- Tham, Yih-Chung, et al. "Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis." Ophthalmology 121.11 (2014): 2081-2090.
- Kapetanakis, Venediktos V., et al. "Global variations and time trends in the prevalence of primary open angle glaucoma (POAG): a systematic review and meta-analysis." British Journal of Ophthalmology (2015): bjophthalmol-2015.
- Becker – Shaffer’s Diagnosis and Therapy of the Glaucomas
- Jasien JV, Jonas JB, de Moraes CG, Ritch R. Intraocular Pressure Rise in Subjects with and without Glaucoma during Four Common Yoga Positions. Lin H, ed. PLoS ONE. 2015;10(12):e0144505. doi:10.1371/journal.pone.0144505.
- Sun, Xiaoshen, et al. "Focus: Addiction: Marijuana for Glaucoma: A Recipe for Disaster or Treatment?." The Yale journal of biology and medicine 88.3 (2015): 265.
- Yoga Positions and Glaucoma - (https://www.glaucoma.org.au/articles/yoga-positions-and-glaucoma-body/ )
- Glaucoma and Lifestyle - (http://www.glaucoma.org.nz/about-glaucoma/life-with-glaucoma/glaucoma-and-lifestyle.asp)
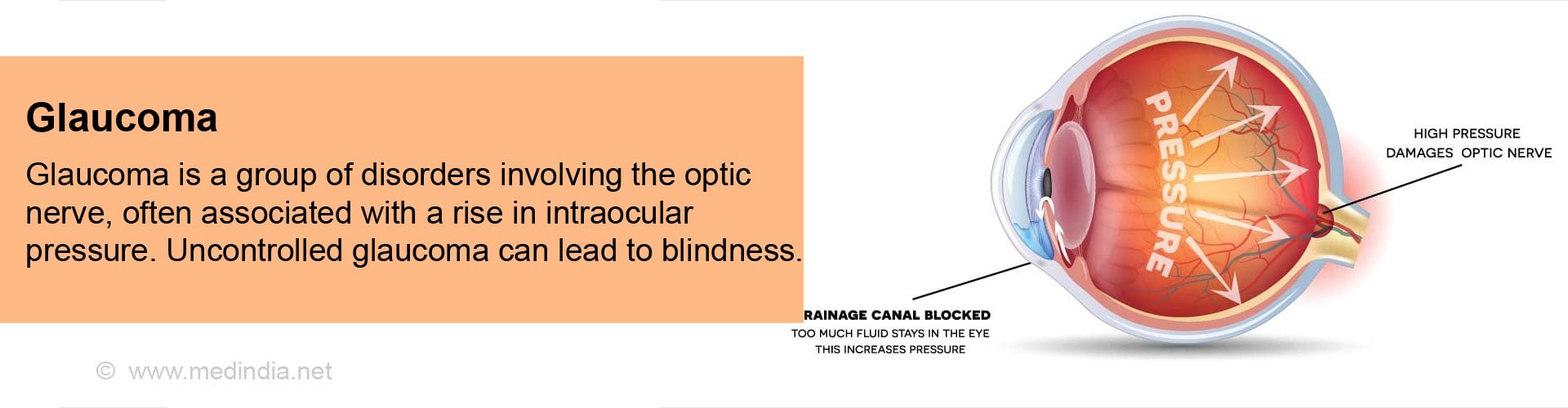
What is Glaucoma?
Glaucoma, refers to a group of disorders that have in common a specific pattern of optic nerve involvement with specific visual field changes, and which are most commonly due to a rise in intraocular pressure.
Earlier glaucoma was defined as a rise in intraocular pressure, which then resulted in optic nerve damage. Recent studies have shown that the specific type of optic nerve damage that occurs only in glaucoma may occur at normal eye pressures as well. These patients have an inherent weakness in the optic nerve that makes it susceptible to damage even at normal intraocular pressures. Hence this change in the definition. However raised intraocular pressure is still the most important modifiable risk factor for glaucoma.
In glaucoma, the optic nerve head (beginning of the optic nerve, and visible while examining the retina as the optic disc) undergoes certain anatomical changes (referred to as cupping) that does not occur in any other disease. These changes are permanent and result in visual impairment. Consequent to the optic disc changes, changes start occurring in the visual field (the entire area which can be seen by the eye without shifting the gaze), such as scotomas or blind spots. These are also permanent, and progress if the glaucoma is not under control. There is a gradual contraction of the visual field which in later stages leads to tunnel vision (only the central portion of the visual field remains). Further progression leads to total blindness.
These optic nerve and visual field changes occur when there is a sustained rise in intraocular pressure. A sudden rise which is controlled very soon does not give rise to these changes, unless repeated episodes occur.
| Glaucoma |
|
Facts & Statistics about Glaucoma
Glaucoma is the second leading cause of blindness in the world after cataracts, and the leading cause of irreversible visual impairment around the world.
Primary open angle glaucoma is more common and accounts for almost three quarters of glaucoma cases.
In the West, open angle glaucoma is more prevalent in blacks. However, since angle closure glaucoma is slightly more common among Asians who constitute 60% of the world population; this type of glaucoma is responsible for the maximum number of blind people due to glaucoma in the world.
Understanding Glaucoma - Aqueous Humor Dynamics
The aqueous humor is the fluid present in the anterior segment of the eye, the part between the cornea on the outside and the iris and lens on the inside. It helps to maintain the intraocular pressure. The production of aqueous humor and its drainage occur at an equal rate in the eye. Any small change in either function can have a large change in the intraocular pressure.
The aqueous humor is produced in the ciliary body, and enters the anterior chamber from behind the iris through the pupil. It drains via a sieve-like tissue called the trabecular meshwork into a tube-like structure called the Schlemm’s canal. From here, it passes via the collector channels in the sclera into the episcleral veins, which are small veins in the sclera, the tough white part of the eye. The trabecular meshwork is situated in the angle between the periphery of the iris and the cornea. Thus, blockage of the aqueous humor drainage can be due to either of the following:
- Closing of this angle (angle closure glaucoma) as the aqueous no longer has access to the trabecular meshwork.
- The angle may be open but the trabecular spaces may be narrowed, thus providing increased resistance to the drainage of aqueous (open angle glaucoma).
- Occasionally both mechanisms may operate (combined mechanism glaucoma).
What are the Types and Causes of Glaucoma?
Almost all glaucomas are due to deficient drainage of aqueous humor from the eye. Glaucoma can be broadly divided into childhood and adult glaucomas.
- Childhood glaucoma can be:
- Primary congenital (present since birth). This is the most common of the pediatric glaucomas, and believed to be genetic in origin
- Infantile (present within a few years of birth)
- Juvenile glaucoma (which presents after 3 years of age or in early adulthood)
Congenital and infantile glaucomas are usually due to developmental anomalies in the angle of the anterior chamber of the eye leading to deficient drainage of the aqueous humor.
- Adult glaucomas are primary open angle, primary angle closure or secondary glaucomas.
Primary open angle glaucoma (POAG) is the more common type, and is characterized by slowly progressive optic nerve and visual field changes, usually with a raised intraocular pressure. It occurs due to a deficient drainage mechanism at the level of the trabecular meshwork.
Important risk factors in POAG
- Myopia or short sightedness
- Black race
- Family history of glaucoma
- Advanced age
- Decreased central corneal thickness
- Diabetes mellitus
Primary angle closure glaucoma (PACG) is characterized by closure of the angle of the anterior chamber by the iris (in an eye that has an anatomically narrow angle) thus preventing access of aqueous to the trabecular meshwork, and drainage of the aqueous humor. Here, the intraocular pressure rises are more sudden and more severe than that of POAG.
Important risk factors in PACG
- Middle age females
- Hypermetropia or long sightedness
- Small eyes
- Eskimos & South east Asians
- Family history of angle closure glaucoma
- Advanced age
Secondary glaucomas can be either open angle or closed angle and are usually associated with some other disease in the eye. Some of the causes of secondary glaucoma are –
| Type of Glaucoma | Disease Entity | Pathology | Important Clinical Features |
| Secondary Open Glaucomas | Pseudoexfoliation syndrome | Block in trabecular meshwork (TM) by protein containing fibrilliar material. | Gradual onset; occurs in older individuals |
| Pigmentary glaucoma | Block in TM by iris pigment. | Gradual onset. More common in young male myopes. | |
| Phacolytic glaucoma | Block of TM by large cells (macrophages) containing ingested lens material. | Sudden rise of intraocular pressure. Presents with redness and pain in eye. | |
| Lens particle glaucoma | Block of TM by lens cortex particles | Slow onset. Usually follows cataract surgery or eye injury. | |
| Phacoantigenic glaucoma | Antibodies formed to the patient’s own lens proteins. | Slow onset. Usually follows cataract surgery or eye injury and associated with ocular inflammation. | |
| Inflammation of iris & ciliary body | TM dysfunction, and block by inflammatory cells. | Associated with inflammation of the eye and so eye would be red and painful in most cases. | |
| Intraocular tumors | Block of TM by tumor cells and debris. | Slow onset. | |
| Eye injury | Direct injury to TM or block by inflammatory cell and blood. | Features suggestive of trauma are present. | |
| Steroid induced glaucoma | Deposition of extracellular matrix material in outflow channels. | Clinical features similar to POAG. | |
| Secondary Angle Closure Glaucoma | Phacomorphic glaucoma | Swollen lens blocks pupil; accumulated aqueous behind iris pushes iris forward to block angle of anterior chamber. | Sudden rise of IOP (intraocular pressure). Eye becomes red and painful). |
| Lens displacement | Pupillary block. | Sudden rise of IOP (intraocular pressure) . Eye becomes red and painful) | |
| Neovascular glaucoma | Contraction of fibrovascular membrane in angle of anterior chamber leads to angle closure. | More common in diabetes and blockage of the central vein of the retina. Gradual onset. Painful in advanced stages | |
| Intraocular tumors | Pushing forward of lens and iris. | Gradual onset. | |
| Inflammation of iris and ciliary body | Inflammatory sequelae lead to pupillary block. | Gradual onset in an inflamed eye. | |
| Malignant glaucoma | Aqueous gets misdirected into the vitreous and pushes iris forward to block the angle. | Often follows ocular surgery. Rapid onset with very high intraocular pressure. | |
| Drug induced | Fluid accumulation which pushes the iris forward to block the angle. | Most commonly seen with topiramate and sulphonamides. Presents as a bilateral acute myopia initially. |
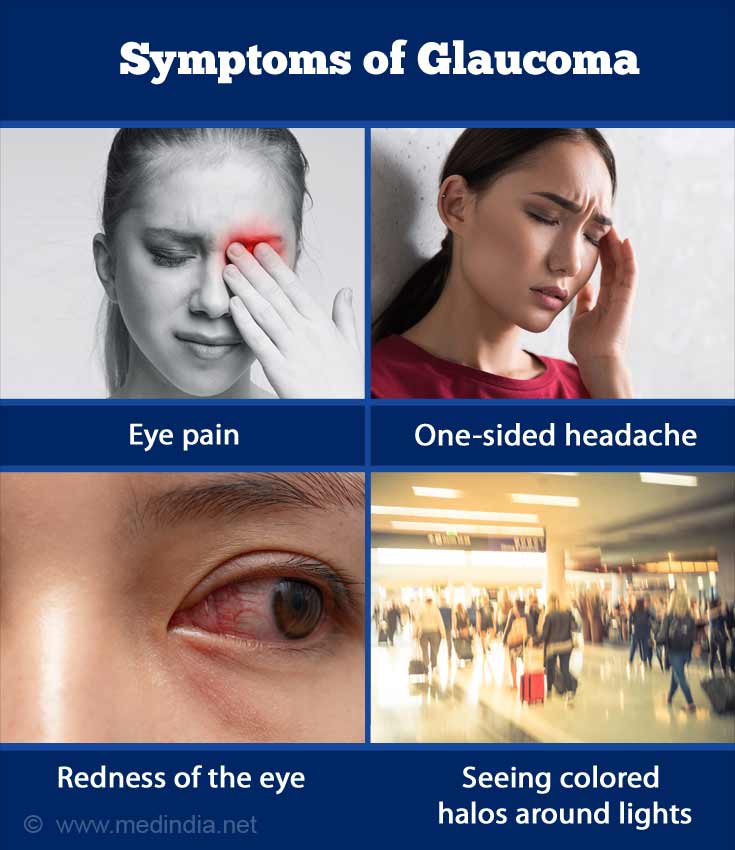
What are the Symptoms of Glaucoma?
The symptoms of glaucoma depend on the type.
Primary open angle glaucoma usually does not cause any symptoms and is often picked up on routine examination. The patient may experience a gradual painless progressive reduction of vision. Because of its non-specific presentation, patients often have significant visual impairment by the time it is diagnosed, and hence POAG is often referred to as a silent killer of vision.
Primary angle closure in its acute stage presents with severe eye pain, one-sided headache, redness of the eye, seeing colored halos around lights and rapid reduction of vision. The triggering factor is dilatation of the pupil – this can occur while watching a movie, in the evenings when the lighting is dim or during dilatation of the pupil in the doctor’s clinic. Often, the pain is severe enough to cause nausea and vomiting – symptoms that may be misleading and lead to misdiagnosis of the actual condition. Acute attacks have sometimes been diagnosed as acute appendicitis! Symptoms subside only with treatment, after which the angle opens up (but still remains narrow). Usually no major sequelae are seen if treated on time.
Sometimes the patient with primary angle closure may not present with the acute stage as just described, but may have intermittent attacks of raised pressure with the above symptoms which get terminated on their own without treatment. Such a patient should be investigated for the possibility of intermittent angle closure attacks.
Chronic angle closure is more common than acute angle closure. Here there is a gradual permanent closure of the angle due to adhesions between the iris and the cornea which cannot be broken. Chronic angle closure clinically presents very similar to primary open angle glaucoma and the only differentiating feature is the presence of a closed angle.
In primary congenital glaucoma, there occurs corneal swelling which can give rise to severe photophobia (abnormal sensitivity to light), tearing and forceful closure of eyelids. The child often buries its head in a pillow as it cannot tolerate light. Also as the sclera is elastic, the eyeball enlarges and looks big; that is why the term buphthalmos or “ox eye”.
How do you Clinically Evaluate for Glaucoma?
Evaluation of glaucoma includes the following:
- A detailed eye examination including vision testing, refraction and slit lamp examination.
- Ophthalmoscopy (examination of the retina) helps to evaluate the optic disc to determine the presence, nature and extent of any glaucomatous cupping.
- Measurement of central corneal thickness (pachymetry).
- Measurement of intraocular pressure (tonometry). The normal intraocular pressure ranges from 10-21 mm Hg. Sometimes, when the intraocular pressure is normal, the doctor will want to repeat the measurements at various times of the day to determine the diurnal variation.
- Gonioscopy (assessment of the angle of the anterior chamber) to determine if it is narrow or wide open, and if there is any additional pathology.
- Perimetry (assessment of the visual field)
- OCT (optical coherence tomography) for quantitative measurement of the optic nerve head and the retinal nerve fiber layer.
- Children younger than 5 years may have to be examined under general anesthesia for better cooperation.
Secondary glaucomas will show features of the cause of the glaucoma in addition to raised intraocular pressure, optic disc and visual field changes.
How do you Treat Glaucoma?
Treatment of glaucoma depends upon the type and stage of the glaucoma. It is important to realize that treatment does not reverse the damage to the optic nerve. It only prevents further damage and subsequent blindness.
Primary Open Angle Glaucoma
The initial treatment is always with pressure lowering eye drops. Treatment is started with one medication and if uncontrolled, more may be added. The goal is to reduce the pressure to a level that prevents further optic disc and visual field damage. If there is failure of adequate pressure control, one can go for laser treatment of the trabecular meshwork or alternately a surgery wherein an enhanced drainage mechanism for aqueous is provided.
Acute Angle Closure
The initial step is to bring down the intraocular pressure to a safe level with intravenous drugs, oral medication and eye drops. This is followed by the definitive treatment which is to make an opening in the iris with a laser (laser iridotomy). This prevents future attacks. This laser treatment has to be carried out in the other unaffected eye as well to prevent such an attack occurring in that eye.
Chronic Angle Closure is usually treated with a filtration surgery.
Secondary Glaucomas are treated based on the causes. This may be medical or surgical.
Primary Congenital Glaucoma is always treated surgically.
Glaucoma surgeries aim to provide enhanced drainage of aqueous, either through the normal channels (such as viscocanalostomy and canaloplasty) or through alternate routes such as trabeculectomy. In trabeculectomy, the drainage pathway may become blocked with scar tissue and become less effective over time. In cases where this is expected such as in neovascular glaucoma and in repeat trabeculectomy, a glaucoma drainage implant is used wherein a tube shunt is used for aqueous drainage. This tube cannot be blocked by scar tissue.
The most important advance in glaucoma surgery is the group of surgeries referred to as minimally invasive glaucoma surgery (MIGS). Here the anterior chamber is not entered (unlike in regular filtration surgery), and so these are considered safer.
What are the Side effects of Anti-glaucoma Medications?
Minor discomfort may be experienced with most of the anti-glaucoma eye drops. Some of them can give rise to redness and burning in the eye, which may improve with time. If the discomfort is excessive, consult your doctor for a possible change in medication.
Most anti-glaucoma medications used over a long time result in dryness of eyes. This is especially true of drugs like Timolol. Your doctor will prescribe ocular lubricants for the same. Timolol can also worsen wheezing in asthmatics, and can affect heart function; it may have to be substituted with another medication if you suffer from these conditions.
A popular class of medications called prostaglandin analogues (e.g. Latanoprost, travoprost, Bimatoprost) can cause increased iris pigmentation. This may especially cause aesthetic problems for individuals with lighter colored eyes undergoing the treatment in one eye. Growth of eyelashes and also pigmentation of the skin around the eyes can occur if care is not taken to avoid spillage.
Brimonidine can cause drowsiness; patients on these eye drops should be wary of driving.
How do you Prevent Glaucoma?
All types of glaucoma cannot be prevented. If a child has primary congenital glaucoma, the parents can undergo genetic counseling to discuss the possibilities of subsequent children developing the disease.
Primary open angle glaucoma cannot be prevented, but regular screening after the age of 40 years (especially in individuals with risk factors) can detect it at a very early stage and thus prevent its progression.
In patients with narrow anatomical angles, laser iridotomy (making an opening in the iris with laser) can prevent acute attacks.
Secondary glaucomas can be prevented to a certain extent by treating the causative disease adequately.
In all types, it is mandatory to arrest the progression as soon as possible, as the damage to the optic nerve cannot be reverted.