- Herniated disc - (http://www.mayoclinic.org/diseases-conditions/herniated-disk/home/ovc-20271246)
- Incidence and risk factors of herniated lumbar intervertebral disc or sciatica leading to hospitalization - (https://www.ncbi.nlm.nih.gov/pubmed/3818881)
- Herniated lumbar disc - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2907819/)
- Familial predisposition for lumbar degenerative disc disease. A case-control study. - (https://www.ncbi.nlm.nih.gov/pubmed/9589542)
- Herniated disc in the lower back - (http://orthoinfo.aaos.org/topic.cfm?topic=a00534)
- About herniated disc - (https://my.clevelandclinic.org/health/articles/herniated-disc)
- Knezevic NN, Mandalia S, Raasch J, Knezevic I, Candido KD. Treatment of chronic low back pain - new approaches on the horizon. J Pain Res. 2017 May 10; 10: 1111-23. doi: 10.2147/JPR.S132769 . eCollection 2017. PMID: 28546769.
- Hooten WM, Cohen SP. Evaluation and treatment of low back pain: a clinically focused review or primary care specialists. Mayo Clin Proc. 2015 Dec; 90(12):1699-718. doi: 10.1016/j.mayocp.2015.10.009 . PMID: 26653300.
- Jordan J, Konstantinou K, O'Dowd J. Herniated lumbar disc. BMJ Clin Evid. 2011 Jun 28; 2011. pii: 1118. PMID: 21711958.
- Hahne AJ, Ford JJ, McMeeken JM. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine (Phila Pa 1976). 2010 May 15; 35(11): E488-504. doi: 10.1097/BRS.0b013e3181cc3f56 . PMID: 20421859.
- Matsui H, Kanamori M, Ishihara H, Yudoh K, Naruse Y, Tsuji H. Familial predisposition for lumbar degenerative disc disease. A case-control study. Spine (Phila Pa 1976). 1998 May 1; 23(9): 1029-34. PMID: 9589542
- HeliÖvaara M, Knekt P, Aromaa A. Incidence and risk factors of herniated lumbar intervertebral disc or sciatica leading to hospitalization. J Chronic Dis. 1987; 40(3): 251-8. PMID: 3818881.
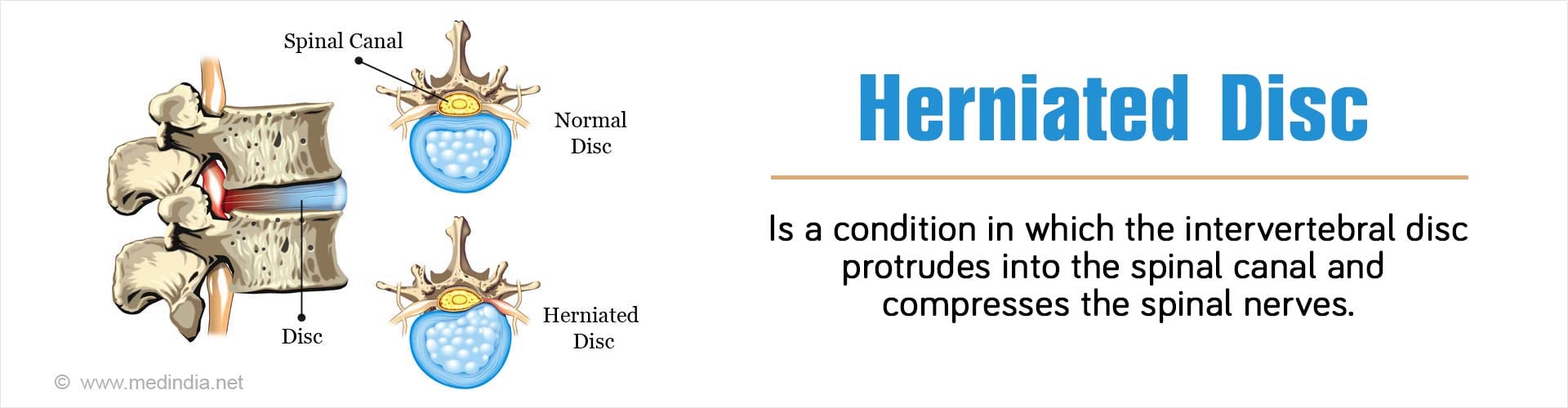
What is Herniated Disc?
Herniated disc is said to occur when the intervertebral disc between the two vertebrae of the spine protrudes or herniates into the spinal canal and compresses the spinal nerves that travel through the canal. This compression of the nerve can lead to lower back pain that can be mild to severe and sometimes the pain can radiate down to the affected limb.
Majority (95%) of herniated discs occur at the lower lumbar spine (L4/5 and L5/S1 level). It is important to differentiate herniated disc with spinal cord compression, or cauda equina syndrome. These require emergency intervention.
Diagnosis can be done using MRI investigation. However, one must also note that 19-27% of people without symptoms also may have disc herniation on imaging.
How Common is Herniated Disc?
Herniated disc is a common condition. The highest prevalence of herniated disc is among people aged between 30-50 years. It is more common in men and the male to female ratio of its occurrence is 2:1. It is interesting to note that the incidence of disc herniation drops in the elderly especially after the age of 80 years.
What Causes Herniated Disc?
The following risk factors can cause a herniated disc:
- Sedentary Lifestyle: A sedentary lifestyle predisposes to development of a herniated disc. Regular exercise is required to keep the body toned, and prevent the occurrence of a herniated disc.
- Gender: Men are more likely to develop a herniated disc, which usually occurs in the age-group between 30 to 50 years.
- Body Weight: Being overweight puts much more pressure on the lower back, thereby causing stress on the vertebral column, which can lead to a herniated disc.
- Bad Posture while Lifting: While lifting heavy weights, if the back muscles are used instead of the leg muscles, then there is a chance of developing a herniated disc. Twisting rapidly while lifting also has the same effect.
- Repetitive Strenuous Activities: Certain types of occupation involve repetitive strenuous activities like lifting, bending, twisting, pulling, and climbing. In the absence of proper posture maintaining techniques while performing these activities, a herniated disc may occur.
- Genetic Factor - There may also be a genetic factor in the development of lumbar disc herniation as an expression of disc degeneration.

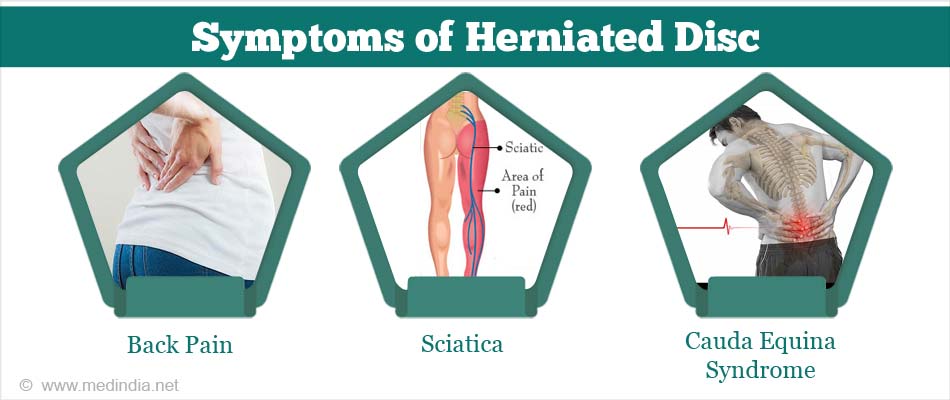
What are the Symptoms of Herniated Disc?
Very often a herniated disc may not produce any symptoms. However, when symptoms do occur, they can be quite severe.
Symptoms Due to Lumbar Disc Herniation:
- Back Pain: This is a common symptom of a herniated disc in the lower back or lumbar region.
- Sciatica: Severe pain can radiate down either leg, eventually reaching the ankles and feet. This type of pain is called sciatica or sciatic pain.
- Numbness/Tingling Sensation: This type of sensation can occur in the legs and/or feet when the sensory nerves are affected.
- Muscle Weakness: The legs can become very weak and unable to bear the weight of the body if the motor nerves are involved.
- Cauda Equina Syndrome: This is an extremely rare condition, which occurs due to compression of the spinal nerve roots and causes loss of bladder and/or bowel control. If this syndrome occurs, immediate surgical intervention is required.
Symptoms Due to Cervical Disc Herniation:
- Neck Pain: Neck pain is especially evident on the sides and the back of the neck. The pain can get aggravated when the neck is bent and turned around.
- Muscle Spasms: Spasms may occur in the muscles of the neck.
- Radiating Pain: Pain can occur near the shoulder blade, which radiates to the shoulder, arm, and even the hand and fingers.
How do you Diagnose Herniated Disc?
In order to diagnose a herniated disc, first your doctor will take a detailed Medical History, followed by a Physical Examination, which includes the following:
- Neurological Assessment: The doctor will assess the strength of the muscles in your thighs, ankles and toes. He/she will also check whether there is any sensory loss, which is indicated by numbness experienced while gently touching the feet. Additionally, the knee and ankle reflexes will also be assessed.
- Straight Leg Raised (SLR) Test: This is a special type of neurological test used for young people (below 35 years). Here, you will be asked to lie down on your back. The doctor will lift the affected leg upwards, keeping the leg straight without any bending at the knees. If you feel pain in the leg below the knees, you are most probably suffering from a herniated disc.
If you test positive by the SLR test, you will be advised to undergo imaging and certain other tests to confirm the diagnosis. These are briefly described below:
- X-Ray: An x-ray of the spine is done to rule out any other causes of back pain, besides that due to a herniated disc.
- Magnetic Resonance Imaging (MRI): MRI scan can be used for clinching the diagnosis as it can detect the narrowing of the spinal canal due to herniation. It can also create detailed images of soft tissues like the intervertebral discs.
- Computed Tomography (CT) Scan: In case MRI cannot be done, the next best option is a CT scan, which can produce sliced images of the spinal canal and associated vertebrae to detect disc herniation.
- Myelography: In this technique a radio-opaque dye is injected into the spinal canal and images are taken to detect the location and size of the herniation. In this procedure, the imaging can be done using x-rays, MRI or CT scan.
- Electromyogram and Nerve Conduction Studies: Electromyogram and nerve conduction studies may be performed to test which nerves are affected.
What is the Treatment for Herniated Disc?
Drug Treatments
In an extensive review of literature it was found that there is little scientific evidence to suggest that drug treatments are effective in treating herniated disc. The evidence indicates that:
- Analgesics, antidepressants, or muscle relaxants are not effective in people with herniated disc.
- Non-steroidal anti-inflammatory drugs (NSAID) and cytokine inhibitors such as glucocorticoids like prednisone do not improve symptoms of sciatica caused by disc herniation.
- There is no evidence to suggest that epidural injections of corticosteroids are effective for treating herniated disc.
Non-Drug Treatments
Non-drug treatments also appear to be largely ineffective in improving the condition of patients with herniated disc. The evidence suggests that:
- Although spinal manipulation could be useful for relieving local or radiating pain in patients with acute back pain and sciatica with disc protrusion, there may be further herniation from spinal manipulation in patients who will undergo surgery.
- Bed rest and traction are not effective in treating patients with sciatica caused by disc herniation.
- There is insufficient evidence to suggest that staying active, exercising or other procedures like acupuncture, massage, heat or ice treatments have any effect in patients with herniated disc.

Surgery
Only surgical intervention by standard discectomy or microdiscectomy seems to improve the condition.
Standard Discectomy: A standard discectomy involves the surgical removal, in part or whole, of an intervertebral disc, without using an operating microscope (as opposed to a microdiscectomy). A 5-cm incision is made over the region where the disc is herniated. The affected part of the spine is exposed and once the herniated disc is identified, it is excised and the wound is closed.
Microdiscectomy: This is a minimally invasive surgical procedure, where the surgeon uses a special type of microscope to provide a close-up view of the surgical field. In this procedure, the herniated portion of the disc is excised, thereby relieving pressure on the nerve root, which then slowly heals. Microdiscectomy is generally very successful and instantly relieves leg pain (sciatica) arising from a lumbar herniated disc. However, complete recovery may take up to several weeks. In case of the neck, along with discectomy, the neighboring vertebrae may be fused together (spinal fusion) to prevent movement at that level.
Comparison of Standard Discectomy vs. Microdiscectomy: Three randomized controlled trials (RCT) compared 293 patients with herniated disc who had undergone either standard discectomy or microdiscectomy. It was found that there was no significant difference with reference to the following parameters:
- Patients’ perception of the outcome of surgery after 1 year: Same in both groups.
- Pain in the legs or back: Same in both groups.
- Time taken to return to work: 10 weeks in both groups.
What are the Complications of Herniated Disc?
If the herniated disc is not treated, the following complications may occur:
- Pain: Chronic back pain (due to lumbar disc herniation) may occur, which can produce sciatica, resulting is severe leg pain. In case of cervical disc herniation, severe neck pain as well as pain in the shoulder and arms can occur.
- Loss of Sensation: Sometimes, there may be loss of sensation in the legs and feet.
On the other hand, if the herniated disc is treated by surgery, the following complications may occur:
- Infections: Post-surgical infection can occur.
- Hematoma: Internal bleeding can cause the formation of a large blood clot, technically termed as hematoma, which can cause nerve compression and severe pain.
- Nerve Damage: This can occur due to inefficient planning and execution of the surgery.
- Recurrent Disc Herniation: There is some chance (about 10-15 percent) that the same disc may herniate again. Usually happens in the first six weeks after surgery, but it can occur anytime and this may require a second operation. It is more common when a minimally invasive approach like micro-dissectomy is undertaken.
- Difficulty with Urination: Rarely there maybe problem with urinary system and symptoms may include -
- Involuntary urination
- Urgency - Feeling sudden urge(s) to urinate
- Frequent bathroom visits
- Bladder may not completely empty leaving residual urine needing drainage
- Overfilling of bladder and leakage of urine
- Intermittent leakage of urine
Is it Possible to Prevent Herniated Disc?
Although it may not be possible to entirely prevent herniated disc, certain precautionary measures can be taken to reduce the risks appreciably. These are briefly highlighted below:
- Maintain Good Posture: Practice a good posture at all times – while standing, walking, sitting and sleeping. Avoid sitting in one place for too long.
- Practice Proper Lifting Techniques: While lifting weights, do not bend at the waist but instead bend at the knees. Keep your back straight and use the lower limb muscles to lift the weight.
- Maintain Proper Weight: Maintain the correct weight for your height as excess weight puts pressure on the lower back.
- Exercise Regularly: Regular exercise is good for maintaining muscle tone and to increase the weight-bearing capacity of the muscles. While sitting for long periods, stretch as often as you can.
- Do Not Smoke: Since smoking can predispose to disc degeneration, avoid smoking.
What is the Prognosis of Herniated Disc?
The prognosis is generally good for people with herniated disc. Most people recover with conservative therapy within 6 weeks. Some however still have persisting pain and require surgical intervention. The prognosis of microdiscectomy is generally very good and most patients improve and completely recover within several weeks.
Health Tips
1. Exercise regularly: Regular exercise strengthens the trunk muscles and helps stabilize and support the spine.
2. Maintain good posture: Always maintain good posture as this helps to reduce pressure on the spine and intervertebral discs. Keep your back straight and vertically aligned, especially while sitting for long periods. While lifting heavy weights, let your lower limb muscles (not your back muscles) do the work.
3. Maintain a healthy weight: Excessive weight puts pressure on the spine and discs and predisposes to disc herniation.
4. Eat a healthy diet: Consume a balanced diet with plenty of fiber, proteins and fruits. Drink plenty of water and avoid carbohydrates and fat in your diet.