- Fatal familial insomnia - (https://rarediseases.info.nih.gov/gard/6429/fatal-familial-insomnia/resources/1)
- Schenkein J, Montagna P. Self Management of Fatal Familial Insomnia. Part 1: What Is FFI? Medscape General Medicine. 2006;8(3):65.
- Tabernero C et al. Fatal familial insomnia: clinical, neuropathological, and genetic description of a Spanish family. J Neurol Neurosurg Psychiatry. 2000;68:774-777.
- Introduction to fatal familial insomnia - (http://www.cureffi.org/2012/12/03/introduction-to-fatal-familial-insomnia/)
- Cortelli P et al. Gait disorders in fatal familial insomnia. Mov Disord. 2014;29(3):420-424.
- Montagna P et al. Familial and sporadic fatal insomnia. Lancet Neurol. 2003;2(3):167-176.
- Bechtel K, Geschwind MD. Ethics in Prion Disease. Progress in neurobiology. 2013;110:10.1016/j.pneurobio.2013.07.001. doi:10.1016/j.pneurobio.2013.07.001.
- Krasnianski A, Sanchez Juan P, Ponto C, et al. A proposal of new diagnostic pathway for fatal familial insomnia. Journal of Neurology, Neurosurgery, and Psychiatry. 2014;85(6):654-659. doi:10.1136/jnnp-2013-305978.
What is Fatal Familial Insomnia?
Can you imagine lack of sleep or insomnia being a fatal problem? Well, in certain cases, insomnia is an inherited condition that occurs due to brain abnormalities.
The basic correlation between sleep and brain disorders was observed as early as 1939. However, it was Elio Lugaresi’s group that first reported the condition of fatal familial insomnia in a patient in 1986. Fatal familial insomnia (FFI) is an inherited disease that belongs to a group of diseases called prion diseases. Prion diseases are caused by the accumulation of proteins called prions of altered conformation in the brain cells, thereby damaging the cells.

Fatal familial insomnia is a rare brain disease characterized by insomnia or sleeplessness and hallucinations, among other symptoms. The symptoms usually appear later in life, between 20 and 61 years of age but more commonly around 50 years of age. The condition is fatal between 7 and 36 months after the appearance of symptoms. Fatal familial insomnia shows no gender discrimination with both sexes being equally affected. Though considered a fatal disorder, it must be noted that in the paper by Pasquale Montagna and colleagues, mentions that a few unreported cases of FFI carriers who are still leading a healthy life at the age of 74.
What are the Causes of Fatal Familial Insomnia?
Fatal familial insomnia is a genetic condition caused by a mutation in the prion gene (PRNP) is located on chromosome 20. This results in the formation of prion protein (PrP) with altered conformation. The defective protein forms clumps which destroy the neurons or the nerve cells. This results in the signs and symptoms observed in fatal familial insomnia.
Fatal familial insomnia is inherited in an autosomal dominant pattern. Thus, only one defective gene on a single chromosome is enough to cause the condition.
What are the Symptoms and Signs of Fatal Familial Insomnia?
Fatal Familial Insomnia affects several parts of the brain, but mainly the thalamus. The thalamus is a very important part of the brain that is involved in the sleep-wakefulness cycle, consciousness and interpretation of sensory stimuli. Fatal familial insomnia is characterized by the following symptoms:
- Hallucinations
- Insomnia or sleeplessness that is progressive
- Loss of short-term memory
- Dreaminess
- Inability to move after waking up
- Attention deficit
- Problems with walking and other movements
- Hormonal issues
- Loss of weight
- Dementia or forgetfulness
- Hyperthermia or hypothermia (changes in temperature)
- Hypertension
- Perspiration
- Salivation
- Seizures
Fatal Familial Insomnia Stages
Patients show insomnia, perspiration, salivation, fever, hypertension in the initial stages of the condition. Hallucinations, dreaminess, abnormalities in gait and movement set in as the condition progresses. Individuals may pass away either in a conscious state or may lapse into a vegetative state before passing away. Insomnia may not be the predominant symptom in those whose disease is a slow-progressing disease. If it is a rapidly progressing condition, then insomnia is a predominant feature.
How do you Diagnose Fatal Familial Insomnia?
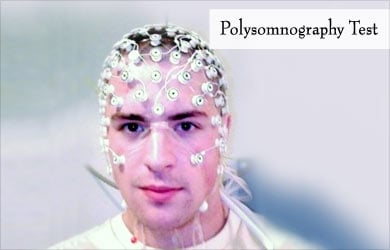
The best diagnostic method that has been approved so far for the diagnosis of FFI is polysomnography or a sleep study. Positron emission tomography is also accurate in detecting FFI by detecting the degradation of the thalamus in the brain. Genetic analysis of the PRNP gene is another method of diagnosing the condition. However, sometimes, mutations may not be detected despite the condition being present.
Researchers have suggested the following steps in the diagnosis of fatal familial insomnia:
- Observe for sleep disturbances or if not obvious, perform a polysomnography test.
- Observe for a minimum of 2 symptoms resembling Creutzfeldt-Jacob disease, another prion disease. These symptoms include defects in cognition, psychiatric disorders like anxiety, hallucinations, and depression, motor movement abnormalities, and visual defects.
- In addition, at least one of the symptoms specific to FFI like husky voice, weight loss is greater than 10 kg over a period of 6 months, hyperthermia, excessive sweating, and abnormally fast heartbeat should be present.
Individuals who satisfy the above three steps of diagnosis could be diagnosed as suffering from fatal familial insomnia.
How do you Treat Fatal Familial Insomnia?
Currently, there is no cure for fatal familial insomnia or for that matter, any prion disease. Once detected, the role of the caregiver is to manage the symptoms and reduce the discomfort due to the symptoms.
Certain drug trials for human FFI have been carried out. The drugs used are doxycycline, quinacrine, and intracerebral pentosan polysulfate (PPS). However, there has been no clear positive effect of these drugs on FFI.

Health Tips
In the article by Kendra Bechtel of University of California, San Francisco, the ethical issues related to early diagnosis of prion diseases are dealt with. It is suggested that early diagnosis can help prepare the patient with the choices to make regarding the family, professional life, and treatment. Early diagnosis can also avoid strain on the resources of the hospital with fewer diagnostic procedures, and preventive treatment can be utilized. The family is also prepared for the consequences. However, the downside of early diagnosis may result in anxiety and depression for the patient with FFI.







