- How Can Hemolytic Anemia Be Prevented? - (http://www.nhlbi.nih.gov/health/health-topics/topics/ha/prevention)
- Hemolysis - (https://medlineplus.gov/ency/article/002372.htm)
- Edema and Hemolytic Anemia in Premature Infants - A Vitamin E Deficiency Syndrome - (http://www.nejm.org/doi/full/10.1056/nejm196811282792202)
- Hemolytic disease of the newborn - (http://www.ncbi.nlm.nih.gov/books/nbk2266/)
- What Causes Hemolytic Anemia? - (https://www.nhlbi.nih.gov/health/health-topics/topics/ha/causes)
- Anemia, Hereditary Nonspherocytic Hemolytic - (http://rarediseases.org/rare-diseases/anemia-hereditary-nonspherocytic-hemolytic/)
- Hemolytic Anemia in Children - (http://www.stanfordchildrens.org/en/topic/default?id=hemolytic-anemia-in-children-90-p02321)
- Hemolytic Anemia - (http://www.hopkinsmedicine.org/healthlibrary/conditions/hematology_and_blood_disorders/hemolytic_anemia_85,p00076/)
- Introduction About Hemolytic Anemia? - (https://www.nhlbi.nih.gov/health/health-topics/topics/ha)
- What is Hemolytic Anemia - (http://www.aafp.org/afp/2004/0601/p2599.html)
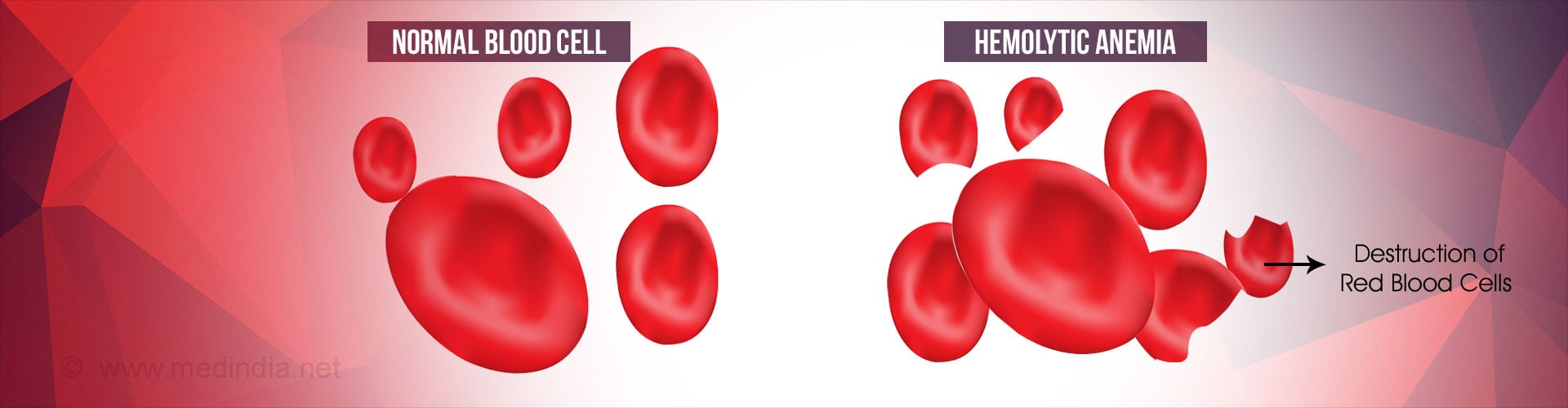
What is Hemolytic Anemia?
Hemolytic anemia is a disorder where the body destroys red blood cells (RBCs), which are removed from the system before their normal life span of 120 days is over. Destruction of red blood cells is termed as hemolysis.
This condition results in anemia when the formation of red blood cells by the bone marrow cannot match the pace of their destruction.
What are the Causes of Hemolytic Anemia?
Depending on the cause, hemolytic anemia can be classified into two main types - intrinsic and extrinsic
1. Intrinsic Hemolytic Anemia
Intrinsic hemolytic anemia is also often referred to as inherited hemolytic anemia. This occurs due to a defect in the red blood cells which leads to their destruction. Sickle cell anemia, hereditary spherocytosis, anemia due to glucose-6-phosphate dehydrogenase (G6PD) deficiency, hereditary elliptocytosis (ovalocytosis), and thalassemia are some conditions that lead to this type of anemia. The red blood cells in these anemias don’t last as long as normal red blood cells. Since they have a defect, they are taken by the spleen and destroyed early, resulting in anemia.
2. Extrinsic Hemolytic Anemia
In this type of hemolytic anemia, normal red blood cells are produced by the bone marrow but during their course in the blood, they are trapped by the spleen and destroyed.
Some of the possible causes of extrinsic hemolytic anemia are:
- Autoimmune disorders such as lupus, Wiskott-Aldrich syndrome (characterized by abnormal immune system function), rheumatoid arthritis, ulcerative colitis and autoimmune hemolytic anemia.

- Infections with microorganisms like hepatitis virus, Escherichia coli, typhoid fever, cytomegalovirus (CMV), Epstein-Barr virus (EBV), Mycoplasma pneumoniae, or streptococcus.
- Intake of medications like penicillin, anti-malarial medications, sulfa medications, or acetaminophen
- Overactive or enlarged spleen
- Certain tumors and blood cancers like leukemia and lymphoma hemolytic anemia
What are the Symptoms of Hemolytic Anemia?
Some patients with hemolytic anemia may not have symptoms for years while in others, it can produce acute symptoms. The most common symptoms of this condition are:
- Paleness of the skin or yellowish skin
- Fever
- Abdominal pain
- Confusion
- Light-headedness
- Weakness or inability to perform regular tasks or physical activity
- Increased heart rate also known as tachycardia. The doctor may detect the presence of a heart murmur on examination
- Dark colored urine due to jaundice
- Enlargement of spleen and liver
How is Hemolytic Anemia Diagnosed?
Hemolytic anemia is diagnosed based on the history from the patient or the family, physical examination, and blood and bone marrow tests.
- Blood tests: The following blood tests may be necessary for the diagnosis of hemolytic anemia:
- Complete blood count: A complete blood count will indicate a reduced number of red blood cells
- Hemoglobin level: The hemoglobin level is low in hemolytic anemia
- Reticulocyte count: The number of immature red blood cells called reticulocytes in the blood is higher than normal. This indicates an attempt of the bone marrow to make up for the reduced number of red blood cells in the circulation
- Peripheral smear: An abnormal shape of red blood cells may be noted in some of the genetic disorders affecting red blood cells
- Bilirubin level: The breakdown of red blood cells causes an increase in the bilirubin level in the blood, which is responsible for the yellowish discoloration of the skin
- Lactate dehydrogenase level: The level of the enzyme lactate dehydrogenase in the blood is also increased
- Haptoglobin level: The hemoglobin that is released from the red blood cells binds to a protein called haptoglobin in the blood, and is excreted through the urine. The level of haptoglobin in the blood is therefore low
- Coombs’ test: Coombs’ test is used to detect the presence of antibodies that destroy the red blood cells
- Glucose-6-phosphate dehydrogenase levels: The level of the enzyme glucose-6-phosphate dehydrogenase in the blood is reduced in patient with this deficiency

In this procedure, a small amount of bone marrow is taken from the hip bone and analyzed to see the number, size, maturity and absence/presence of abnormal/normal red blood cells
How is Hemolytic Anemia Treated?
Treatment of hemolytic anemia depends on various patient factors, which include:
- Age
- Medical history
- Severity of the condition
- Cause of the disease
- Tolerance to medications
Treatment includes:
- Blood transfusion in case of severe anemia. Exchange transfusion may be done, where blood is transfused to the patient and an equal amount of blood is removed to prevent fluid overload
- Corticosteroid medications or other drugs that reduce immunity (immunosuppressive drugs) to reduce hemolysis due to autoimmune disease
- The antibodies from the blood may be removed through a process called plasmapheresis
- Hydroxyurea is used in the treatment of sickle cell disease
- Surgical removal (splenectomy) of an enlarged or diseased spleen may be done if necessary
How can Hemolytic Anemia be Prevented?
Some ways to prevent episodes of hemolytic anemia include the following:
- Factors that precipitate a hemolytic attack in sickle cell anemia like dehydration and low oxygen levels should be avoided
- A thorough testing of the blood group and the Rh factor should be done before a blood transfusion
- Avoid intake of medications that can precipitate hemolysis especially if you are suffering from glucose-6-phosphate dehydrogenase (G6PD) deficiency