- Optochiasmatic arachnoiditis - (http://www.theaword.org/index.php?option=com_content&view=article&id=515:optochiasmatic-arachnoiditis)
- Cerebral arachnoiditis - (http://www.theaword.org/index.php?option=com_content&view=article&id=514:cerebral-arachnoiditis)
- Steel CJ, Abrames EL, O'Brien WT. Arachnoiditis ossificans - a rare cause of progressive myelopathy. Open Neuroimag J. 2015; 9: 13-20. doi: 10.2174/1874440001509010013
- Pasoglou V, Janin N, Tebache M, Tegos TJ, Born JD, Collignon L. Familial adhesive arachnoiditis associated with syringomyelia. Am J Neuroradiol. 2014; 35(6): 1232-1236. doi: 10.3174/ajnr.A3858
- Spinal arachnoiditis. Online Mendelian Inheritance in Man (OMIM). July 2, 2012.
- NINDS Arachnoiditis Information Page. National Institute of Neurological Disorders and Stroke (NINDS). July 8, 2015.
- Arachnoiditis. Genetic and Rare Diseases Information Center (GARD), National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), Bethesda, USA.
- Sharma A, Goyal M, Mishra NK, Gupta V, Gaikwad SB. MR imaging of tubercular spinal arachnoiditis. Am J Roentgenol. 1997;168: 807-812. doi: 10.2214/ajr.168.3.9057539
What is Arachnoiditis?
Arachnoiditis is a chronic pain disorder caused by the inflammation of the arachnoid mater, the middle layer of the three-layered meninges that cover the brain and spinal cord. The inflammation usually involves the arachnoid membrane and the subarachnoid space that surround the nerves of the spinal cord. Arachnoiditis is characterized by chronic pain accompanied by leg cramps. There may also be excruciating stinging and burning pain. Sometimes there is a shooting pain, resembling an electric shock.
Prevalence of Arachnoiditis
Arachnoiditis is a rare condition generally affecting females more than males. This increased incidence in the female population may arise from administration of epidural anesthesia during childbirth. Due to the rarity of the condition, the exact incidence and prevalence rates are unknown. Moreover, this condition often goes misdiagnosed or undiagnosed making it further difficult to estimate the prevalence.
Structure & Function of the Meninges in Brief
The brain and spinal cord are surrounded by three protective fibrous connective tissue layers, collectively called the meninges. The three membranes viewed from the outside going inwards are as follows:
- Dura mater: This is the outer tough membrane, consisting of fibrous connective tissue. It envelopes the arachnoid mater and surrounds the dural sinuses and provides support to these sinuses. The dura mater carries blood from the brain toward the heart.
- Arachnoid mater: The arachnoid mater is located between the outer tough dura mater and the inner delicate pia mater. The arachnoid mater is attached to the inner part of the dura mater and surrounds the brain and spinal cord. The space between the arachnoid mater and pia mater is called the subarachnoid space and contains cerebrospinal fluid (CSF).
- Pia mater: The pia mater is the innermost delicate layer of the meninges. It firmly adheres to the surface of the brain and spinal cord. It is a very thin membrane that is composed of fibrous tissue and covered on the outer surface by an impermeable sheet of flat cells.
What are the Types of Arachnoiditis?
There may be several types of arachnoiditis, which can be classified in various ways. As per the National Organization for Rare Disorders (NORD), arachnoiditis can be divided into the following types:
- Adhesive Arachnoiditis: This type of arachnoiditis is very serious, where scar tissue formation occurs. Compression of the nerve roots also occur. Moreover, the normal flow of CSF is greatly hampered.
- Arachnoiditis Ossificans: This is a complication that occurs at the last stage of adhesive arachnoiditis. This rare type of myelopathy results in replacement of parts of the spinal arachnoid with bony deposits.
- Cerebral Arachnoiditis: This is so called because it affects the brain. Infections are the most common cause of cerebral arachnoiditis. Mechanical injury, cancer, hemorrhage and contrast dyes can also cause this type of arachnoiditis.
- Hereditary Arachnoiditis: Arachnoiditis is generally not hereditary in nature. This type of arachnoiditis has so far been reported in the literature to have occurred in two families with many affected family members, possibly due to interaction between multiple genes.
- Neoplastic Arachnoiditis: Neoplastic arachnoiditis is associated with cancer. It is primarily caused by chronic infection or due to underlying inflammatory conditions.
- Optochiasmatic Arachnoiditis: This is an abnormal thickening of the arachnoid in the region of the optic nerves and the optic chiasm. The optic chiasm is the junction between the two optic nerves. Arachnoiditis in this area can arise due to bacterial (tuberculosis) or parasitic (tapeworm) infections. Viral infections (encephalitis) have also been implicated in optochiasmatic arachnoiditis.
- Postmyelographic Arachnoiditis: Myelography is a diagnostic imaging procedure that uses a contrast dye and X-rays or computed tomography (CT) to look for problems in the spinal canal, including the spinal cord and nerve roots. When a person suffers from arachnoiditis following a myelography where contrast dyes like metrizamide or meglumine iocarmate are injected, it is known a postmyelographic arachnoiditis.
- Rhinosinusogenic Cerebral Arachnoiditis: This is a subtype of cerebral arachnoiditis that is associated with inflammation of the soft tissues that line the sinuses, technically termed as rhinosinusitis.
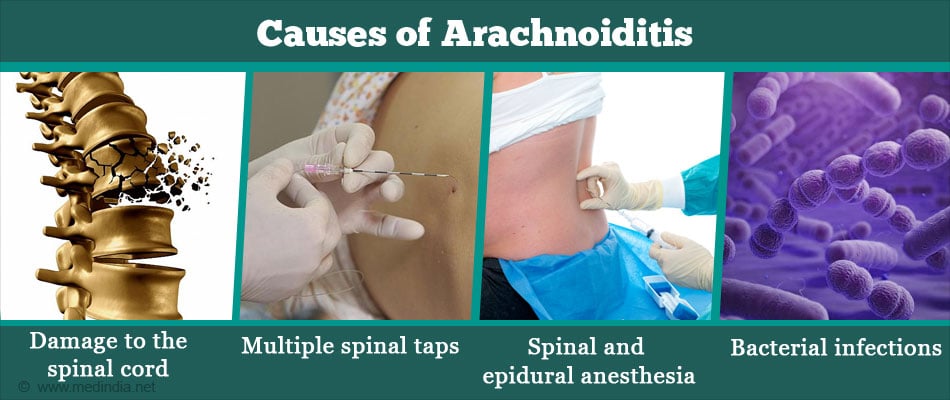
What are the Causes of Arachnoiditis?
Arachnoiditis may be caused by several factors, some of which are listed below:
- Mechanical Injury: This can occur during spinal surgery, or complications from spinal surgery (about 60% of cases).
- Trauma: Damage to the spinal cord.
- Spinal Tap: Multiple spinal taps.
- Injections: Epidural injections of steroids or other drugs.
- Anesthesia: Spinal and epidural anesthesia.
- Myelography: Arachnoiditis can occur after a myelography procedure.
- Infections: Bacterial (tuberculosis), viral (encephalitis) or parasitic (tapeworm) infections of the spinal cord and brain.
What are the Symptoms and Signs of Arachnoiditis?
Arachnoiditis can cause a number of symptoms including the following:
- Numbness
- Tingling
- Loss of temperature sensation
- Stinging and burning pain in the lower back, limbs, and trunk
- Loss of balance
- Tinnitus
- Vision and hearing problems
- Bladder and bowel problems
- Sexual dysfunction
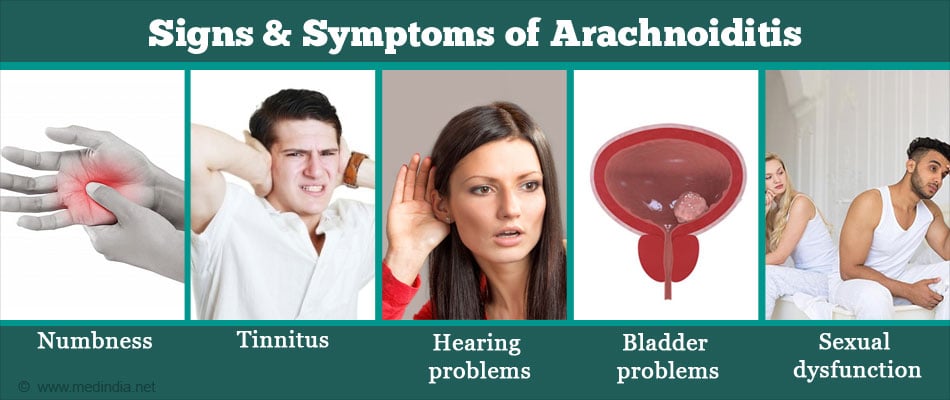
It should be noted that the pain can be aggravated by any type of movement. There may also be severe muscle cramps or spasms. Moreover, severe cases of arachnoiditis may lead to paralysis of the lower limbs.
What are the Risk Factors of Arachnoiditis?
The major risk-factors of arachnoiditis are briefly highlighted below:
- Bacterial, viral, fungal or parasitic infections that spread to the brain and spinal cord.
- Diseases that weaken the immune system e.g. diabetes, AIDS, alcoholism, and organ transplantation.
- Complications arising from brain or spinal surgery.
- Anesthetics, steroids and contrast media administered intrathecally i.e. into the subarachnoid space.
- Cancers such as melanoma, non-Hodgkin’s lymphoma, breast cancer, lung cancer as well as other cancers specific to the brain.
How do you Diagnose Arachnoiditis?
Diagnosis of arachnoiditis can be done by using the under-mentioned strategies:
- Patient History: A detailed medical history of the patient is important for acquiring and assessing all the relevant information that may have an impact on the diagnosis.
- Clinical Examination: The patient is examined by the neurologist for any physical signs and symptoms that might help in the diagnosis.
- Magnetic Resonance Imaging (MRI): MRI is the investigation of choice for diagnosing arachnoiditis. An MRI scan uses a strong magnetic field and radio waves to create pictures, on a computer, of tissues, organs and other structures inside the body.
- Computed Tomography (CT) Scan: This technique uses X-rays to take photos of the body part under investigation and uses a computer to process the images to produce cross-sectional images or slices of that body part. This technique can be used along with myelography to increase the clarity of the images.
- Myelography: It is a diagnostic imaging procedure that uses a contrast dye (metrizamide / meglumine iocarmate) in conjunction with CT scanning to look for problems in the spinal canal, including the spinal cord and nerve roots. This can be used to obtain fine details of the arachnoid mater and associated structures so that any abnormalities can be detected.
How do you Treat Arachnoiditis?
There is currently no cure for arachnoiditis. Arachnoiditis does not have a specific treatment plan. Management of arachnoiditis is done symptomatically. Treatment options are similar to those for other chronic pain conditions, which aims to relieve pain and improve symptoms that impair function, so that the patient can perform the daily activities. Treatment may include the following:
- Oral medicines such as painkillers, non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants for controlling pain.

- Physical therapy for reducing pain and improving functionality.
- Psychotherapy for overcoming depression.
Surgical treatment is contraindicated because it does not offer long-term relief and can lead to excessive scar tissue formation, which can worsen the condition.
How do you Prevent Arachnoiditis?
The following simple strategies could be adopted to prevent the occurrence of arachnoiditis:
- The necessity for invasive surgery should be avoided unless absolutely required and there is no other alternative.
- Women could opt for natural childbirth, which usually does not require epidural administration of anesthesia.
- Avoid unnecessary investigative techniques that may be invasive, involving injection of drugs, dyes, chemicals and other substances.