- Ramana, K V, et al. "Invasive Fungal Infections: A Comprehensive Review." American Journal of Infectious Diseases and Microbiology 1.4 (2013): 64-69.
- Cryptococcus neoformans - (https://en.wikipedia.org/wiki/Cryptococcus_neoformans)
- Oral Antifungal Drugs - (https://www.drugoffice.gov.hk/eps/do/en/consumer/news_informations/dm_18.html#e)
Overview and Facts about Fungal Infections
Fungi are a highly adaptable group of organisms.
- Fungi are classified into a separate kingdom of their own (neither plants nor animals).
- They can live freely in the environment, or be a part of the normal flora in animals and humans.
- They can cause superficial infections of the skin with red itchy lesions, as well as deep and invasive systemic infections, especially in persons with reduced immunity.
- Usually, fungal infections are mild and become serious or threatening only in those with a weakened immune system.
- Typically, fungal infections progress slowly and do not pass from one person to another, except in the case of certain superficial skin infections.
- Fungal infections are becoming a source of major health concern nowadays due to the use of potent immunosuppression for certain diseases and in transplant recipients, with the use of invasive devices in the hospital to monitor critically ill patients and with the increase in the incidence of diseases such as AIDS that cause immunosuppression.
- Fungal spores (structures formed during fungal reproduction and adapted for survival in unfavorable environmental conditions) exist in the air and in the soil and can cause infection in susceptible individuals.
- Fungal spores can thus be inhaled or come in contact with human skin. As a result, fungal infections usually begin in the skin or the lungs.
- Fungi can exist in two morphological forms namely, single rounded cells, also known as yeast forms, and the mold forms where many cells join together to form long threadlike structures called hyphae.
- Superficial skin and mucous membrane fungal infections are treated with topical application of powders or gels. Serious infections are treated with anti-fungal drugs given by mouth or by injections. Antibiotics are not effective in fungal infections and should not be used.
What are the Types of Fungal Infections?
Fungal infections may be described as primary or opportunistic. They can be localized i.e. limited to one region e.g. localized in a part of the skin,mouth or vagina, or be invasive i.e spread to multiple sites. Skin and nail bed infections are also described as ‘superficial’ while invasive and systemic infections are referred to as ‘deep’ infections.
- Primary infections affect persons with a normal immune system.
- Opportunistic infections, as the name suggests, occur in persons with a weakened immune system (the fungi availing the opportunity) and persons with normal immunity are rarely affected.
- Fungal infection remains localized in persons with good immunity but can become invasive and threatening in persons with a poor and ineffective immune system.
- Localized infections include involvement of sinuses. This typically occurs with Aspergillus spp which can form a fungal ball within the sinuses causing features of chronic sinus infection such as fever with cough and headache.
1. Superficial Fungal Infections
Fungi that cause skin infections are referred to as dermatophytes. They live on dead body tissues such as hair and nails. They cause disease on skin that is weakened or injured or constantly moist. Candida or yeast is another fungus that can also cause superficial infections.
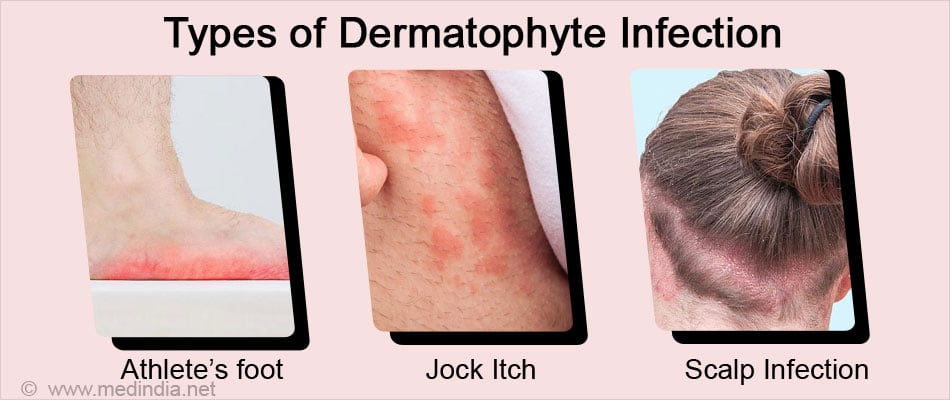
Dermatophyte infection
Infection caused by dermatophytes is referred to as tinea or ringworm infection. Ringworm infection can spread by contact with skin or clothing of infected persons. Depending on the location, the various types include:
- Athlete's foot (tinea pedis)
- Barber's itch occurring in the beard (tinea barbae)
- Jock itch (tinea cruris) occurring in the groin
- Scalp infection (tinea capitis)
- Hand infection (tinea manuum)
- Infection in other parts of the body (tinea corporis)
- Nail bed infection (tinea unguium)
Cutaneous yeast or Candida infection
Cutaneous yeast infection or cutaneous candidiasis can involve any part of the skin but occurs most commonly in warm, moist and creased areas such as armpits, groin and underneath body folds. It often occurs in obese persons, persons suffering from diabetes and those on longterm antibiotics.
Other yeast infections include oral thrush occurring in the mouth, vaginal yeast infections (also referred to as moniliasis) in women and fungal diaper or nappy rash in babies.
2. Deep or Systemic Fungal Infections
Systemic fungal infections include the following -
- Invasive aspergillosis
- Systemic candidiasis
- Mucormycosis
- Cryptococcosis
- Histoplasmosis
- Blastomycosis
- Coccidioidomycosis
- Paracoccidioidomycosis
How Does Fungal Infection Spread?
Fungal infections, as mentioned earlier, are acquired by inhalation of spores or contact of spores on the skin.
Superficial skin infections are spread from one part of the body to another by scratching the lesions and touching other parts of the body, or through contact with the skin or clothing of infected persons.
Deep seated or systemic infections enter the body via inhalation of spores. In invasive disease, the organisms are carried to different parts of the body through the bloodstream.
What are the Risk Factors of Developing Fungal Infections?
A person’s immunity may be suppressed due to drugs that are administered for the treatment of other conditions or a disease occurring in the person that naturally suppresses his or her immunity. Thus, the risk factors of developing a fungal infection include the following:
Drugs that suppress immunity
- Corticosteroids
- Drugs used to prevent transplant rejection – e.g. methotrexate, cyclosporine, azathioprine
- Drugs used to treat cancer
- Drugs used to treat rheumatoid arthritis and related conditions – e.g. tumor necrosis factor inhibitors
Diseases that suppress immunity
- Cancers like leukemia, Hodgkin’s and non-Hodgkin’s lymphomas
- Diabetes
- Acquired Immunodeficiency syndrome (AIDS)
Others:
- Preterm infants
- Persons undergoing intensive care treatment
- Longterm broad spectrum antibiotic therapy
- Elderly and weak individuals
- Insertion of indwelling catheters or other devices
- Inherited causes of immune deficiency

What are the Symptoms and Signs of Fungal Infections?
Here are some of the Clinical features of various types of fungal infections.
Clinical features of tinea or ringworm infections include the following:
- Itchy, red and scaly ring-shaped patches
- Loss of hair in affected area
- Peeling and cracking of skin
- Cracking or breaking and thickening of nails with discoloration
Symptoms and signs of yeast infection affecting the skin and mucus membranes include the following:
- Skin rash that is itchy, especially in skin folds
- Tiny bumps on the skin
- Skin lesions that ooze clear fluid
- Discolored nails that break from the nail bed (nail bed infection)
- White patches on the tongue or inner aspect of cheek (oral thrush)
- White or yellow thick vaginal discharge (vaginal candidiasis)
- Redness and itching on the skin of the external genitalia

Systemic fungal infections may be primary or opportunistic
Primary systemic fungal infections
These infections occur in persons with normal immunity and include Histoplasmosis, blastomycosis, coccidioidomycosis and paracoccidioidomycosis infections that are acquired by inhalation of spores in the air. The main symptoms are related to the respiratory tract and may include:
- Fever with cough
- Difficulty in breathing
- Flu-like illness
- Chest pain
In some persons when large amounts of spores are inhaled or in individuals with weakened immunity, the infection may spread to other parts of the body resulting in a serious infection like:
- Progressive disseminated histoplasmosis, characterized by enlarged liver, spleen and lymph nodes, brain involvement and ulcers in mouth and intestines
- Progressive blastomycosis, which may cause multiple skin lesions and may involve the prostate, bone and even the brain
- Progressive coccidioidomycosis, – characterized by skin lesions, bone and joint involvement, and even brain disease
Opportunistic systemic infections
These typically occur in immunosuppressed persons. Opportunistic fungi generally do not cause infection in normal individuals. They include Mucor, Cryptococcus, Aspergillus and Candida. Some of the systemic infections caused by these fungi include the following:
- Invasive bronchopulmonary aspergillosis – The infection starts in the lungs and can spread via the bloodstream to involve organs like the brain, liver, heart and kidneys.
- Rhinocerebral mucormycosis – The infection occurs in persons with poorly controlled diabetes. It can affect the eye causing swelling of eye and protrusion of the eye from the socket (proptosis). There may be loss of vision. Facial and nasal bones can be destroyed by invasive disease and appear black. The brain may be involved with development of paralysis, seizures and coma.
- Systemic candidiasis: Systemic Candida infection can involve multiple organs such as the brain, heart, lungs, kidneys, eyes and spleen. It is commonly seen in hospitalized and ill patients with indwelling catheters or other devices. It can be fatal unless promptly treated.
- Cryptococcal meningitis – Infection is acquired via inhalation of spores and rapidly spreads from the lung to the brain. It is often seen in AIDS patients.
How do You Diagnose Fungal Infections?
Superficial Infections
Clinical examination:
Fungal infections of the skin, hair, and nails are often diagnosed by the characteristic symptoms and appearance of the lesions.
KOH preparation
A KOH (potassium hydroxide) preparation is a simple laboratory test to confirm the diagnosis. A sample from the lesion is treated with KOH and examined under the microscope to detect fungal elements.
The use of stains such as Gram stain Giemsa and India ink increase the chances of detection.
Wood’s lamp examination
Direct examination of the skin lesion with a Wood's ultraviolet lamp is another simple and convenient method to detect the presence of a fungus.
Culture and sensitivity
Culture of the organism from the lesion on special fungal media can be used for a more definitive diagnosis.
Systemic Fungal Infections
Blood tests – Serological tests to detect fungal antigens in the tissue/lesion samples or antibodies in the serum may be done.
Culture
The organism can be cultured from samples of sputum, urine, blood or other infective lesions for a more definite diagnosis.
Molecular methods
Tests based on amplification of DNA e.g. polymerase chain reaction (PCR) may be useful when the diagnosis is difficult.
Tissue biopsy
Histological examination of the tissue sample by employing routine and special stains gives a definitive diagnosis.
How do You Treat Fungal Infections?
Superficial Infections
Mild superficial fungal infections usually respond to topical anti-fungal creams or sprays such as tolnaftate, clotrimazole, itraconazole, fluconazole, miconazole nitrate, econazole, ketoconazole, ciclopirox, naftifine, terbinafine or Whitfield's tincture containing salicylic acid and benzoic acid.
Infections that do not respond to local applications may also need the addition of an oral anti-fungal drug such as itraconazole, ketoconazole or griseofulvin.
Systemic Infections
Systemic infections may be treated with one of the azoles e.g. fluconazole or itraconazole which are the least toxic. Other agents include flucytosine used alone or with another agent.
For life-threatening infections, amphotericin B may be used, although it is a highly toxic drug and can cause kidney damage.
Some extensive fungal infections may need surgery to remove dead and damaged tissue.
How do You Prevent Fungal Infections?
The following measures may help reduce or prevent superficial fungal infections:
- Maintain good personal hygiene
- Keep the skin clean and dry
- Avoid scratching lesions and immediately touching other parts of the body
- Avoid sharing or borrowing of bed linen and other clothes
- Clothes and contact surfaces of infected person should be washed in hot water and disinfected
- Avoid wearing heavy clothes in warm weather
Systemic infections can be controlled by the following:
- Keep blood sugar levels in check if you a diabetic
- Avoid the unnecessary use of antibiotics
- Persons on immunosuppressive agents should undergo regular check-ups for fungal infection
- Environmental screening and effective disinfection protocols should be followed in hospitals







