- About Liver Transplantation - (http://my.clevelandclinic.org/health/articles/liver-transplantation)
- Liver Awareness Month... 13 Ways To Have A Healthy Liver - (http://www.liverfoundation.org/education/liverlowdown/ll1013/13ways/)
- Liver Transplant - (https://www.niddk.nih.gov/health-information/liver-disease/liver-transplant)
- Liver Transplant Preparation - (https://www.ucsfhealth.org/conditions/liver_transplant/signs_and_symptoms.html)
- Reasons for Liver Transplantation - (http://www.lahey.org/departments_and_locations/departments/transplantation/liver_transplant/reasons-for-liver-transplant/)
- Liver Transplant Overview - (http://www.mayoclinic.org/tests-procedures/liver-transplant/home/ovc-20211840)
- Duffy JP et al. Liver Transplantation Criteria For Hepatocellular Carcinoma Should Be Expanded; A 22-Year Experience With 467 Patients at UCLA. Ann Surg. 2007 Sep; 246(3): 502–511. - (doi: 10.1097/SLA.0b013e318148c704)
- Schöning W, Schmeding M, Ulmer F, Andert A and Neumann U. Liver Transplantation for Patients with Cholestatic Liver Diseases. Viszeralmedizin. 2015 Jun; 31(3): 194-198. - (doi: 10.1159/000431017)
- Varma V, Mehta N, Kumaran V, Nundy S. Indications and Contraindications for Liver Transplantation. International Journal of Hepatology
Introduction to Liver
The liver is the largest organ within the body and weighs 800-900 gm in the adult. It is situated on the upper right side of the abdominal cavity behind the lower part of the rib cage. It consists of a larger right and a smaller left lobe.
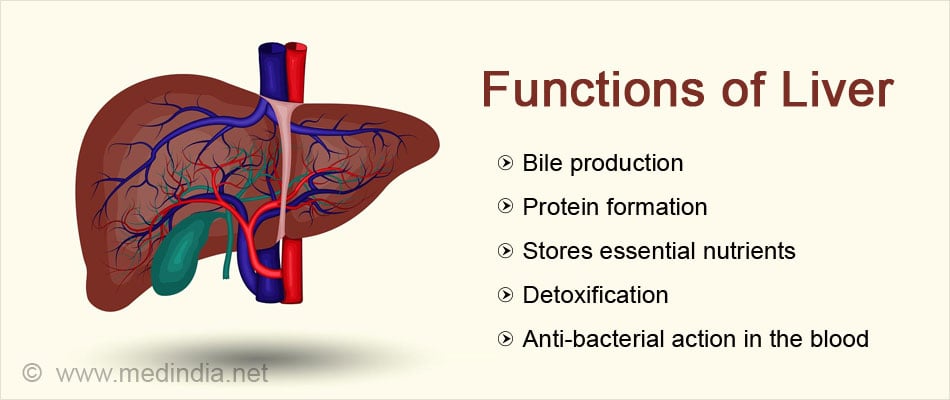
The liver performs several important functions, many of which are necessary for survival.
Functions of the liver include:
- Bile production which is necessary for the absorption of fat and fat-soluble vitamins A, D, E and K
- Formation of several proteins including albumin and immunoglobulins that are necessary for proper body function
- Storage of nutrients such as vitamins, sugars and minerals to be used when needed
- Formation of proteins required for blood clotting
- Removal of toxic byproducts of cell metabolism and ingested drugs
- Removal of bacteria from the blood
What is Liver Disease?
The liver can be affected or become diseased due to several reasons. These include:
- Infections – Hepatitis B and hepatitis C
- Biliary tract obstruction – Primary sclerosing cholangitis, extra-hepatic biliary atresia
- Chemicals and toxins – Alcohol, drugs (statins, NSAIDs, aspirin, acetaminophen, antifungals and phenytoin)
- Liver tumors – Liver cell cancer, bile duct cancer
- Non-alcoholic fatty liver disease
- Acute liver damage – Drug overdose, viruses, mushroom poisoning, certain drug reactions
- Inherited and metabolic disorders – Wilson’s disease, alpha-1 antitrypsin deficiency, hemochromatosis, glycogen storage diseases, polycystic liver disease
- Congenital hepatic fibrosis
- Autoimmune – Autoimmune hepatitis, primary biliary cirrhosis
What is Liver Failure?
Liver failure or end stage liver disease occurs when a large portion of the liver is irreversibly damaged due to acute or chronic causes, as mentioned above, and is unable to function adequately and maintain several important functions.
Liver failure is divided into 2 types based on the time duration in which it occurs
- Acute – Acute liver failure develops rapidly, usually within weeks to months. In some cases, it is much more rapid. This type is usually caused by drug overdose (eg acetaminophen), reaction to certain drugs, viruses and mushroom poisoning. Acute liver failure may be fulminant (course of disease less than 8 weeks) or sub-fulminant (course ranges between 8 to 26 weeks)
- Chronic –
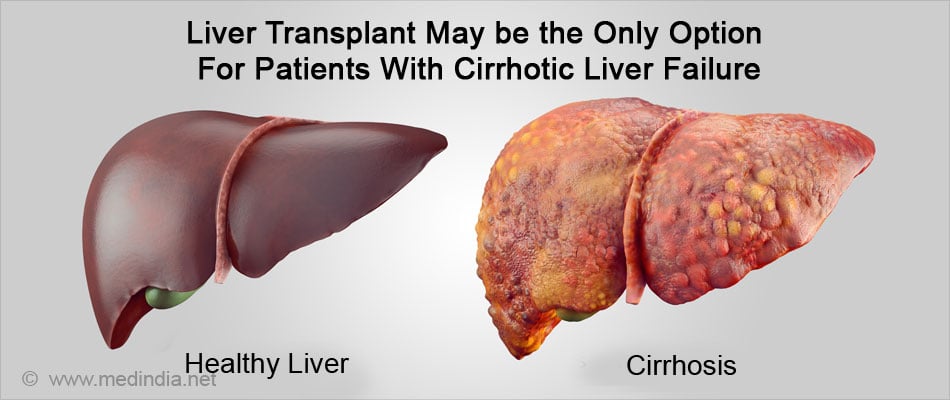
Chronic liver failure develops gradually over several years. In chronic liver failure, the liver becomes irreversibly damaged and scarred (cirrhosis) due to the underlying disease process. A large part of the liver is replaced with scar tissue which cannot perform the normal functions of the liver.
In the setting of acute or chronic liver failure, a liver transplant becomes necessary for survival.
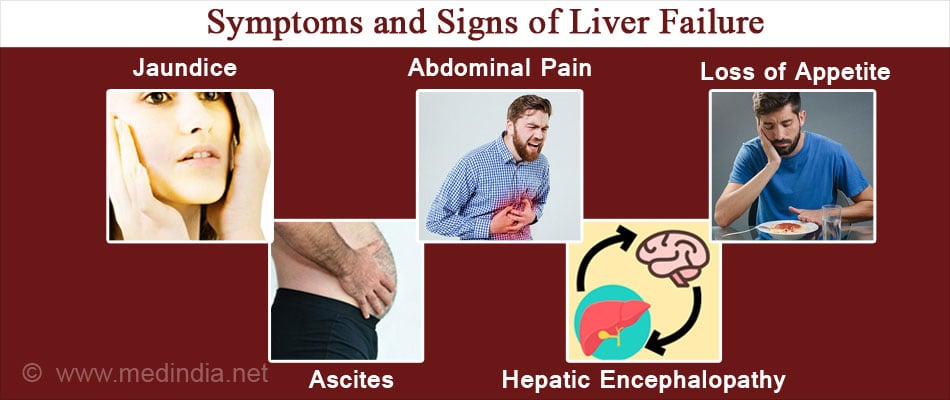
What are the Symptoms and Signs of Liver Failure?
Liver failure is recognized by the following symptoms and signs:
- Jaundice or yellowing of the skin and the white of the eyes
- Weakness and fatigue
- Confusion and clouding of consciousness (hepatic encephalopathy)
- Bleeding and bruising due to deficiency of clotting factors
- Vomiting blood (hematemesis) from engorged esophageal veins
- Passing black tarry stools
- Abdominal swelling due to fluid collection in the peritoneal cavity (ascites)
- Wasting of muscles
- Loss of appetite and weight
- Nausea and abdominal pain
What are the Common Types of Liver Disease Needing Transplant?
Some of the common types of liver disease that can progress to liver failure and ultimately need a liver transplant include the following:
Viral infection – The liver can be infected by hepatitis A, B and C viruses. Generally hepatitis A infection is a mild self-limiting illness. Hepatitis B and C infection can become chronic in some persons leading to inflammation and liver cell damage. Long standing hepatitis B or C infection leads to irreversible scarring or fibrosis (cirrhosis) of the liver with liver failure.
Hepatitis A and B infections are also known to cause acute fulminant hepatic failure (liver failure developing within 8 weeks in a previously normal and healthy liver).
Hepatitis A and B can be prevented by vaccination but currently there is no vaccine for hepatitis C. Treatment with antiviral drugs is available for hepatitis B and C. Unfortunately, these conditions are often diagnosed in the advanced stages when the drugs may not be effective.
Inherited metabolic disorders – These are genetic diseases caused by a mutated or defective genes. As a result, there is deficiency or lack of certain key enzymes that are necessary for the formation, transport or activity of certain substances such as iron, copper, glycogen and several others.
Metabolic diseases are thus characterized by accumulation of these substances or their precursors in the liver cells leading to liver cell damage and ultimately cirrhosis and liver failure.
Examples of some metabolic diseases include hemochromatosis (defective iron transport and overload), Wilson’s disease (defective copper transport and overload), glycogen storage diseases (defective formation of glycogen), and alpha-1 antitrypsin deficiency (defective transport of alpha-1AT).
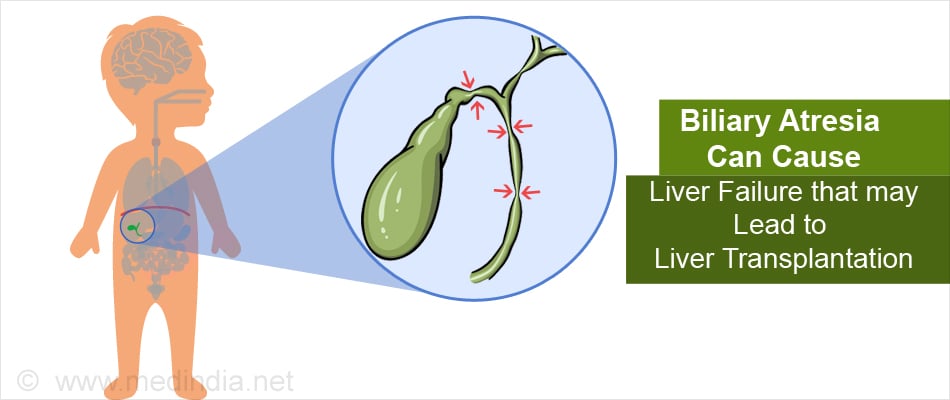
Biliary atresia – In biliary atresia, the biliary ducts outside the liver that connect the liver to the intestine are damaged or absent at birth. As a result, bile that is produced in the liver cannot reach the intestine. The resulting back flow of bile into the liver damages and scars the liver resulting in liver failure.
Infants who remain jaundiced even after 4 weeks of birth are investigated for biliary atresia and if diagnosed, surgery (Kasai procedure) is performed to re-establish bile flow before 8 weeks to achieve optimal results.
About 20 percent of infants do not get cured with the Kasai procedure and for these, liver transplant is the only cure for biliary atresia.
In fact, biliary atresia is the most common indication for liver transplant in children in the United States.
Acute liver damage – Some drugs especially acetaminophen overdose are associated with severe liver damage and death of large areas of liver cells. Other causes of massive liver cell death or necrosis include hepatitis B infection, mushroom poisoning and exposure to some chemicals such as carbon tetrachloride, an organic solvent used as a cleaning agent.
When acute liver necrosis and failure occurs, liver transplant is the only hope for survival.
Non-alcoholic fatty liver disease (NAFLD) – Fatty liver disease is typically associated with alcohol abuse. However, NAFLD occurs in persons who consume little or no alcohol. It is more common in the developed world and associated with obesity and type 2 diabetes, and is seen in the 4th to 5th decades.
Fat is deposited in the liver cells leading to inflammation and scarring terminating in liver failure.
Alcohol abuse – Alcohol abuse is one of the leading causes of liver disease. Normally alcohol is metabolized in the liver and when the liver has too much alcohol to handle, it can result in fat deposits in the liver cells (fatty liver), inflammation of the liver cells (alcoholic hepatitis) and in long standing abuse, scarring and irreversible liver damage (cirrhosis). When cirrhosis occurs with consequent liver failure, a liver transplant may be the only option for patient survival. It is however important that the person should abstain from drinking alcohol for a few months before the transplantation so that the condition does not recur after the transplantation. Transplantation is not advised in patients with acute alcohol hepatitis.
Alcoholic liver disease is also associated with development of liver cancer in some individuals, which is another indication for transplant.
Autoimmune liver diseases – In certain cases, the body’s immune system inappropriately attacks a person’s liver cells or the cells of the bile ducts. The ensuing inflammation and damage causes scarring and cirrhosis.
Examples of autoimmune liver diseases include autoimmune hepatitis, primary sclerosing cholangitis and primary biliary cirrhosis.
Primary sclerosing cholangitis and primary biliary cirrhosis are cholestatic (causing stasis of bile) liver diseases and liver transplant has been found to be highly effective if done at the appropriate time.
Autoimmune hepatitis with end stage liver disease is also an excellent indication for liver transplant.
Liver cancer – Hepatoblastoma is a rare form of liver cancer that occurs in children. It can be cured by surgical removal of the tumor and a liver transplant. Even if the primary tumor is inoperable because of size or location, a liver transplant may still cure the condition. Chemotherapy before and after transplant increases the chances of cure and prevents recurrences.
In adults, liver cancer is termed hepatocellular carcinoma (HCC). It can be caused by chronic hepatitis B or C infection, or any chronic liver disease with cirrhosis.
If the cancer remains localized to the liver, surgical removal of the tumor and the surrounding scarred cirrhotic liver and replacing with a healthy liver transplant is the only chance of survival. Though there have been mixed reports regarding the success of liver transplant in HCC patients, studies have shown that proper patient selection using stringent criteria (Milan criteria) significantly improved the chances of survival. Patients with cancers that have spread from other parts of the body to the liver do not qualify for liver transplantation.

Tips for a Healthy Liver
- Maintain a healthy weight since obesity can cause NAFLD
- Eat a balanced diet containing fruits, vegetables and fiber. Reduce the amount of red meat and avoid high calorie refined foods. Include good fats from vegetable oils, nuts seeds and fish
- Exercise regularly
- Avoid or limit alcohol intake. Do not take over-the-counter pain killers if you suffer from some form of liver disease
- Avoid unsafe injection practices. Use disposable needles. Use clean and fresh needles for body piercings and tattoos
- Practice safe sex – Hepatitis B and C can be transmitted through body fluids
- Seek medical care if exposed to blood. Wash the area with antiseptic immediately and go to the doctor
- Don’t share personal hygiene items such as razors, toothbrushes and nail clippers
- Get vaccinated against hepatitis A and B
- Foods that aid liver detoxification should be included in diet e.g. garlic, onions, leek, beets, avocado, spring onion, cabbage, kale, cauliflower, barley grass, alfalfa and spirulina