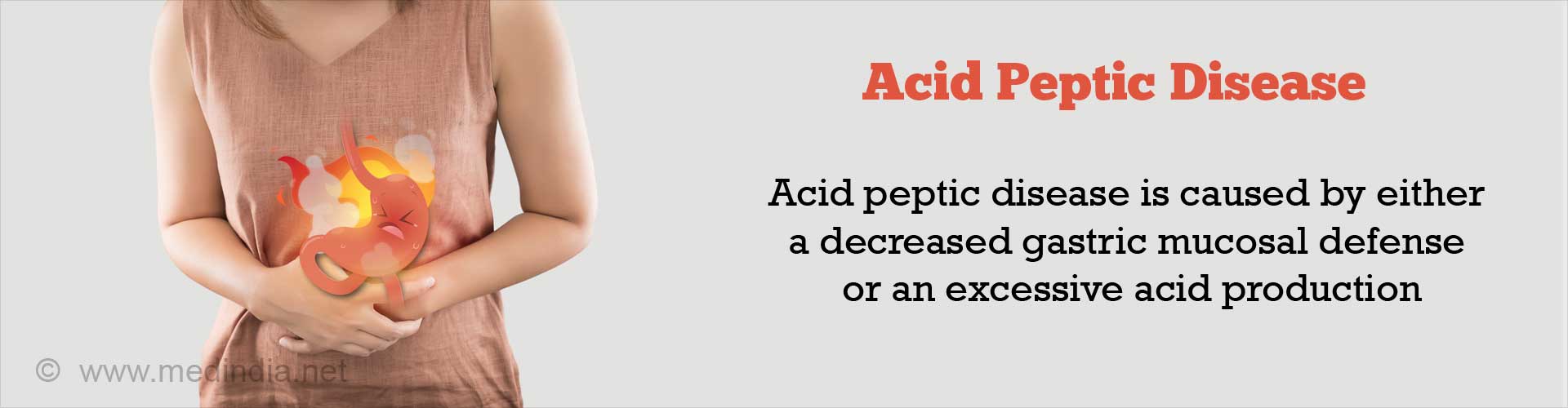
Excessive secretion of this acid and pepsin or a weakened stomach mucosal defense is responsible for damage to the delicate mucosa and the lining of the stomach, esophagus and duodenum resulting in ulceration which is known as “Acid Peptic Disease”.(1✔ ✔Trusted Source
Kunmam (Acid Peptic Disease)
Go to source)
Physiologically, a certain amount of acid is secreted by the gastric cells lining the stomach as a natural mechanism which serves to activate the digestive enzymes and help in the digestion and assimilation of important proteins so that they can be easily absorbed by the body.(2✔ ✔Trusted Source
American College of Gastroenterology guideline on the management of Helicobacter pylori infection.
Go to source)
“Acid peptic disease” is a collective term used to include many conditions such as gastro-esophageal reflux disease (GERD), gastritis, gastric ulcer, duodenal ulcer, esophageal ulcer, Zollinger Ellison Syndrome (ZES) and Meckel’s diverticular ulcer.(3✔ ✔Trusted Source
The prevalence of Helicobacter pylori in acid peptic disease
Go to source)
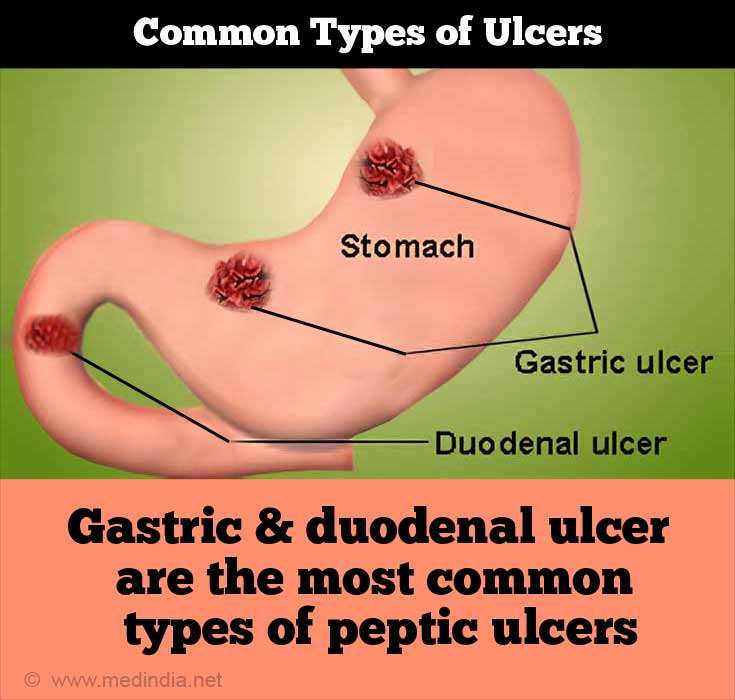
The commonest ulcers are the gastric and the duodenal ulcer.
Symptoms of peptic ulcers include abdominal pain, nausea, water brash, vomiting, loss of appetite and weight loss. Complications include bleeding, perforation, obstruction in the digestive tract and sometimes cancer.(4✔ ✔Trusted Source
Long-term stress and Helicobacter pylori infection independently induce gastric mucosal lesions in C57BL/6 mice.
Go to source, 5✔ ✔Trusted Source
Peptic Ulcer Disease and Helicobacter pylori infection
Go to source)
Peptic ulcer is diagnosed using blood and stool tests, breath tests, and endoscopy and barium radiography. The patient is treated with drugs that reduce acidity and sometimes in addition with certain antibiotics to eliminate the H pylori causing the infection (described below). Surgery may be required in some cases.
Causes of Acid Peptic Disease
Acid peptic disease is a result of either a decreased gastric mucosal defense or an excessive acid production.
Causes of acid peptic disease include:
- Helicobacter pylori: H.pylori is responsible for around 60%-90% of all gastric and duodenal ulcers.
- NSAIDs: Prostaglandins protect the mucus lining of the stomach. Non steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, diclofenac and naproxen prevent the production of these prostaglandins by blocking cyclo-oxygenase enzyme leading to ulceration and bleeding.
- Smoking, alcohol and tobacco: Cigarettes, alcohol and tobacco cause an instant and intense acid production which acts as though gasoline is poured over a raging fire!
- Blood group O: People with blood group “O” are reported to have higher risks for the development of stomach ulcers as there is an increased formation of antibodies against the Helicobacter bacteria, which causes an inflammatory reaction and ulceration.
- Heredity: Patients suffering from peptic ulcer diseases usually have a family history of the disease, particularly the development of duodenal ulcer which may occur below the age of 20.
- Steroids/Other medicines: Drugs like corticosteroids, anticoagulants like warfarin (Coumadin), niacin, some chemotherapy drugs, and spironolactone can aggravate or cause ulcers.
- Diet:
Low fiber diet , caffeinated drinks and fatty foods are linked to peptic ulcer. - Other diseases: Chronic liver, lung and kidney diseases especially tumors of the acid producing cells all predispose to peptic ulcers. Zollinger-Ellison Syndrome (ZES) is a rare pre-cancerous condition which causes peptic ulcer disease. It is a syndrome disorder wherein tumors in the pancreas and duodenum also known as gastrinomas produce a large amount of gastrin which is a hormone that stimulates gastric acid secretion. Endocrine disorders such as hyperparathyroidism are also implicated in the development of peptic ulcers.
- Stress: Stress and neurological problems can also be associated with the Cushing ulcer and peptic ulcer.(6✔ ✔Trusted Source
Peptic Ulcer
Go to source)
Symptoms and Signs of Acid Peptic Disease
Symptoms of peptic ulcers include abdominal pain, nausea, water brash, vomiting, loss of appetite and weight loss.(6✔ ✔Trusted Source
Peptic Ulcer
Go to source)
Peptic ulcer disease is usually a chronic problem with a natural history of relapse and remission which can last for over 10 years or even more. Gastric and duodenal ulcers usually have common symptoms such as:
- Abdominal Pain: A burning pain in the upper part of the abdomen usually related to mealtimes together with fullness, distension of the abdomen, bloating, with or without nausea and generalized discomfort also known as “dyspepsia”. The pain is usually so sharply localized that the patient can often indicate the exact place with two or three fingers called the “pointing sign”. Gastric ulcer pain is more after the ingestion of meals while duodenal ulcer pain occurs more due to hunger.
- Nausea, heart burn, vomiting, loss of appetite and weight loss.
- Gastric outlet obstruction: The ulcer could heal with scarring and result in narrowing of the gastric or intestinal lumen. This could cause an obstruction to food being passed forward.
- Vomiting or passing blood in stool: Signs of bleeding as vomiting of blood or black tarry color of the stool.
- Bleeding and perforation from the ulcer: Bleeding from the site of the ulcer with thinning of the wall may result in perforation.
What is the difference between gastric ulcer and duodenal ulcer?
Depending on the duration, peptic ulcers are classified into acute and chronic. Gastric ulcers develop more often in the elderly after the age of 60, while duodenal ulcers occur around the age of 30-40 years. Gastric ulcers are more common in women while men suffer more from duodenal ulcer. Chronic duodenal ulcer rarely develops into cancer while chronic gastric cancers are potentially precancerous. Chronic gastric ulcer is usually seen on the lesser curve of the stomach while the usual area of occurrence in a duodenal ulcer is the first part of the duodenum.
Differential Diagnosis, Complications and Diagnosis of Acid Peptic Disease
Peptic ulcer is diagnosed using blood and stool tests, breath tests, endoscopy and rarely now barium radiography. Complications include bleeding, perforation, obstruction in the digestive tract and sometimes cancer.
Differential Diagnosis or Other Possibilities:
Pain in the upper part of the abdomen is usually seen in the following conditions besides peptic ulcer disease:
- Pancreatitis
- Cholecystitis (bile duct inflammation) and biliary colic
- Hepatitis or hepatic congestion
- Stomach Cancer
- Pericarditis (Inflammation of the covering of the heart)
- Pleurisy (Inflammation of the covering of the lungs)
- Myocardial infarction or heart attack
Complications:
Besides having sleepless nights due to pain and other dyspeptic symptoms, bleeding, perforation, penetration into other organs and obstruction in the intestines are other complications which can develop due to chronic or acute acid peptic disorders. “Barrett’s esophagus” is a precancerous lesion which develops due to chronic GERD or “gastro esophageal reflux disorder”. GERD is a condition wherein the liquid contents of the stomach regurgitate back into the esophagus. This causes damage to the esophageal lining resulting in esophagitis and Barrett’s esophagus. Infection with H.pylori responsible for peptic ulcer disease can cause an atrophy of the stomach called “atrophic gastritis” which is a precancerous condition. Duodenal cancer is also a complication of the acid peptic disease.
Diagnosis:
Before instituting therapy, it is imperative to diagnose the ulcer disease and the H.pylori infection because treatment protocols are variable for different types of ulcer diseases. The treatment of an NSAID induced ulcer differs from the ulcer caused by H.pylori.
- Clinical History: Medical and family history establish whether ulcers are present in the family. Other information such as the misuse of NSAIDs, medicines taken and information regarding the use of alcohol, smoking and tobacco should also be elicited. Also the timing of food in relation to the pain and dyspepsia may help in the diagnosis.
- Blood Tests. Blood tests such as an enzyme-linked immunosorbent assay (ELISA) help in the measurement of antibodies to H. pylori. Serum gastrin levels should be measured in patients with multiple ulcers to consider gastrin secreting tumors or Zollinger-Ellison Syndrome. Tests for gastric secretion include the “pentagastrin test”, the “chew and spit test” and the “Hollander insulin test”.
- Stool Test. Stool test detects the presence of H. pylori in the feces and also establishes whether there is any recurrence after antibiotic therapy.
- Breath Test: The urea breath test (UBT) is helpful in the detection of H.pylori. The patient is made to drink a liquid containing carbon-labeled urea, which is broken down by the bacteria. The patient is subsequently asked to breathe into a sealed bag, which is tested for the presence of labeled carbon. A positive test indicates the presence of H pylori infection.
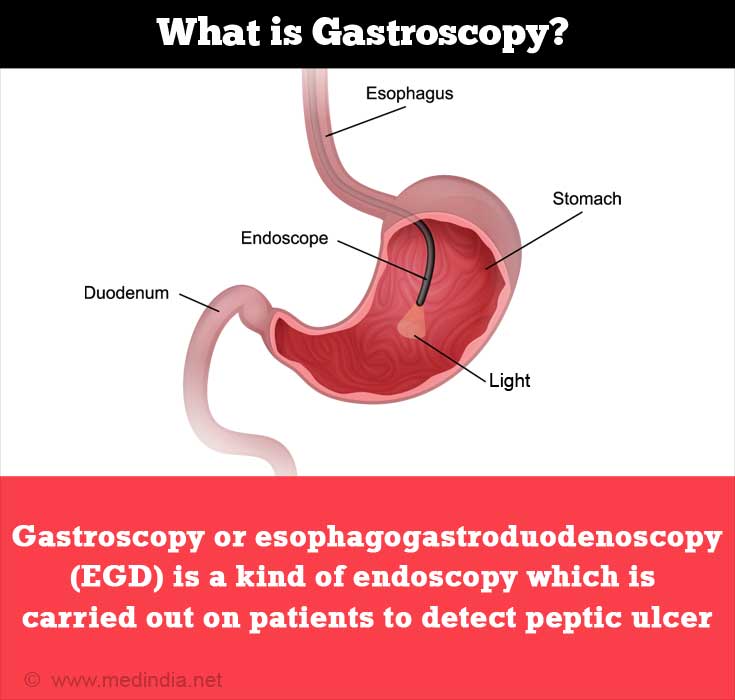
- Endoscopy: Endoscopy is considered a more accurate test for the diagnosis of “peptic ulcer diseases” and also helps in taking biopsy of the affected area. Gastroscopy or esophagogastroduodenoscopy (EGD) is a kind of endoscopy which is carried out on patients to detect peptic ulcer.
- Barium Radiography: X-rays are taken of the stomach, esophagus and duodenum after swallowing barium and the retention of contrast in the ulcer is monitored.(7✔ ✔Trusted Source
Peptic Ulcers: Causes, Prevention, Perforation and Treatment
Go to source)
Treatment for Acid Peptic Disease
Acid Peptic Disease is treated with drugs that reduce acidity and sometimes in addition, with certain antibiotics to eliminate the H pylori causing the infection. Surgery may be needed in cases of complication.(8✔ ✔Trusted Source
Peptic Ulcer: Causes and Therapy
Go to source)
Medical Management:
A) Diet: Dietary therapy relates to avoidance of spicy and oily foods which increase acid production and are difficult to digest. Avoid tea and coffee, alcohol, aspirin and other NSAIDs, chocolate, tobacco and cigarettes. Meals should preferably be light and at small intervals.
B) Eradication of H.pylori: The three way approach to eradicate H.pylori involves diagnosis, treatment and confirmation of the cure of H.pylori infection. The standard protocol to eradicate H.pylori involves the use of two or three antibiotics (e.g., amoxicillin, tetracycline, clarithromycin, metronidazole) and the use of a proton pump inhibitor (e.g., esomeprazole, omeprazole, lansoprazole, rabeprazole, pantoprazole) with or without a bismuth compound for around 2-3 weeks and repeated if there is recurrence.
C) Avoid NSAIDs or the concurrent use of a prostaglandin analogue (misoprostol) may be prescribed to prevent peptic ulceration due to NSAIDs.
D) The use of antacids or H2 receptor antagonist (H2RAs) such as cimetidine, ranitidine, famotidine, and nizatidine which help in the reduction of gastric acid secretion and in turn increase the gastric pH and reduce the secretion of pepsin.
E) The treatment of peptic ulcer complications includes a blood transfusion for hematemesis and melena, the use of antacids and H2 receptor antagonists for pain, the treatment of peritonitis in case of perforation of peptic ulcer disease.
Maintenance with H2 receptor antagonists is usually effective and relatively safe.
Surgery
Surgical treatment of ulcer may be indicated for patients with failure to respond to medical line of treatment or with complications such as increased pain, bleeding, obstruction and perforation.