- Updated Guidelines for Antiretroviral Postexposure Prophylaxis After Sexual, Injection Drug Use, or Other Nonoccupational Exposure to HIV—United States, 2016 - (https://www.cdc.gov/hiv/pdf/programresources/cdc-hiv-npep-guidelines.pdf)
- Risk and Management of Blood-Borne Infections in Health Care Workers - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc88939/)
- Overview - Blood-Borne Infections - (http://www.cdc.gov/bloodsafety/bbp/diseases_organisms.html)
- Bloodborne pathogens - (https://medlineplus.gov/ency/patientinstructions/000453.htm)
- Bloodborne Infectious Diseases: Hiv/Aids, Hepatitis B, Hepatitis C - (https://www.cdc.gov/niosh/topics/bbp/)
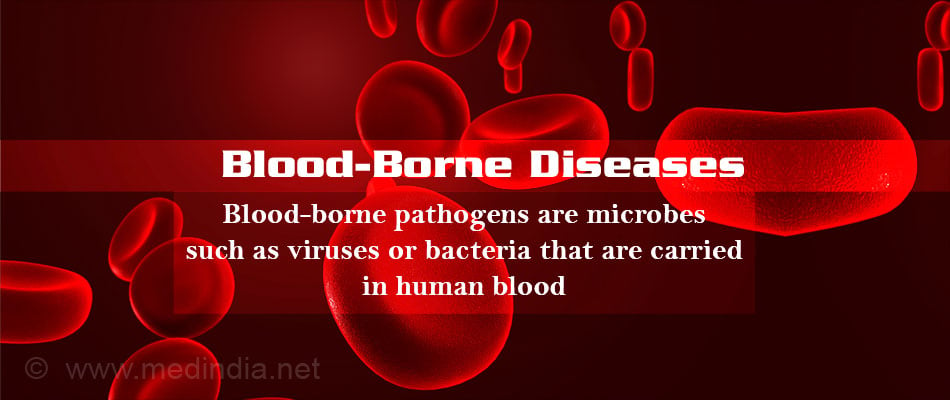
What is a Blood-Borne Disease?
A blood-borne disease is one that spreads mainly through contamination of blood and other body fluids such as semen, vaginal secretions, amniotic fluid and in some cases, saliva.
The infection may occur through transfusion of blood or blood products, sexual contact, contaminated IV drug use, occupational exposure especially in health-care workers, or from mother to the baby. The main blood-borne pathogens are the human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV).
How are Blood-Borne Infections Spread?
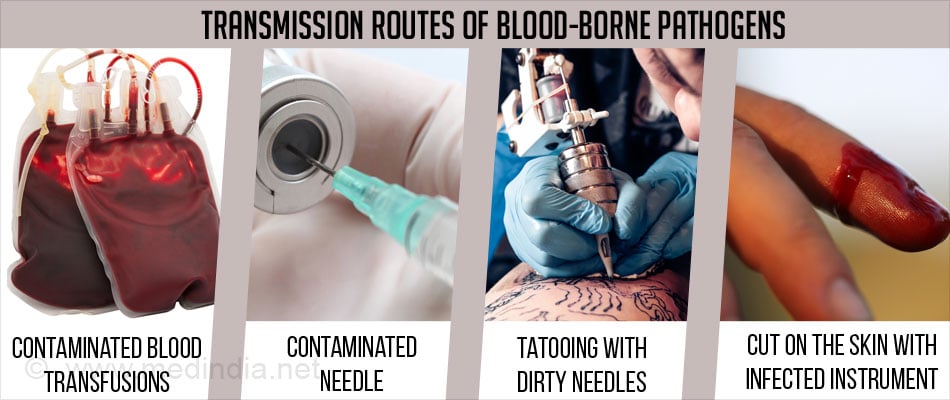
Transmission of blood-borne pathogens has been reported from patient to patient, patient to health care workers, and rarely, from health care workers to the patient. The transmission may occur due to following reasons:
- Contaminated blood transfusions - The risk of infection after receiving large volumes of infected blood, e.g., from transfusions, is extremely high.
- Percutaneous exposures - The spread of a blood-borne infection can result from an injection with a contaminated needle or a cut on the skin with any other sharp contaminated instrument. Improper disinfection or sterilization of instruments/equipment after each patient, reuse of single-use items such as needles or blades which can’t be properly cleaned and sterilized, and lack of proper regulations of procedures like skin piercing and tattooing can spread the infection.
Which are Some of the Blood-Borne Diseases?
Viral Diseases - Viral diseases like hepatitis B, hepatitis C and HIV are blood-borne infections. Cytomegalovirus and Human T-cell lymphotrophic viruses (HTLVs) are viral blood-borne pathogens. Other viral diseases that can potentially be spread through blood transfusion are listed below:
- Dengue fever (DF) - is caused by any one of four related viruses and is usually transmitted by the Aedes mosquitoes.
- Hepatitis A - is a liver disease that results from infection with the hepatitis A virus (HAV). Unlike hepatitis B and hepatitis C which are spread via blood, hepatitis A usually spreads via the feco-oral route though transmission through blood transfusion can occur.
- West Nile virus - is a potentially serious illness often transmitted through the bite of infected mosquitoes.

Bacterial Infections - Bacteria are a common cause of infections transmitted through blood transfusion. Gram positive bacteria like Staphylococcus aureus and Staphylococcus epidermidis, and gram negative bacteria like Escherichia coli can contaminate blood used for blood transfusion.
Other organisms that may rarely be spread through blood transfusion are:
Parasitic Diseases - Transmission of parasitic infections through blood donation is very rare but not impossible. Examples of parasitic diseases that can be transmitted by blood transfusion are listed below:
- Babesiosis - is caused by Babesia that infects red blood cells and is usually spread by certain ticks.
- Chagas disease - is caused by Trypanosoma cruzi, a parasite which is transmitted to animals and people by insects called triatomine bugs.
- Leishmaniasis - spreads through the bite of the sandfly, though it can also rarely spread through blood transfusion.
- Malaria - is caused by a parasite that commonly infects a certain type of mosquito which feeds on humans.
Prion Diseases - Also known as transmissible spongiform encephalopathies (TSEs), prion diseases are rare, progressive neurodegenerative disorders that affect both humans and animals. Creutzfeldt-Jakob disease (CJD), a prion disease, can spread through blood transfusion.
Diagnosis of Blood-Borne Diseases
Diagnosis of Hepatitis B Virus
Acute hepatitis B infection may take between 45 to 160 days (average 120 days) to develop following infection. Symptoms are due to the liver getting affected and include fatigue, nausea, loss of appetite, jaundice and dark urine. Hepatitis B can also cause chronic liver disease. The diagnosis depends on demonstration of certain antigens and antibodies in the blood - serum of hepatitis B surface antigen (HBsAg) that appears well before the appearance of symptoms, and immunoglobulin M (IgM) antibody to HBc, which appear along with the symptoms.
Diagnosis of Hepatitis C Virus
Acute HCV infection takes 2 to 24 weeks to develop following the viral infection, with an average of 6 to 7 weeks.. Persons with an acute infection are either asymptomatic or have an illness with symptoms of jaundice, dark urine, clay-colored stools, extreme fatigue, abdominal pain, loss of appetite and nausea. Some people develop chronic infection. Testing for HCV is done using the screening enzyme immunoassay (EIA) and supplemental immunoblot assays to detect antibodies to HCV. Anti-HCV may be positive within 5 to 6 weeks after the onset of infection and continue to be positive long after the primary infection.
Diagnosis of HIV Infection
People may not have any symptoms when first infected with HIV. They may later develop symptoms of fever, headache, fatigue, enlarged lymph nodes and weight loss. The infection is diagnosed based on the enzyme immunoassay (EIA) and the Western blot tests. HIV is considered to be negative when the EIA result is negative.
Treatment & Prevention
Prevention of HBV Infection Using Hepatitis B Vaccine
The hepatitis B vaccine appears to provide both pre-exposure protection, that is, before coming in contact with the hepatitis B virus, and post-exposure protection following contact with the virus. A protective antibody response occurs in >90% of healthy recipients of the vaccine. Hepatitis B vaccination is recommended in infancy. Post-vaccination testing for the protection given by the vaccine should be done for all HCWs who are at risk for having blood or blood-contaminated body fluid exposures.
Post-exposure Management of HCV
There is no vaccine or medication recommended of people who have been exposed to the hepatitis C virus. The exposed person should be followed up regularly and treated when necessary.
Post-exposure Management for HIV
Post-exposure preventive treatment is given to people exposed to HIV in the previous 72 hours. Healthy people exposed from non-occupational sources are prescribed a 28-day course of three anti-HIV drugs - tenofovir disoproxil and emtricitabine, along with either raltegravir or dolutegravir. A four drug regimen can also be used with includes tenofovir DF, emtricitabine, darunavir and ritonavir. Following occupational exposure, the person should be tested with the rapid HIV test. The three drug regimen of tenofovir disoproxil, emtricitabine and raltegravir is administered following occupational exposure.
Safety Measures
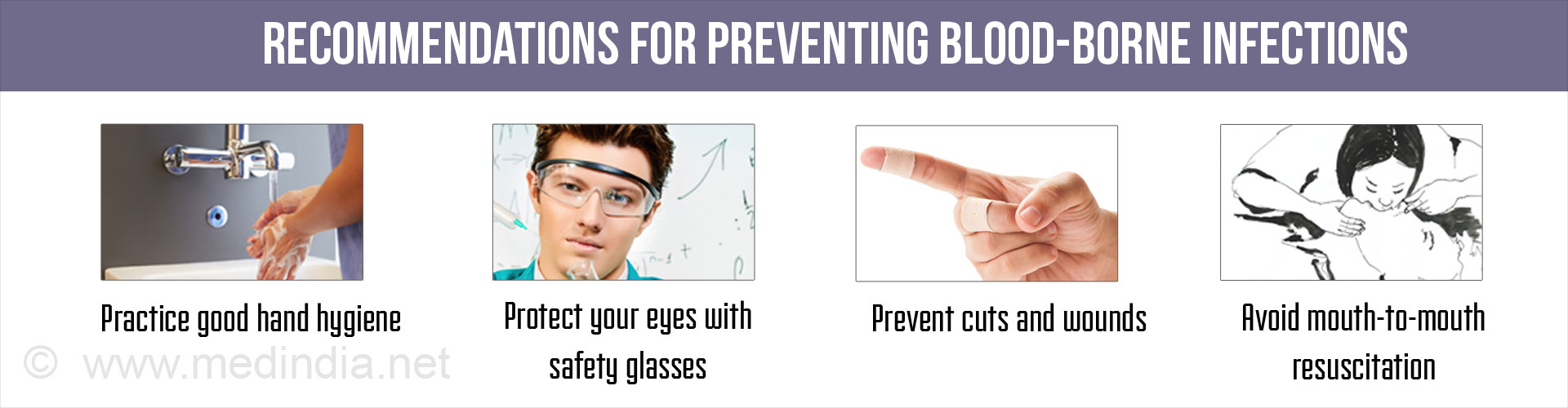
The CDC recommendations should be followed by health care workers and others prone to occupational exposure to prevent blood-borne infections:
- Observe good hand hygiene practices by washing hands with soap and water or using an alcohol-based sanitizer. Wear gloves if contact is likely with blood, body fluids, non-intact skin or mucous membranes.
- Prevent cuts and wounds especially when coming in contact with blood and any other body fluids.
- Use safety devices and avoid the use of or exposure to sharp instruments, for e.g., needles, glass and metal.
- Take particular care in handling and disposal of used / contaminated items.
- Protect the eyes and mouth by means of a goggles/safety spectacles and a waterproof mask where splashing is a possibility.
- Avoid contamination of the person or clothing by use of waterproof/water-resistant protective clothing and plastic aprons.
- Wear rubber boots when the ground is likely to be contaminated.
- Health care workers should be aware of the first aid and follow-up procedures following contamination.
- Avoid mouth-to-mouth resuscitation to revive another person. Use mouth pieces or resuscitation bags instead.
- The infection control committee of a hospital should develop and update annually all relevant protocols on prevention of spread of infection.
Risk Management of Blood-Borne Infections in Health Care Settings
The development of risk management plan and infection control strategies is essential for the prevention of transmission of blood-borne pathogens in the health care settings.
- Each hospital/institution or medical/dental practice should develop and adopt risk management policies and also monitor them for their effectiveness.
- Specialist advice in relation to occupational health, microbiology, infectious diseases and infection control should be made available to each healthcare setting.
- Infection control should be incorporated into the curriculum of medical, dental and nursing students.
- Health care institutions should keep themselves updated about developments of devices like needleless technology, which reduce the chances of blood-borne infection.
- Standard precautions should be taken with all patients in all health care facilities at all times by all staff, since an undetected blood-borne infection could be present where it is least expected.
- Hemodialysis units require specific additional precautions.

- Contact and standard precautions should be applied to patients with uncontrolled bleeding known to be positive for a blood-borne virus.