- Graft-versus-host disease - (https://medlineplus.gov/ency/article/001309.htm)
- Know About Graft Versus Host Disease - (http://my.clevelandclinic.org/health/articles/graft-vs-host-disease-an-overview-in-bone-marrow-transplant)
- GVHD symptoms - (http://www.cancerresearchuk.org/about-cancer/coping-with-cancer/coping-physically/gvhd/gvhd-symptoms)
- About graft versus host disease (GVHD) - (http://www.cancerresearchuk.org/about-cancer/coping-with-cancer/coping-physically/gvhd/about-graft-versus-host-disease)
- Ibrutinib Relieves Chronic Graft-Versus-Host Disease Symptoms - (https://www.cancer.gov/news-events/cancer-currents-blog/2017/ibrutinib-stem-cell-transplant-gvhd)
- Ratanatharathorn V et al. Chronic graft-versus-host disease: clinical manifestation and therapy. Bone Marrow Transplantation. 2001;28(2):121-129.
- Holtan SG, Pasquini M, Weisdorf DJ. Acute graft-versus-host disease: a bench-to-bedside update. Blood. 2014;124:363-373.
- Shlomchik WD. Graft-versus-host disease. Nat Rev Immunol. 2007;7(5):340-352.
- Lee SJ. Classification systems for chronic graft-versus-host disease. Blood. 2017;129:30-37.
- Jacobsohn DA, Vogelsang GB. Acute graft versus host disease. Orphanet Journal of Rare Diseases. 2007;2:35. doi:10.1186/1750-1172-2-35
What is Graft versus Host Disease?
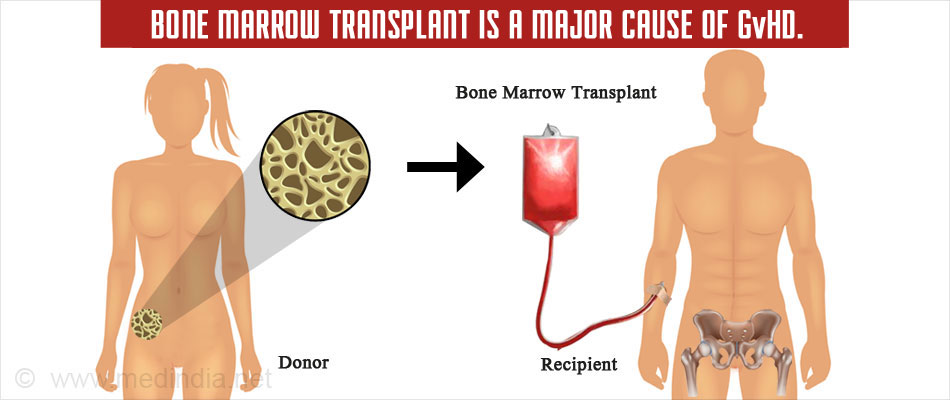
This condition typically occurs during a stem cell or bone marrow transplant from another individual.
GvHD occurs when lymphocytes (immune cells) in the donor tissue encounter antigens of the host tissue, which are seen as foreign, resulting in undesirable manifestations in the host. This is the opposite of transplant rejection wherein the graft tissue is rejected by the host immune cells.
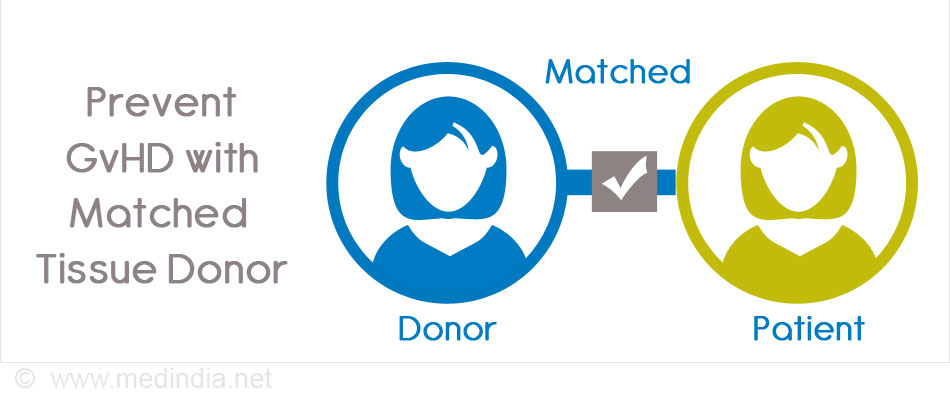
The risk of GvHD is reduced (30% to 40%) when there is increased similarity in the cells and tissues between the donor and the host. The risk of GvHD is higher (60% to 80%) when the donor is unrelated to the host.
What are the Types of Graft versus Host Disease?
There are 2 types of GvHD
Chronic: Patients who have undergone a transplant may exhibit chronic GvHD (cGVHD) symptoms more than 100 days or perhaps several years after the transplant. Sometimes, the reaction may be due to a prior acute GvHD (aGVHD). However, 30% of cGVHD cases occur spontaneously without prior ‘aGVHD’.
Chronic GvHD may involve the lungs, genitourinary tract, eyes, skin, neuromuscular system, liver, mouth, and the gastrointestinal tract.
Acute: Cases of acute GvHD (aGVHD) appear in the host, usually within 100 days. Acute GvHD develops primarily in the liver, gastrointestinal tract, eyes, and skin.
Approximately 5% to 50% of the hematopoietic stem cell recipients develop aGvHD.
What are the Causes of Graft versus Host Disease?
The major causes of GvHD are bone marrow or stem cell transplants.
The risk of GvHD is determined by the
- Age of the individual,
- Source of the stem cells,
- Graft environment (conditioning),
- Presence of cytomegalovirus (CMV) antibodies in the host and
- Measures taken to avoid complications (prophylaxis)
Human Leukocyte Antigens (HLA) are proteins found on the surface of all cells in our body. The immune system (body’s defence mechanism) can recognize HLA antigens that are not belonging to the host (eg donor tissue) and can mount an immune attack against the graft. In graft versus host disease, the reverse occurs.
In acute GvHD, there is a mismatch between the donor and the host in relation to the human leukocyte antigen (HLA). The mismatch causes the donor cells to regard the host environment as foreign. The HLA mismatch can occur in both related or unrelated donors.
Risk factors for aGvHD include -
- Over 30 years of age
- Donors who have been pregnant earlier
In cGvHD, the HLA mismatch may be from a related donor or it could be due to an HLA match from an unrelated donor.
Risk factors for cGvHD include -
- Increased age or
- A prior case of acute GvHD
What are the Symptoms and Signs of Graft versus Host Disease?
The reactions to GvHD range from mild, severe to life-threatening.
There are 3 main organs that are affected by GvHD. They are the -
- Liver,
- Skin,
- Gastrointestinal tract.
Based on the organ involvement and the type of GvHD, the symptoms vary. The organ affected earliest and most often is the skin. The possible clinical features include
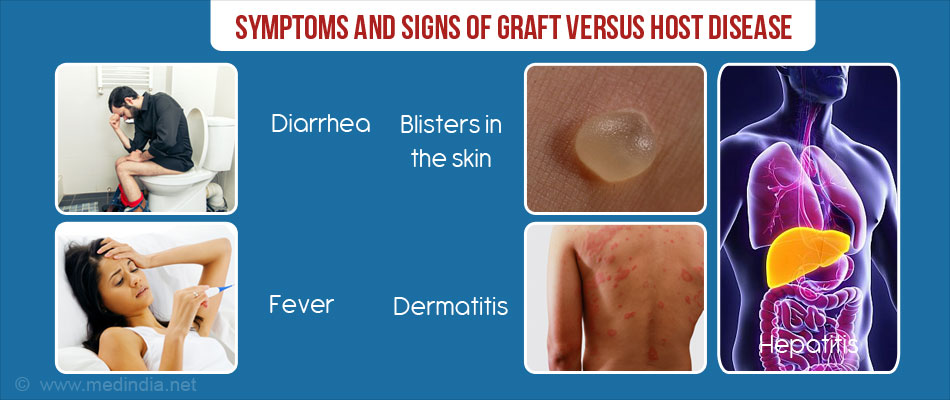
Acute GvHD:
- Fever
- Abdominal cramping (aGvHD of the gastrointestinal tract) in the abdomen without or with diarrhea, constant vomiting and nausea. The diarrhea is green in colour and may contain blood and mucus. There is a loss of appetite as well
- Blisters on the skin or rash in the skin (dermatitis) – The rash may be painful and itchy. The shoulders, palms of feet and hands, and ears get affected with the skin rash
- Hepatitis (high levels of liver enzymes or bilirubin) - Following the transplant, the individual is assessed with liver function tests. Prior to visible symptoms, any changes in the liver function will give an indication of liver problems. Persistent liver damage will cause yellowing of the whites of the eyes and the skin. An enlarged liver causes the abdomen to swell resulting in pain
- Thrombocytopenia
- Anemia
- Low immunity or poor resistance to infections
Chronic GvHD
- Dry eyes with irritation- Ocular GvHD occurs in 40% to 60% of transplant cases. Eyes feel dry, are unable to tolerate dry light, and experience burning and pain.
- Rash on the skin with inflammation- Skin may feel itchy, dry, tight, may thicken, feel bumpy and may be darker in coloration. Nails may become brittle and hard. Hair begins to grey and fall.
- Sensitivities in the oral cavity-There may be sores or fungal infections in the mouth. Chronic GvHD affects the salivary glands resulting in dryness and soreness in the mouth. There is difficulty in swallowing.
- Liver damage- There is scarring and damage to the liver affecting its functioning.
- Digestive system- Chronic GvHD affects the lining of the digestive tract affecting its capacity to absorb nutrients. Individuals experience cramps and a bloated feeling. They also lose appetite and consequently their weight.
- Vaginal damage- Inflammation of the vagina causes problems to have sex.
- Lung damage- There is a risk of chest infections, wheeze, shortness of breath and continuous cough.
- Inflamed tendons- If the tendons (connections between muscles and bones) get inflamed then the movement of limbs is affected.
- Immune deficiency- This condition makes chronic GvHD patients prone to infections and ultimately death.
How to Diagnose Graft versus Host Disease?
Based on the symptoms, one can diagnose acute GvHD. However, sometimes the symptoms could be due to other complications, such as drug reactions or infections.
- A sample of tissue (biopsy) of the affected site is recommended to rule out other complications and confirm GvHD. Biopsies of the gastrointestinal (GI) tract, the skin, and the liver provide clues to confirm GvHD.

- Clinical laboratory tests help to detect decreased platelets (thrombocytopenia), lymphocytes (lymphopenia), hypoalbuminemia, and eosinophilia.
Even in the presence of diagnostic features, such as oral ulcers, dry eyes, and skin lesions, confirmatory tissue biopsies are necessary to confirm the diagnosis. Imaging, tests specific for organs, and specialists help to confirm the diagnosis.
How do you Treat Graft versus Host Disease?
Acute graft versus host disease is graded on a scale of 0 to IV depending on the number of organs involved and the severity of the reaction with 0 being the mildest form and IV representing severe disease.
- In acute GvHD, the predominant form of treatment for matched donor transplants involves a short duration of suppressing the immune system (the body’s defence mechanism) using methotrexate combined with tacrolimus or cyclosporine.
- For high-risk transplants, immune suppression is performed by depleting the immune T cells in the donor marrow.
- Mycophenolate mofetil (MMF) is used to treat reduced-intensity transplants (mini transplant) where the blood forming cells of the patient are replaced with stem cells from a compatible donor.
- Corticosteroids, such as methylprednisolone is used but only ~ 40% to 50% of the patients respond to the drug.
- The non-responders to corticosteroid treatment are subjected to salvage (second line) immunosuppressive therapy. Pentostatin, anti-thymocyte globulin (ATG), infliximab, daclizumab, sirolimus, and mesenchymal cells are some examples of salvage therapy.
It is not easy to treat chronic GvHD because of the problems with the immune system, the bone marrow, the multiple organs that are affected, and the progressive development of the condition.
- If chronic GvHD develops on its own or much later following acute GvHD, then corticosteroid treatment, cyclosporine, and tacrolimus therapies are effective.
- However, if chronic GvHD develops immediately after acute GvHD, these patients respond poorly to corticosteroid treatment.
- Early symptoms of chronic GvHD can be treated with immunosuppression by corticosteroids. However, the symptoms reappear once the treatment is gradually tapered off.
- Chronic GvHD of the skin responds to hydroxychloroquine, etritrenate, UVB (shortwave ultraviolet B), and light therapy (extracorporeal photopheresis).
T-cell treatments, such as etanercept and infliximab have been effective in treating chronic cGvHD (Ratanatharathorn). However, so far, there is no FDA-approved drug to help treat these chronic GvHD. Clinical trials have found drugs, such as ibrutinib to be effective symptoms.
How do you Prevent Graft versus Host Disease?
The ideal way to prevent GvHD is to get the best possible tissue-matched donor.
Available treatments, such as tacrolimus and thalidomide have not been very effective in preventing GvHD. Tacrolimus is used to treat acute GvHD but has been found to increase the risk of chronic GvHD. Thalidomide is used to treat chronic GvHD but has also been found to increase the incidence of chronic GvHD.
Immune T-cell depletion during stem cell transplants has been found to be effective in preventing the risk of acute and chronic GvHD.
What is the Prognosis of Graft versus Host Disease?
If the donor is a related tissue match, then the risk of GvHD is reduced.
The prognosis of GvHD varies based on:
- The type of transplant
- The kind of organ that is affected
- The presence of infections
Although GvHD may be prevented, there is no assurance that the transplant may be successful.
- Grade I and II acute GvHD have nearly 80% chances of survival but these chances reduce with increasing severity of acute GvHD with grade IV having only a 5% chance of survival.
- In chronic GvHD, infections are a main cause of death. The treatment phase for chronic GvHD may extend for months and even years.