- Auto-Brewery Syndrome - (https://www.ncbi.nlm.nih.gov/books/NBK513346/)
- What Exactly Is Auto-Brewery Syndrome? - (https://alcohol.org/co-occurring-disorder/auto-brewery-syndrome/)
About
Auto-brewery syndrome, also known as gut fermentation syndrome, is a condition characterized by the internal production of ethanol via endogenous fermentation conducted by fungi or bacteria within the gastrointestinal (GI) system, oral cavity, or urinary system(1✔ ✔Trusted Source
Auto-Brewery Syndrome
Go to source).
Contrary to conventional alcohol ingestion, individuals afflicted with ABS display symptoms resembling alcohol intoxication, even though they vehemently deny consuming any alcoholic beverages. This complexcondition is frequently associated with a dietary regimen rich in sugars and carbohydrates(2✔ ✔Trusted Source
What Exactly Is Auto-Brewery Syndrome?
Go to source).
Causes of Auto-Brewery Syndrome
1. Fermenting Microorganisms
The primary causative agents of ABS are fermenting yeasts and bacteria residing within the body. Fungal strains such as Candida albicans, Candida glabrata, Saccharomyces cerevisiae, and others possess the enzymatic machinery necessary for fermenting dietary sugars and carbohydrates into ethanol.
2. Dietary Factors
A diet high in sugars and carbohydrates provides ample substrate for fermenting microorganisms to thrive. Excessive consumption of sugary and starchy foods creates an environment conducive to the overgrowth of fermenting yeasts and bacteria, thereby increasing ethanol production.
3. Antibiotic Use
The administration of antibiotics can disrupt the balance of microorganisms within the gastrointestinal tract, leading to dysbiosis. Antibiotics indiscriminately target both harmful and beneficial bacteria, creating an opportunity for fermenting microorganisms to proliferate unchecked.
4. Underlying Medical Conditions
Diabetes: Individuals with diabetes often exhibit alterations in gut microbiota composition and function, predisposing them to dysbiosis. Additionally, fluctuations in blood glucose levels provide fermenting microorganisms with ample substrate for ethanol production.
Liver Dysfunction: Liver diseases, such as cirrhosis or fatty liver disease, impair hepatic metabolism and clearance of ethanol. Inadequate ethanol metabolism exacerbates the effects of ABS, leading to heightened blood alcohol levels and associated symptoms.
5. Immunocompromised States
Individuals with compromised immune systems, such as those undergoing immunosuppressive therapy or living with HIV/AIDS, are more susceptible to infections by fermenting microorganisms. Immunodeficiency creates an environment conducive to microbial overgrowth and dysbiosis.
6. Gastrointestinal Disorders
Conditions affecting the structure or function of the gastrointestinal tract, such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), or gastroparesis, can disrupt normal gut microbial ecology. Altered gut motility, mucosal integrity, and immune responses contribute to dysbiosis and the pathogenesis of ABS.
7. Genetic Predisposition
Although less understood, genetic factors may predispose certain individuals to ABS. Polymorphisms in genes involved in host-microbe interactions, immune responses, or ethanol metabolism could influence susceptibility to fermenting microorganism colonization and subsequent ethanol production.
Biochemical Mechanisms of Auto-Brewery Syndrome (ABS)
The biochemical mechanisms that leads to to the production of ethanol, carbon dioxide, and other metabolic byproducts are as follows:
- Formation of Pyruvate: Sugars, such as glucose, are broken down into pyruvate through biochemical pathways like the Embden-Meyerhof-Parnas (EMP) or Entner-Doudoroff (ED) pathway, depending on the microorganism involved.
- Decarboxylation to Acetaldehyde: Pyruvate is then converted to acetaldehyde via the action of pyruvate decarboxylase, releasing carbon dioxide as a byproduct.
- Reduction to Ethanol: Acetaldehyde is further reduced to ethanol by alcohol dehydrogenase, accompanied by the oxidation of nicotinamide adenine dinucleotide (NADH) to nicotinamide adenine dinucleotide (NAD+), which replenishes the cell's NAD+ pool.
- First Pass Metabolism: Ethanol produced through fermentation undergoes first-pass metabolism primarily in the liver. Alcohol dehydrogenase converts ethanol to acetaldehyde, which is then metabolized into acetate by aldehyde dehydrogenase, ultimately detoxifying ethanol and reducing its systemic effects.
In ABS, there is an imbalance between ethanol production and breakdown, leading to elevated blood alcohol levels. Factors such as underlying medical conditions (e.g., diabetes, obesity, liver diseases) or dietary habits high in sugars and carbohydrates exacerbate this imbalance, contributing to heightened ethanol production and subsequent intoxication.
Symptoms and signs of Auto-Brewery Syndrome
Auto-brewery syndrome manifests through a spectrum of symptoms and signs that closely mimic those of alcohol intoxication.
- Dizziness: Individuals may experience a sensation of lightheadedness or unsteadiness, making it difficult to maintain balance and coordination.
- Disorientation: Confusion and cognitive impairment can occur, leading to difficulties in understanding surroundings or processing information.
- Headache: Headaches are commonly reported, often accompanied by sensations of pressure or throbbing discomfort.
- Nausea: Feelings of queasiness or an urge to vomit may arise, contributing to gastrointestinal discomfort.
- Fatigue: Chronic fatigue syndrome may develop, characterized by persistent feelings of tiredness, lethargy, and decreased energy levels.
- Anxiety and Depression: Psychological symptoms such as anxiety and depression may emerge, impacting mood and overall mental well-being.
- Red or Flushed Skin: External signs of ABS can include flushed or reddened skin, which may be mistaken for alcohol-induced vasodilation.
- Dehydration: Elevated ethanol levels can lead to dehydration due to increased urine output and impaired fluid balance regulation.
- Memory Impairment: Cognitive dysfunction, including memory impairment and difficulty concentrating, may be evident.
- Slurred Speech: Speech may become slurred or difficult to articulate clearly, resembling the effects of alcohol intoxication.
- Stumbling and Loss of Motor Functions: Impaired coordination and motor function may result in stumbling, clumsiness, or difficulty performing basic tasks.
- Belching: Excessive belching or burping may occur due to gastrointestinal disturbances associated with ABS.
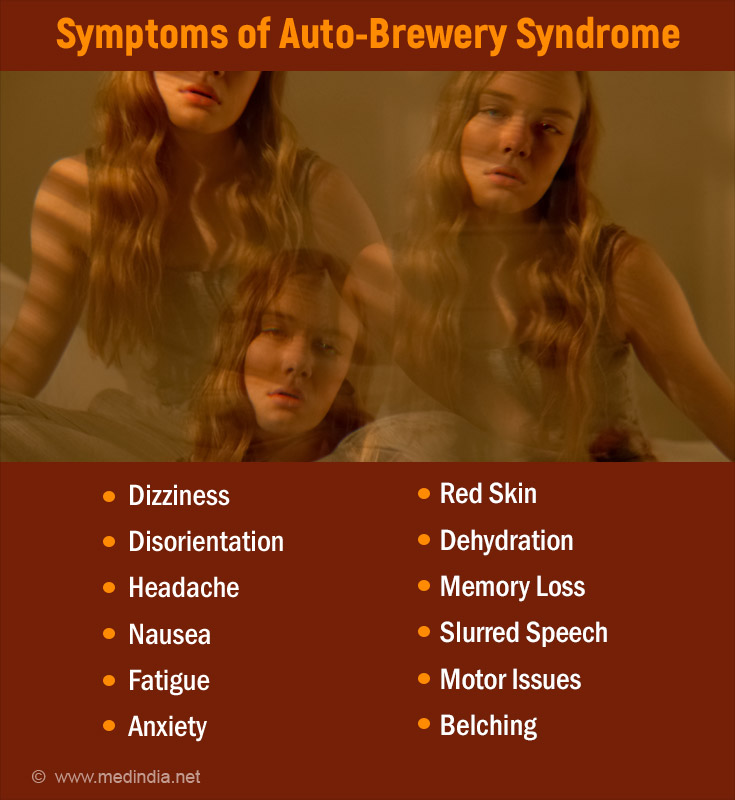
These symptoms and signs are often indistinguishable from alcohol intoxication andcan have significant implications on theaffected individuals. Legal and social ramifications may arise, as elevated blood alcohol levels can lead to impaired driving ability and misunderstanding by others.
Diagnostic Strategies for Auto-Brewery Syndrome
Diagnosing auto-brewery syndrome(ABS) requires a thorough and multi-faceted approach to ensure accurate identification and differentiation from other conditions.
1. History and Physical Examination:
A comprehensive history-taking, including information from family members regarding diet, alcohol intake, and episodes of unexplained intoxication, is crucial. Physical examination to assess for signs of alcohol intoxication and any underlying medical conditions associated with ABS.
2. Laboratory Tests:
Blood Alcohol Level (BAL): Measurement of blood ethanol concentration to assess elevated levels consistent with ABS. This may be performed using gas chromatography, serum measurements, or breathalyzers.
Metabolic Panel: Evaluation of electrolyte levels, liver function tests, and kidney function to assess for underlying metabolic abnormalities.
Complete Blood Count (CBC): To rule out hematological disorders or infections.
Drug Screen: Screening for the presence of drugs that could potentially contribute to symptoms.
Stool Culture and Sensitivity: Examination of stool samples to identify fermenting microorganisms and assess for any associated infections.
3. Carbohydrate Challenge Test:
A 24-hour observation period with a high-carbohydrate diet followed by a carbohydrate challenge involving the ingestion of a specific amount of glucose.
Blood alcohol concentration (BAC) and breath alcohol concentration (BrAC) testing are undertaken at regular intervals to monitor for elevated ethanol levels afterthe carbohydrate ingestion. ABSis confirmed if ethanol levels rise significantly during the test.
4. Endoscopic Evaluation:
Upper and lower endoscopy with sampling of gastrointestinal mucosa for culture and sensitivity testing. This helps identify fermenting microorganisms and assess for any mucosal abnormalities or infections contributing to ABS.
5. Other Considerations:
These to be considered include:
- Awareness that not all patients may present with symptoms within 24 hours, necessitating longer observation periods.
- Utilization of various methods such as gas chromatography, serum measurements, and breathalyzers to accurately quantify blood ethanol levels.
- Fasting prior to serum measurement tests to establish baseline blood alcohol and glucose levels before administering a glucose challenge.
Comprehensive Management Approaches for Auto-Brewery Syndrome
Treatment and management of auto-brewery syndrome (ABS) encompass a multi-faceted approach aimed at addressing both immediate symptoms and long-term prevention of relapses.
1. Immediate Care
Treatment of Acute Alcohol Poisoning: Patients presenting with extremely high blood alcohol levels require immediate stabilization and management to address symptoms of alcohol intoxication.
2. Drug Therapy
Prescription Medications: Based on culture and sensitivity results, targeted drug therapy may be initiated to combat identified pathogenic microorganisms. Commonly prescribed medications include antifungals such as fluconazole or micafungin for fungal infections, and antibiotics for bacterial infections. Rare or resistant microbes may necessitate the use of echinocandins or specialized antibiotics.
3. Diet Therapy
High-Protein, Low-Carbohydrate Diet: A cornerstone of ABS management involves dietary modifications to minimize the fermentation of sugars and carbohydrates into ethanol. Patients are advised to follow a high-protein, low-carbohydrate diet to reduce the substrate available for fermentation. Elimination of simple and complex sugars helps decrease alcohol production within the gastrointestinal and genitourinary tracts.
4. Supplements
Probiotics: Multistrain probiotic supplements are recommended to restore and rebalance the gut microbiome. Probiotics aid in the establishment of beneficial bacteria, preventing the overgrowth and recolonization of pathogenic microorganisms implicated in ABS. While probiotics have shown promise in ABS management, further research is needed to evaluate their efficacy as a treatment modality.
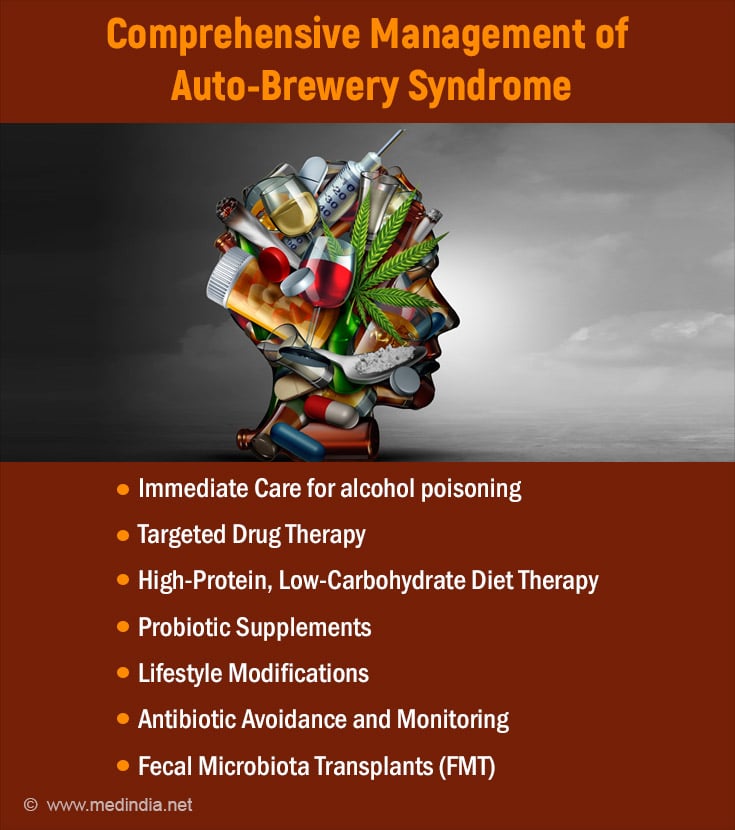
5. Lifestyle Modifications
Avoidance of Carbohydrates: Patients are advised to minimize carbohydrate intake to reduce the risk of relapse. Carbohydrate avoidance plays a crucial role in mitigating symptoms and preventing ethanol production within the body.
Nutritional Guidance: Involvement of a nutritionist is essential to provide dietary guidance and support throughout the treatment process. Nutritional counseling helps patients adhere to dietary restrictions and optimize their dietary choices for symptom management and long-term wellness.
6. Antibiotic Avoidance and Monitoring
Avoidance of Antibiotics: Whenever possible, antibiotics should be avoided to prevent disruptions to the gut microbiome and minimize the risk of exacerbating fermentation.
Monitoring and Retesting: In cases where antibiotic therapy is necessary, close monitoring and retesting for fermenting pathogens are essential to guide treatment decisions and prevent relapses.
7. Fecal Microbiota Transplants (FMT)
Long-Term Management: Patients with chronic relapses or refractory ABS may benefit from fecal microbiota transplants. FMT aims to restore microbial balance and diversity within the gut, offering a potential solution for individuals with persistent symptoms despite conventional treatments.
Differential Diagnosis
Differential diagnosis for auto-brewery syndrome (ABS) involves ruling out other potential causes of symptoms resembling alcohol intoxication.
1. Head Injury
Traumatic Brain Injury (TBI): Patients with TBI may exhibit symptoms such as confusion, dizziness, and impaired coordination, which can mimic alcohol intoxication. A thorough history of recent head trauma and neurological examination is essential to differentiate TBI from ABS.
2. Psychiatric Disorders
Certain psychiatric conditions, such as conversion disorder or somatization disorder, may manifest with symptoms resembling alcohol intoxication as a result of psychological distress. Evaluation by a psychiatrist and consideration of the patient's psychiatric history are crucial in ruling out these disorders.
3. Hidden Alcohol Consumption
Patients denying alcohol consumption may still engage in covert or surreptitious drinking, leading to elevated blood alcohol levels. Inquiring about alcohol habits and corroborating information from family members or caregivers can help identify hidden drinking as a potential cause of symptoms.
4. D-Lactic Acidosis
Metabolic Acidosis: D-lactic acidosis, characterized by elevated D-lactate levels in the blood, can result from conditions such as short bowel syndrome or carbohydrate malabsorption. Symptoms may overlap with those of ABS, necessitating consideration of metabolic acidosis in the differential diagnosis.
5. Medication Effects
Drug-Induced Intoxication: Certain medications, including sedatives, hypnotics, and anticholinergic agents, can produce symptoms resembling alcohol intoxication. Reviewing the patient's medication history and conducting a drug screen can help identify potential medication-induced effects.
6. Nutritional Deficiencies
Thiamine Deficiency: Chronic alcohol consumption and malnutrition can lead to thiamine deficiency, causing symptoms such as confusion, ataxia, and cognitive impairment. Assessing nutritional status and performing relevant laboratory tests can aid in diagnosing thiamine deficiency as a differential diagnosis.
7. Neurological Disorders
Conditions such as epilepsy, stroke, or transient ischemic attacks (TIAs) may present with transient neurological deficits resembling alcohol intoxication. Neuroimaging studies and consultation with a neurologist may be necessary to rule out these disorders.
Prognosis
Resolution with Treatment: Some patients may achieve symptom resolution by discontinuing antibiotics and adopting a sugar-free, low-carbohydrate diet. Additional interventions, such as antifungals, antibiotics, and probiotics, along with dietary modifications, may be necessary for others to manage their symptoms effectively.
Chronic Relapses: Despite treatment efforts, some individuals may experience recurrent episodes of ABS, leading to ongoing challenges in managing their condition. Chronic relapses can significantly impair quality of life and necessitate long-term therapeutic strategies.
Impact on Lifestyle: ABS can disrupt normal daily activities and social interactions, causing distress for patients and their families. Misinterpretation of symptoms as alcohol consumption may result in legal consequences, further complicating the prognosis.
Potential for Alcohol Use Disorder: Prolonged exposure to endogenous ethanol may increase the risk of developing alcohol cravings and addiction, potentially leading to alcohol use disorder. Vigilant monitoring and support may be necessary to mitigate this risk.
Complications
Social and Legal Issues: Misdiagnosis or misunderstanding of ABS as alcohol consumption can lead to social stigmatization and legal ramifications, including challenges with law enforcement and impaired interpersonal relationships.
Disruption of Lives: ABS can disrupt daily routines and activities, causing emotional strain and psychological distress for both patients and their families. Managing the condition may require significant adjustments to lifestyle and behavior.
Risk of Alcohol Addiction: Long-term exposure to endogenous ethanol may predispose individuals to alcohol cravings and dependency, increasing the likelihood of developing alcohol use disorder. This poses a significant complication that requires ongoing monitoring and support.
Postoperative and Rehabilitation Care
Ongoing Monitoring: Patients may require continuous monitoring for symptom recurrence and adherence to dietary and medication regimens. Regular follow-up appointments with healthcare providers are essential to assess treatment efficacy and address any emerging concerns.
Lifestyle Adjustments: Adopting a healthy lifestyle, including dietary modifications and stress management techniques, can support long-term symptom management and reduce the risk of relapse.
Psychosocial Support: Psychological counseling and support groups may be beneficial for individuals and families coping with the emotional impact of ABS. Addressing social and interpersonal challenges can improve overall well-being and facilitate successful rehabilitation.
In summary, auto-brewery syndrome is a rare but impactful condition characterized by the endogenous production of ethanol within the body, leading to symptoms resembling alcohol intoxication. Despite its rarity, ABS can have profound effects on individuals' lives, causing physical discomfort, legal issues, and social disruptions. Diagnosis requires a comprehensive evaluation, and management involves an interprofessional approach focusing on symptom relief, microbial balance restoration, and dietary modifications. Collaborative care among healthcare professionals is essential for optimizing outcomes and improving the quality of life for individuals with ABS.