- Cholestasis - (https://medlineplus.gov/ency/article/000215.htm)
- Bile - (https://medlineplus.gov/ency/article/002237.htm)
- Heathcote EJ. Diagnosis and management of cholestatic liver disease. Clin Gastroenterol Hepatol. 2007;5:776-782.
- Hirschfield GM, Heathcote EJ, Gershwin ME. Pathogenesis of cholestatic liver disease and therapeutic approaches. Gastroenterol. 2010;139 (5):1481-1496.
- Nguyen KD, Sundaram V, Ayoub WS. Atypical causes of cholestasis. World Journal of Gastroenterology: WJG. 2014;20(28):9418-9426. doi:10.3748/wjg.v20.i28.9418.
- Assy N, Jacob G, Spira G, Edoute Y. Diagnostic approach to patients with cholestatic jaundice. World Journal of Gastroenterology. 1999;5(3):252-262. doi:10.3748/wjg.v5.i3.252.
- Lee WC et al. Adrenal insufficiency insufficiency associated with cholestatic jaundice: A case report. Int J Gerontol. 2017.
- EASL. EASL Clinical Practice Guidelines: Management of cholestatic liver diseases. J Hepatol. 2009;51:237-267.
- Clemente MG, Dessanti A (2016) Emergencies in Neonatal Management: Jaundice and Biliary Atresia. J Pediatr Neonatal Care 4(4): 00147. DOI: 10.15406/jpnc.2016.04.00147.
- Hengstler, J. G. (2017), The ascending pathophysiology of cholestatic liver disease. Hepatology, 65: 722-738. doi:10.1002/hep.28965.
What is Cholestatic Jaundice?
Cholestasis is a Greek word that means stopping or slowing of bile flow from the liver to the small intestine due to a block (obstruction) in the biliary duct system that connects the liver and small intestine, causing the bile to remain in the liver. It is therefore a form of obstructive jaundice.
Normal Flow Of Bile From Liver To Small Intestine – An Overview of The Biliary System
- The bile ducts within the liver (intrahepatic bile ducts) contain the bile formed in the liver. These intrahepatic ducts join together and exit the liver as the right and left hepatic ducts, forming the first part of the extrahepatic (outside the liver) biliary system.
- The right and left hepatic ducts join together to form the common hepatic duct.
- The common hepatic duct is joined by the cystic duct from the gall bladder. The point where the cystic duct meets the common hepatic duct marks the start of the common bile duct.
- The common bile ducts travels for a distance and empties into the second part of the duodenum (part of the small intestine) via the ampulla of Vater.
- The common bile duct is usually joined to the main pancreatic duct just prior to the opening in the ampulla.
Bile is important in the digestion of fats in the small intestine, and consequently this becomes affected. When bile remains in the liver, bilirubin, a pigment occurring in bile escapes and accumulates in the blood resulting in symptoms of jaundice. Jaundice is one of the most discerning features of cholestasis and yet it may not always be the first discernible symptom.
Cholestasis affects both the young and old. Primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC) are the main cholestatic liver conditions in adults while in infants, biliary atresia and Alagille syndrome mainly cause cholestasis.
Cholestasis observed in infants and children (1 out of 2500) can be either congenital (at birth) or hereditary.
Jaundice that occurs due to cholestasis mainly occurs in acute or acute-on-chronic cases. It is rare to observe jaundice in severe longstanding chronic cases since they are treated with liver transplants.
What are the Causes of Cholestatic Jaundice?
Cholestatic jaundice can be broadly classified according to the type of pathology in the biliary system
| Type of Biliary System Pathology | Common Examples |
| Congenital |
|
| Inflammatory |
|
| Obstruction |
|
| Neoplastic |
|
| External compression of CBD | Lymph nodes, tumor (Mirizzi’s syndrome) |
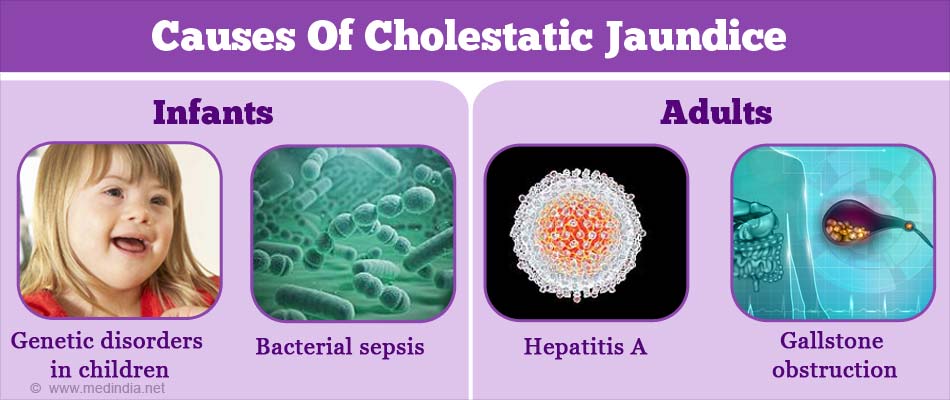
Cholestatic jaundice in infants may be caused by several factors, such as -
- Congenital hypopituitarism
- Adrenal insufficiency in infants (very rare) – This has not been observed in adults
- Rare genetic disorders in children – Accounts for 25% of cholestatic jaundice cases caused by gene mutations
- (e.g. Progressive familial intrahepatic cholestasis; Alagille syndrome; Bile acid synthesis disorders; Cystic fibrosis; Alpha-1-antitrypsin deficiency; metabolic errors; zinc storage disorders)
- Biliary atresia – accounts for 25% to 40% of cases in the initial months of life
- Bacterial sepsis
- Galactosemia
- Bile acid synthesis disorders
- Tyrosinemia
In adults, there are intrinsic and extrinsic factors pertaining the liver, which can cause cholestatic jaundice -
- Infections
- (e.g. viral hepatitis A, B, C; rubella, syphilis, herpes virus; toxoplasmosis; cytomegalovirus, AIDS, PBC, alcoholic hepatitis, autoimmune hepatitis, PSC, autoimmune cholangitis)
- Infiltrative conditions
- (e.g. fatty liver, granulomatous hepatitis, lymphoma, sarcoidosis
- Structural conditions – choledocholithiasis (gallstone obstruction with inflammation), intralobular duct destruction
- Medications e.g. estrogen, erythromycin, statins, nitrofurantoin, sulindac, cimetidine, gold salts
- Surgical complications leading to biliary ductal strictures and scarring
- Graft-versus-host disease
- Third trimester of pregnancy (obstetric cholestasis)
- Cystic fibrosis
- Tumors – gallbladder carcinoma, cholangiocarcinoma, pancreatic tumors, ampullary tumors
- Vanishing bile duct syndrome – rare condition occurring due to drug induced liver damage
What are the Signs and Symptoms of Cholestatic Jaundice?
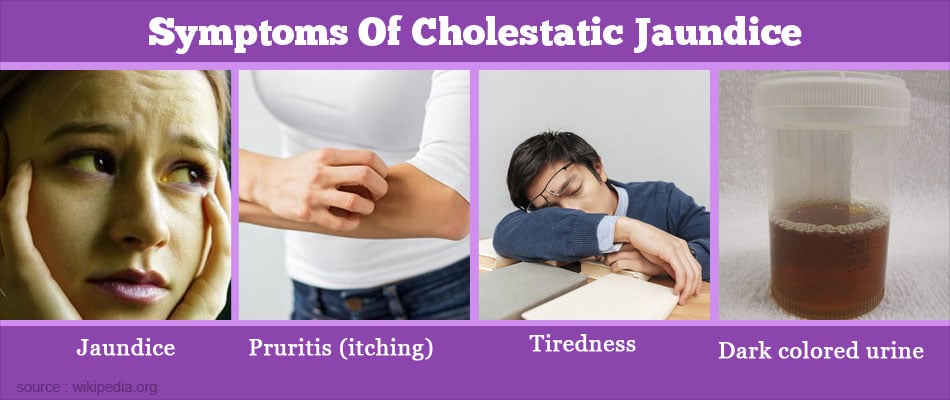
Jaundice due to cholestasis is one of the symptoms. Sometimes, prior to jaundice setting in, the patient may show certain signs indicating potential cholestasis. Clinically, cholestasis may present with the following symptoms -
- Pruritis (itching) due to deposition of bile products in the skin
- Tiredness, loss of appetite, nausea due to liver disease
- Pale-coloured stools (since bile and associated pigment does not reach the intestine)
- Deficiency of fat-soluble vitamins (since bile is needed to absorb fat soluble vitamins)
- Steatorrhea (presence of undigested fat in the stools)
- Urine is dark in colour (since urine is a filtrate of blood in which the bile pigment accumulates)
- Loss of weight due to associated cancer as well as impaired digestion
- Bone pain due to calcium and vitamin D deficiency (poor absorption of fat soluble vitamins)
- Increased bruising or bleeding due to vitamin K deficiency (poor absorption of fat soluble vitamins)
What are the Risks Factors of Cholestatic Jaundice?
During diagnosis, it is essential to evaluate the risk factors of the patient, which may have triggered the onset of cholestatic jaundice.
- Medications such as estrogens, erythromycin, NSAIDs, alcohol, Cimetidine and Itraconazole
- Premature babies
- Alcoholism
- Previous history of liver disease
- Pregnancy (obstetric cholestasis)
- Family history is considered in the case of benign recurrent intrahepatic cholestasis
How do you Diagnose Cholestatic Jaundice?
Cholestatic jaundice is diagnosed by blood tests, imaging techniques, and liver biopsy.
In order to diagnose cholestatic jaundice, it is imperative to first assess the cause of cholestasis; is it due to an intrahepatic (within the liver) condition (predominantly chronic) or an extrahepatic condition (external to the liver). The doctor will assess the patient’s symptoms and perform a thorough a physical examination of the patient. Following are the strategies employed (in the order provided) to confirm diagnosis of cholestasis.
Blood Tests
- Elevated serum bilirubin levels indicate the severity of jaundice but are not useful in determining the cause of cholestasis
- High levels of the enzyme gamma glutamyltransferase (GGT) and alkaline phosphatase
- High serum transaminase levels observed in intrahepatic cholestasis of pregnancy (ICP)
Imaging
If the blood tests are abnormal, imaging studies are done to determine the etiology of cholestatic jaundice.
- Ultrasonography of the abdomen is an effective, inexpensive, specific, and sensitive tool to distinguish between intrahepatic or extrahepatic cause of cholestasis.
- Computed tomography (CT) and magnetic resonance imaging (MRI) may be done instead of or in addition to ultrasound imaging. These may show the location and extent of cancer or other diseases. Abnormalities detected help to formulate the required therapy.
Other Biochemical tests
Negative data from ultrasound necessitates other diagnostic tests. Antimitochondrial antibodies (AMA) are diagnostic of PBC. Fibrosis or beaded appearance of the biliary system (bile production) is indicative of primary sclerosing cholangitis (PSC).
Liver biopsy
If the investigations point to a cause within the liver, a liver biopsy may be useful in establishing the diagnosis such as bile duct carcinoma (cholangiocarcinoma) or autoimmune disease. A liver biopsy also helps to confirm the diagnosis of vanishing bile duct syndrome, a common cause of drug induced cholestatic liver disease
Advanced Imaging Tests
Abnormalities of the bile duct and biliary system , including sclerosing cholangitis (SC) can be observed with advanced imaging tools, such as endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), and magnetic resonance cholangiopancreatography (MRCP)
- Endoscopic retrograde cholangiopancreatography (ERCP): A thin flexible tube (endoscope) is passed through the mouth and into the small intestine. Then, a radiopaque contrast agent (which can be seen on x-rays) is injected through the tube into the bile and pancreatic ducts (biliary tree) and x-ray images are taken.
- Magnetic resonance cholangiopancreatography (MRCP): MRCP is MRI of the biliary tree (bile and pancreatic ducts), with specialized techniques that to make the fluid in the ducts appear bright against a surrounding dark background.
- Endoscopic ultrasonography: An ultrasound probe is inserted with a flexible viewing tube (endoscope) through the mouth and into the small intestine and images are taken.
- Percutaneous transhepatic cholangiography: A long needle is inserted through the skin into the liver and then a radiopaque contrast agent is injected into a bile duct in the liver, using ultrasonography for guidance.
How do you Treat Cholestatic Jaundice?
Treatment of cholestatic jaundice has to take into account the reason behind the retention of bile in the liver and bloodstream and the effect of diminished quantities of bile acids in the digestive tract.
- Autoimmune cholangitis is treated with corticosteroids while bacterial cholangitis can be treated with antibiotics

- Cholestyramine a bile acid binding resin to symptomatically treat pruritis
- Supplements of vitamin D and K
- Ursodeoxycholic acid (UDCA) is a bile acid that improves the functioning of the liver by enhancing the flow of bile. The use of UDCA is effective in treating PBC. Corticosteroids are effective only in treating early stages of PBC since osteoporosis may result in the advanced stages of the disease . Chenodeoxycholic acid and cholic acid are used to treat bile acid synthesis disorders in infants
- Surgery is effective in treating only extrahepatic blocks to bile ducts
- Glucocorticoids can be used to treat cholestatic jaundice caused by adrenal insufficiency
How do you Prevent Cholestatic Jaundice?
Patients are advised to discontinue medications or alcohol that may be the cause of the condition.