- Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990-2017: a population-based observational study - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7402189/)
- The role of hepatic fat accumulation in pathogenesis of non-alcoholic fatty liver disease (NAFLD) - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2873482/)
- Non-alcoholic fatty liver disease and associated dietary and lifestyle risk factors - (https://pubmed.ncbi.nlm.nih.gov/29571977/)
- Fatty Liver - (https://www.ncbi.nlm.nih.gov/books/NBK441992/)
- Nonalcoholic Fatty Liver - (https://www.ncbi.nlm.nih.gov/books/NBK541033/)
- Current status of imaging in nonalcoholic fatty liver disease - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6120999/)
- LIDO Study Group; CYTOL study group. Diagnostic value of biochemical markers (FibroTest-FibroSURE) for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1386692/)
- Diagnosis and Evaluation of Nonalcoholic Fatty Liver Disease/Nonalcoholic Steatohepatitis, Including Noninvasive Biomarkers and Transient Elastography - (https://pubmed.ncbi.nlm.nih.gov/29128062/)
- Saroglitazar for Nonalcoholic Fatty Liver Disease: A Single Centre Experience in 91 Patients - (https://pubmed.ncbi.nlm.nih.gov/35535066/)
- Liraglutide's use in treatment of non-alcoholic fatty liver: an evaluation of the non-alcoholic steatohepatitis study - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5218908/)
- Advances and Emerging Therapies in the Treatment of Non-alcoholic Steatohepatitis - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9835815/)
- Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of the Novel Non-Bile Acid FXR Agonist Tropifexor (LJN452) in Healthy Volunteers - (https://pubmed.ncbi.nlm.nih.gov/31823525/)
- Vitamin D: a new player in non-alcoholic fatty liver disease? - (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4323447/)
About
Non alcoholic fatty liver disease (NAFLD) is the leading cause of liver dysfunction worldwide and is a rapidly growing health problem in regions such as the Middle East, Far East, Africa, the Caribbean, and Latin America. some of the developing countries like India(1✔ ✔Trusted Source
Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990-2017: a population-based observational study
Go to source).
NAFLD ranges from benign accumulation of fat droplets within liver cells (“steatosis”) to an inflammatory state causing fibrosis of the liver (Non Alcoholic Steatohepatitis, or NASH) to end stage liver cirrhosis. In NAFLD the excess fat accumulation is in the form of excessive triglycerides in the liver and they occupy more than 5% of liver cells called hepatocytes. This means that the fat forms 5% of the weight of the liver. Normally there is hardly any fat present in the liver(2✔ ✔Trusted Source
The role of hepatic fat accumulation in pathogenesis of non-alcoholic fatty liver disease (NAFLD)
Go to source).
In NASH there is injury to liver cells due to the fat and this causes the inflammation and fibrosis as stated earlier. Aside from the risk of liver failure, there is also an increased risk of developing liver cancer (hepatocellular carcinoma or HCC) with NASH.
Within the next five years, NASH cirrhosis will surpass Hepatitis C Virus cirrhosis as the leading indication for liver transplant in Western countries.
In 2008 there were at least 1.46 billion adults who were overweight or obese and another 170 million children who were obese and this number seems to be on the rise. Currently there seems to be a worldwide epidemic of
Causes of Non alcoholic fatty liver disease (NAFLD)
The two main causes of NAFLD are poor diet and sedentary lifestyle(3✔ ✔Trusted Source
Non-alcoholic fatty liver disease and associated dietary and lifestyle risk factors
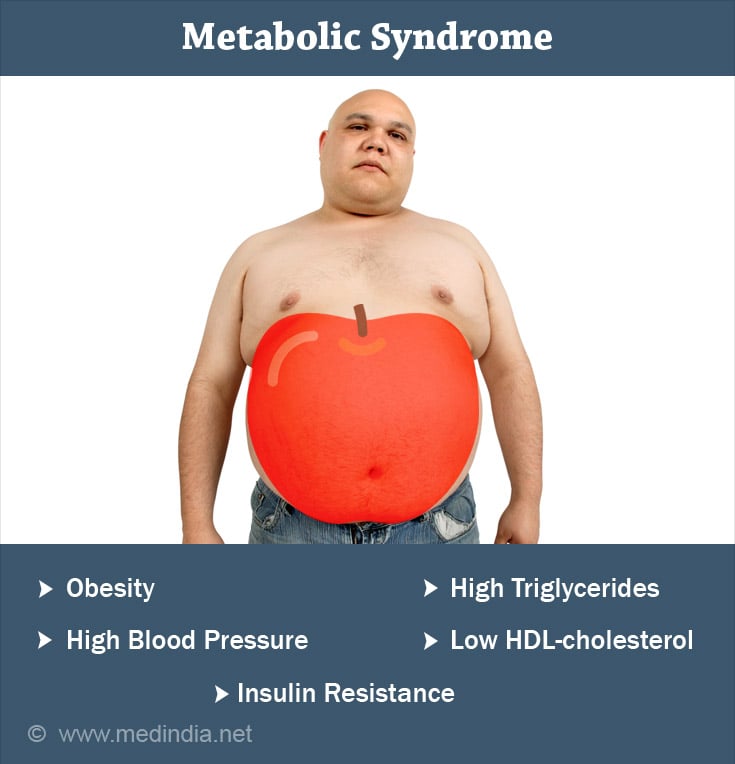
Go to source). NAFLD goes hand in hand with obesity and diabetes and is therefore a component of the Metabolic Syndrome, which consists of 3 or more of the following: obesity, hypertension, elevated fasting blood glucose, hypertriglyceridemia or low high-density lipoprotein levels.
Indians and NAFLD A recent study by Kalra and colleagues reported that among Indians with Type II Diabetes Mellitus, 56.5% also have NAFLD.
There are also genetic factors predisposing to NAFLD. For instance, simple steatosis is highly prevalent in the Indian population, even in people who are not overweight, are not diabetic, and don’t drink alcohol. So the unfortunate combination of a genetic predisposition, lack of exercise, and a diet rich in ghee, sugar, and oils, all conspire to make NAFLD a major health problem in India.
Other causes of fat accumulation within liver cells are excessive alcohol intake, many drugs (particularly chemotherapeutic agents and certain antiviral medications), pregnancy, and chemicals such as carbon tetrachloride.
The term NAFLD is used to distinguish fatty liver disease caused by the Metabolic Syndrome from these other causes. A fatty liver is reversible in its early stages if the offending causes are curtailed or ceased, but continued injury can ultimately cause progression to NASH, cirrhosis, and liver cancer(4✔ ✔Trusted Source
Fatty Liver
Go to source).
Symptoms of NAFLD & NASH
NAFLD and NASH are asymptomatic in their early stages. As the disease progresses, fatigue, malaise, and right upper quadrant pain are the earliest symptoms. As NASH progresses to liver cirrhosis, classic symptoms of liver insufficiency can occur: swelling of the legs and abdomen, confusion, muscle wasting, etc.
Symptoms associated with the Metabolic Syndrome (obesity, diabetes, hypertension, and hyperlipidemia) such as frequent urination, excessive thirst, and headache, should alert treating physicians to the possibility of underlying, asymptomatic fatty liver disease(5✔ ✔Trusted Source
Nonalcoholic Fatty Liver
Go to source).
Diagnosis of NAFLD & NASH
Liver Function Tests: Simple liver function tests, such as AST, ALT, INR, and GGT, can be slightly elevated in early NASH, but they are nonspecific in determining the severity of disease(5✔ ✔Trusted Source
Nonalcoholic Fatty Liver
Go to source).
Ultrasound: New multiparametric ultrasound techniques are emerging that can quantify fibrosis, steatosis, and possibly inflammation. This would be a perfect non-invasive way to diagnose and monitor these patients and would be useful for even for non-alcoholic steatohepatitis (NASH)(5✔ ✔Trusted Source
Nonalcoholic Fatty Liver
Go to source).
CT Scan & MRI: Imaging tests such as ultrasound, CAT scan, and MRI can diagnose later stage NAFLD, but they are insensitive in detecting early disease. Combining these imaging techniques with other modalities such as elastography can improve sensitivity and there is active research promising that these procedures will soon be available(6✔ ✔Trusted Source
Current status of imaging in nonalcoholic fatty liver disease
Go to source).

Fibro Scan: Proprietary tests such as FibroTest (trademark) have been shown to be more sensitive and specific, but they are not routinely used due to expense(7✔ ✔Trusted Source
LIDO Study Group; CYTOL study group. Diagnostic value of biochemical markers (FibroTest-FibroSURE) for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease
Go to source).
Liver Biopsy: The gold standard for diagnosing NAFLD is liver biopsy, but this procedure is invasive, painful, and carries risks of complications such as internal bleeding. So, doctors are reluctant to order a liver biopsy unless absolutely necessary(8✔ ✔Trusted Source
Diagnosis and Evaluation of Nonalcoholic Fatty Liver Disease/Nonalcoholic Steatohepatitis, Including Noninvasive Biomarkers and Transient Elastography
Go to source).
Treatment for NAFLD
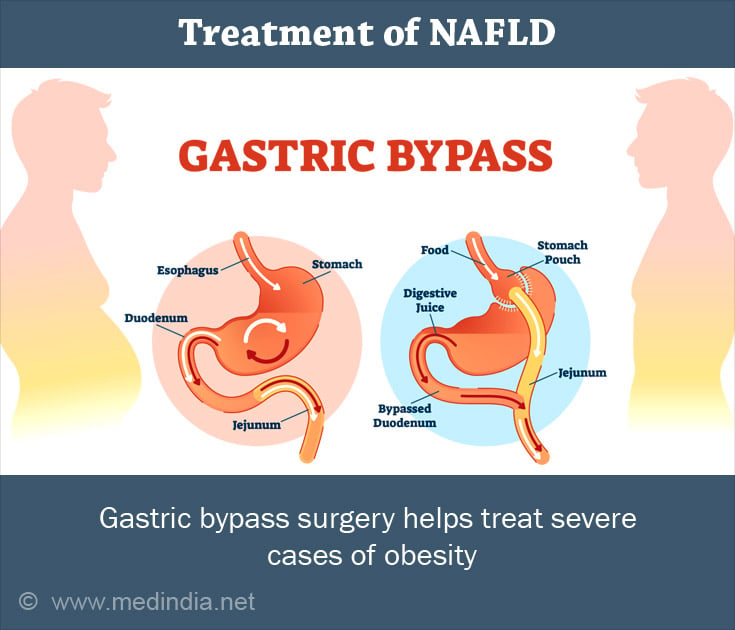
The primary treatment for NAFLD is lifestyle modification. Eating a balanced diet, eating less, and increasing one's physical activity all promote weight loss and improve or prevent diabetes and fatty liver. In severe cases of obesity, surgical or minimally invasive weight loss procedures may be considered, such as gastric bypass surgery (open, laparoscopic, or robotic) or endoscopy(5✔ ✔Trusted Source
Nonalcoholic Fatty Liver
Go to source).
Basic research points to potential medical therapies the treat NAFLD, for example, the diabetes drug Metformin and inhibitors of the endocannabinoid pathway, but no human clinical trials exist as of yet that show efficacy.
There is some evidence that treating diseases concomitant with NAFLD, such as diabetes and hyperlipidemia, can improve NAFLD and possibly prevent progression of liver disease.
Recent Advances with Treatment of NAFLD
Saroglitazar: It is well tolerated drug and effective with no new onset decompensation in compensated cirrhosis patients with approximately 23% reduction in 'Liver Stiffnes'at one year compared with baseline(9✔ ✔Trusted Source
Saroglitazar for Nonalcoholic Fatty Liver Disease: A Single Centre Experience in 91 Patients
Go to source).
Liraglutide: This drug has the potential to cure for Type 2 diabetes with NAFLD(10✔ ✔Trusted Source
Liraglutide's use in treatment of non-alcoholic fatty liver: an evaluation of the non-alcoholic steatohepatitis study
Go to source).
Pegozafermin: It is another drug in early trials that shows it is well tolerated and can reduce liver fat, improve liver function, and increase circulating lipids(11✔ ✔Trusted Source
Advances and Emerging Therapies in the Treatment of Non-alcoholic Steatohepatitis
Go to source).
Tropifexor: Treatment helped improve liver function However it can cause pruritus(12✔ ✔Trusted Source
Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics of the Novel Non-Bile Acid FXR Agonist Tropifexor (LJN452) in Healthy Volunteers
Go to source).
Vitamin D: It may play a role in NAFLD prevention among Europeans(13✔ ✔Trusted Source
Vitamin D: a new player in non-alcoholic fatty liver disease?
Go to source).












