- Alkaptonuria: National Organization for Rare Disorders (NORD) - (https://rarediseases.org/rare-diseases/alkaptonuria/)
- Ranganath LR, Jarvis JC, Gallagher JA. Recent advances in management of alkaptonuria (invited review; best practice article) J Clin Pathol. 2013; 66: 367-73. - (10.1056/NEJMoa021736.)
- Alkaptonuria: Genetics Home Reference (GHR), U.S. National Library of Medicine (NLM), National Institutes of Health (NIH), USA - (https://ghr.nlm.nih.gov/condition/alkaptonuria#)
- Zatkova A. An update on molecular genetics of alkaptonuria (AKU). J Inherit Metab Dis. 2011 Dec; 34(6):1127-36. DOI - (10.1007/s10545-011-9363-z. PMID: 21720873.)
- Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002; 347: 2111-21. DOI - (10.1056/NEJMoa021736.)
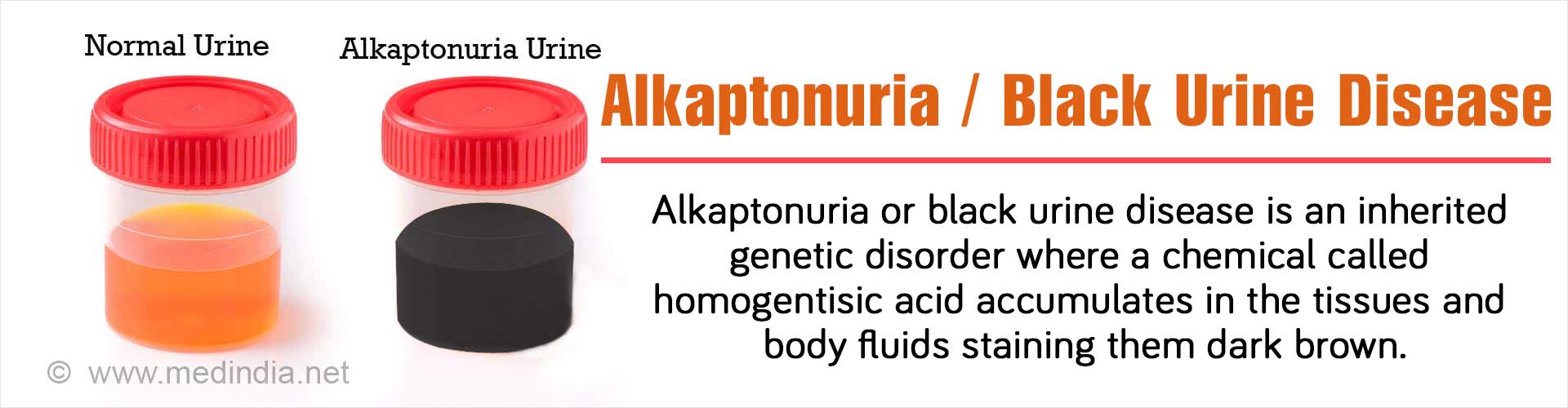
What is Alkaptonuria?
Alkaptonuria, also known as “black urine disease”, is a rare inherited disease that was first described by Sir Archibald Edward Garrod in 1902, along with three other diseases, which are all caused by metabolic abnormalities. These four diseases were originally classified as “inborn errors of metabolism”, a term coined by Garrod himself. He shared his thoughts and ideas on the subject in his celebrated Croonian Lectures held at the Royal College of Physicians in 1908.
Human Genetics & Inheritance in a Nutshell
In humans, like other living beings, all the information is stored in structures called genes, which are located within the nucleus of cells. These genes are made up of a chemical called DNA (deoxyribonucleic acid), which is present in the form of double strands with rungs, much like a ladder. But the only difference is that unlike a ladder, the DNA molecule is twisted into a helix.
These genes, consisting of DNA, are inherited in pairs called “alleles”, one from the mother and one from the father. Once transferred to the offspring, the properties of these genes are said to be inherited.
These genes are responsible for producing all the proteins in the cells that carry out a multitude of functions. This is the basis of human inheritance. However, in certain situations, the DNA sequence of these genes can be rapidly and randomly changed, which is termed as “mutation”. A mutated gene is said to be defective as it produces a defective protein that cannot perform its normal function.
Genetic Basis of Alkaptonuria
- Alkaptonuria is a disease where a specific gene – homogentisate 1,2-dioxygenase (HGD) – is mutated, giving rise to the corresponding defective HGD enzyme.
- In this disease, the body cannot properly metabolize phenylalanine and tyrosine, which are two of the 20 amino acids (building blocks of proteins) leading to accumulation of homogentisic acid, one of the by-products of their metabolism.
- Homogentisic acid (HGA) and its oxidized product benzoquinone acetic acid (BQA), commonly known as “alkapton” are excreted in the “urine” – hence the name “Alkaptonuria”.
- In this condition, the patient’s urine exhibits a characteristic black color upon exposure to air.
Alkaptonuria is inherited as an autosomal recessive trait (characteristic). Recessive genetic disorders occur when a person inherits the same abnormal gene for the same trait from both the parents. This means that in order to get the disease, both the parents must have a copy of the defective gene, which in this case is the HGD gene. However, if that person receives a functional gene from one parent and a defective gene from the other, then he/she will be a carrier of the disease but will not exhibit any symptoms. Thus, both parents will be carriers of the gene but do not suffer from the condition.
Epidemiology of Alkaptonuria
The prevalence of alkaptonuria in most populations varies between 1 in 100,000 to 1 in 250,000 people. However, in certain countries such as Slovakia, the Dominican Republic and Germany, its incidence is much higher. For example, in Slovakia the incidence is as high as 1 in 19,000 people. Scientists have found that the underlying reason for this higher incidence is due to occurrence of up to 12 mutations simultaneously in the HGD gene, instead for the usual single mutation.
What are the Causes of Alkaptonuria?
Alkaptonuria is caused by mutations in the HGD gene, which encodes the enzyme homogentisate 1,2-dioxygenase (HGD). This enzyme helps breakdown the amino acids phenylalanine and tyrosine, which are important building blocks of proteins. Mutations in the HGD gene produce a defective HGD enzyme, which hampers its role in the breakdown of phenylalanine and tyrosine. This results in the accumulation of HGA, which is an intermediate product of phenylalanine and tyrosine metabolism. From early childhood, this acid is excreted in the urine, which has a characteristic black color. Homogentisic acid slowly accumulates in the connective tissues, which causes darkening of the skin and cartilage. Over time, usually after reaching adulthood, the affected tissues can become blue-black in color. Moreover, a build-up of HGA in the joints leads to osteoarthritis.
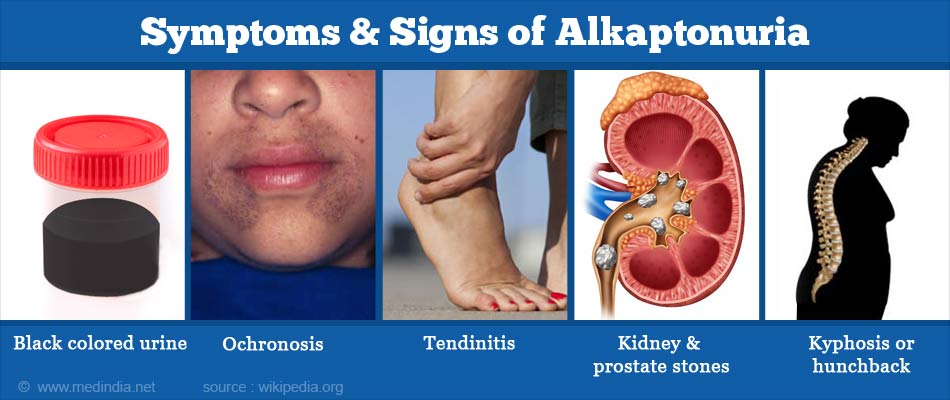
What are the Symptoms and Signs of Alkaptonuria?
There are several symptoms and signs of alkaptonuria, which are briefly highlighted below:
- Black Colored Urine: Urine becomes black in color upon exposure to air. Sweat and earwax can also exhibit a black color.
- Ochronosis: This occurs due to deposition of HGA in the connective tissues, especially cartilages. The cartilage of the ear lobes can become thickened, irregular and blue, grey or black in color. Dark spots can also occur on the sclera (whites of the eyes).
- Tendinitis: The tendons can become thickened, inflamed and painful, technically termed as tendinitis. The thickened Achilles tendon is especially prone to tearing or rupturing. Eventually, discoloration of the tendons can become visible on the overlying skin.
- Kidney & Prostate Stones: Kidney stones can develop in 50% of affected individuals over 64 years of age. Men with alkaptonuria may also develop prostate stones. Passage of these black stones can be extremely painful.
- Ochronotic Arthropathy: There can be chronic joint pain and inflammation (arthritis). When the spine and large joints such as the hips and knees are affected, it is technically termed as ochronotic arthropathy.
- Ankylosis & Kyphosis: Intervertebral discs can flatten, calcify and eventually fuse. This can result in ankylosis, (a condition where the affected joints become stiff and immobile). Moreover, kyphosis or hunchback may occur, where there is an excessive convex curvature of the spine.
- Stiffening of Heart Valves: Accumulation of HGA within the aortic or mitral valves can cause thickening of the valves and narrowing (stenosis) of their openings due to calcification. In some cases, calcification of the coronary blood vessels may also occur.
How do you Diagnose Alkaptonuria?
Alkaptonuria can be suspected in an adult if the urine turns black upon exposure to air. In case of babies, diapers having black stains due to drying of urine can be indicative of alkaptonuria. Moreover, a thorough family history can reveal the likelihood of occurrence of alkaptonuria in an individual. However, there are some definitive tests that can clinch the diagnosis for alkaptonuria. These are highlighted below:
- Detection of Homogentisic Acid in Urine: A 24-hour urine sample can be tested by gas chromatography-mass spectrometry to detect the presence and quantify the amount of HGA in the urine.
- Molecular Genetic Testing: Molecular techniques such as the polymerase chain reaction (PCR) can be used to detect the presence of mutations in the HGD gene in urine or tissue samples. This is the ultimate confirmatory test.
How do you Treat Alkaptonuria?
There are very few options for the treatment of alkaptonuria. Since there are currently no licensed medicines for alkaptonuria, the main focus is providing symptomatic relief, preventive measures, and supportive care. Some of the treatment strategies are briefly highlighted below:
- Ascorbic Acid: Large doses of ascorbic acid (vitamin C) has sometimes been recommended for the treatment of alkaptonuria since it prevents the accumulation of HGA in the tissues. However, research studies have shown that long-term use of ascorbic acid is generally ineffective for the treatment of this condition.
- Nitisinone: A new drug named nitisinone is under investigation as a potential treatment for alkaptonuria. Nitisinone is classified as an orphan drug by the United States Food and Drug Administration (USFDA) and has been approved for the treatment of a metabolic disorder known as tyrosinemia. Studies have shown that nitisinone therapy can reduce plasma and urinary HGA by more than 95%. The main drawback is the accumulation of tyrosine, the long-term risks of which are unknown.
- Diet: Dietary restriction of protein may help in reducing the intake of phenylalanine and tyrosine, thereby slowing the progression of the disease by reducing the production of HGA.
- Pain Medication: Painkillers and anti-inflammatory agents such as paracetamol, ibuprofen and naproxen can help to relieve pain and swelling. Procedures like transcutaneous electrical nerve stimulation (TENS) can help in appreciably reducing pain by numbing the nerve endings of the spinal cord.
- Surgery: Surgical intervention may be necessary if joint replacement or heart valve replacement is required.
What is the Prognosis for Alkaptonuria?
The disease is progressive in nature. There is usually a slow but progressive functional decline in the patient. Complications such as arthritis in the spine, hips, shoulders and knees can develop. There is a greater propensity for the Achilles tendon to rupture and for kidney and prostate stones to develop. The aortic and mitral valves as well as the coronary arteries may become stiff and hardened. The patients experience increased pain and loss of mobility as time progresses, often requiring the use of physical mobility aids such as crutches or wheelchairs. Although cardiac complications may worsen the prognosis, life expectancy is not significantly reduced.