- What is calcium and what does it do? - (https://ods.od.nih.gov/factsheets/calcium-consumer/)
- Davidson's Principles and Practice of Medicine - 21st edition
- Hypercalcemia - (http://www.mayoclinic.org/diseases-conditions/hypercalcemia/basics/definition/con-20031513)
- Know About Hypercalcemia - (https://medlineplus.gov/ency/article/000365.htm)
What is Hypercalcemia?
Hypercalcemia refers to increase in serum calcium levels. and includes serum calcium levels that are >10.5 mg/dL (or >2.5 mmol/L).
Only 2 percent of calcium circulates throughout the body in the blood serum, the rest being present in the skeleton. Serum refers to blood devoid of blood cells. Out of the circulating calcium, (which is the total serum calcium) only one half of it referred to as the free or ionized form is capable of physiologic effects. The remainder is bound to proteins like albumin and globulin and other inorganic molecules.
Since calcium is found as bound and ionic forms in the blood circulation, measurements of calcium levels in the body are based on the total serum calcium levels or ionized calcium levels.
Normal total serum calcium levels are 8.6-10.4 mg/dL (2-2.4 mmol/L) and normal ionized srum calcium levels are 4-5.5 mg/dL (1-1.3 mmol/L).
- Mild hypercalcemia: Total serum calcium = 10.5-11.9 mg/dL (2.5-3 mmol/L) or Ionized calcium = 5.6-8 mg/dL (1.4-2 mmol/L)
- Moderate hypercalcemia: Total serum calcium = 12-13.9 mg/dL (3-3.5 mmol/L) or Ionized calcium = 8-10 mg/dL (2-2.5 mmol/L)
- Hypercalcemic crisis: Total serum calcium = 14-16 mg/dL (3.5-4 mmol/L) or Ionized calcium = 10-12 mg/dL (2.5-3 mmol/L)
Too much of calcium is known to cause stones in the kidney, make the bones weak and cause problems of the heart and brain.
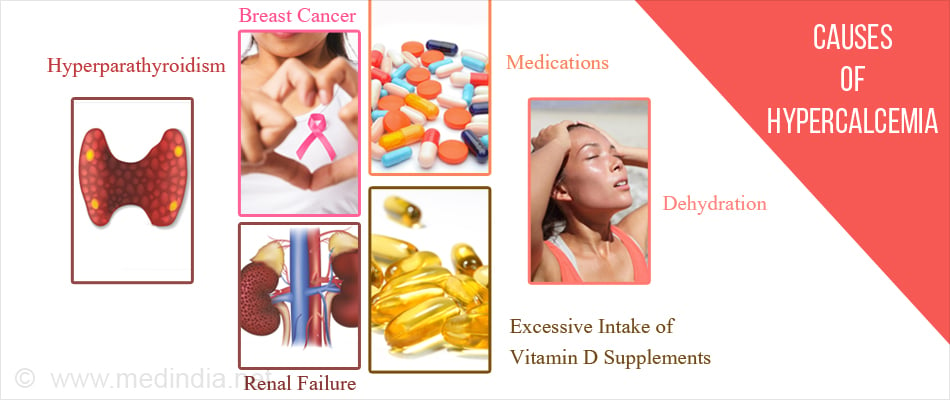
What are the Causes of Hypercalcemia?
Hypercalcemia occurs mostly due to overactive parathyroid glands. Other causes which contribute include cancer, certain other medical disorders, some medications, and excessive use of calcium and vitamin D supplements.
- Overactive parathyroid glands: The most common cause of hypercalcemia is hyperparathyroidism due to a noncancerous tumor in one or more of the four small grain sized parathyroid glands situated behind the thyroid gland.
- Cancer: Lung cancer, breast cancer, and some blood cancers, can increase the risk of hypercalcemia. The risk also increases with metastasis (spread of cancer) to the bones.
- Other diseases: Calcium absorption is stimulated due to raised vitamin D levels in diseases where lumps or granulomas are formed like tuberculosis and sarcoidosis.
- High bone turnover due to:
- Hyperthyroidism
- Immobilization – People who are usually sitting or lying down due to immobility due to fractures or paralysis eventually develop hypercalcemia as their non-weight bearing bones demineralize (break down). Ex: Paget’s disease
- Use of the diuretic Thiazide
- Vitamin A toxicity
- Renal failure (milk-alkali syndrome)
- Medications: Drugs such as lithium, used to treat bipolar disorder, may increase the release of parathyroid hormone causing hyperparathyroidism and hence hypercalcemia.
- Supplements: Taking excessive amounts of calcium or vitamin D supplements over a period of time can elevate calcium levels in the blood above normal range leading to hypercalcemia.
- Hereditary factors: Familial hypocalciuric hypercalcemia is a rare genetic disorder which causes increased calcium in the blood due to faulty calcium sensing receptors [CaSR] that have undergone mutations.
- Dehydration: Mild or transient hypercalcemia is caused due to dehydration; as there is less fluid, calcium concentrations rise.
- Other causes:
- Idiopathic infantile hypercalcemia (William’s Syndrome)
- A rare genetic metabolic syndrome called Blue Diaper Syndrome
- A fatal metabolic bone disease called hypophosphatasia that is characterized by defective mineralization
What are the Symptoms of Hypercalcemia?
If the hypercalcemia is mild, then the patient might have no symptoms. In cases of severe hypercalcemia, the symptoms are felt in the particular parts of the body that are affected.
- Renal system: Excess calcium must be filtered out. This can lead to excessive thirst called polydipsia and frequent urination called polyuria.
- Digestive system: Excess calcium can lead to nausea, vomiting and constipation (inability to pass stools easily) and anorexia (loss of appetite).
- Integumentary system: The excess calcium comes from excess bone resorption (break down of bones) which weakens them. This causes bone pain. Excess calcium can also present as muscle weakness.

- Central Nervous system: Excess calcium can interfere with brain functioning, resulting in confusion, lethargy, fatigue and coma.
- Cardiac: Arrhythmias and syncope due to calcium’s positive inotropic effects.
What are the Risk factors for Hypercalcemia?
Any risk factor that puts a person at a risk for developing hyperparathyroidism or having overactive thyroid glands is also a risk factor for hypercalcemia.
- Women in their 50s
- People with a family history of hyperparathyroidism or hypercalcemia.
How do you Diagnose Hypercalcemia?
- Hypercalcemia as mentioned above is classified based on serum and ionized calcium levels. Thus serum calcium levels must be checked routinely to find out which category it falls under. In malignancy the calcium levels increase rapidly, whereas in overactive parathyroids it is milder.
- Serum PTH (parathyroid hormone), serum PTHrP (PTH-related protein) should simultaneously be measured.
- Serum vitamin D levels, urine calcium, serum phosphate, serum alkaline phosphatase, serum chloride, serum bicarbonate and thyroid function may be useful in some cases.
How do you Treat Hypercalcemia?
People with mild hypercalcemia can choose to wait and watch while periodically monitoring the health of their bones and kidneys. Severe hypercalcemia requires a hospital stay and treatment with fluids and medications. Surgery is another option.
- Calcimimetics: These drugs mimic calcium and hence could replace calcium in the blood and can control overactive parathyroids.

- Bisphosphonates: These are intravenous osteoporosis drugs used to rebuild bones. Eg: Pamidronate, Zoledronic acid.
- Prednisone: These are steroids which help in Vitamin D dependent hypercalcemia.
- Denosumab: It is a monoclonal antibody (a class of drugs) which helps in the treatment of osteoporosis.
- Calcitonin: It is a hormone produced by parafollicular cells of thyroid whose action is the reverse of parathormone i.e. it lowers blood calcium levels.
- Furosemide with intravenous (IV) fluids: This treatment is for hypercalcemic crisis wherein, in the immediate management it is essential to excrete out excess calcium promptly in order to prevent central nervous system and cardiac damage.
- Peritoneal dialysis or hemodialysis: These are done when kidneys are damaged where dialysis machine plays the role of the kidney in filtering out wastes from the body.
- Surgical correction of hyperparathyroidism: This is useful in conditions of primary hyperparathyroidism. Usually only one of the four parathyroid glands might be affected and surgery can help by removing the malfunctioning gland.
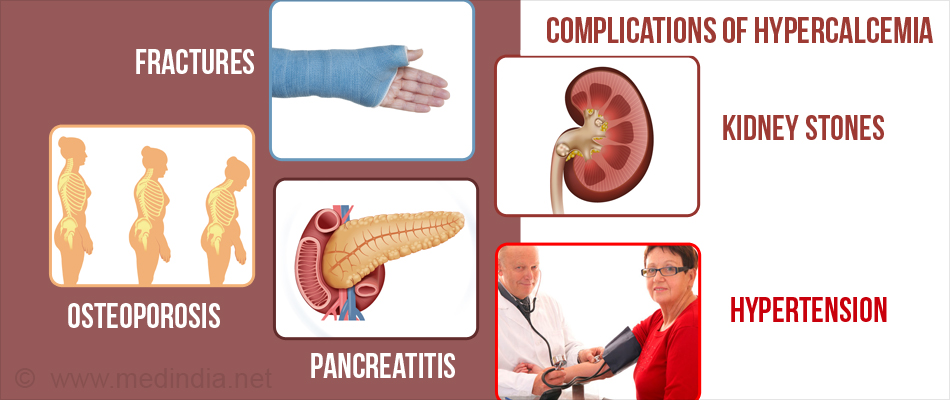
What are the Complications of Hypercalcemia?
- Osteoporosis: Osteoporosis is a disease in which the bone gets ‘thinned out’ due to the break down or demineralization of the bone i.e. the bone melts down and calcium is released into the blood stream. Excess bone resorption makes the bones weak and prone to fractures.
- Bone cysts: These are simple, benign (non-cancerous), fluid-filled lesions in the bones, characteristic of hyperparathyroidism.
- Fractures: These occur due to the fragile bones that result due to excess calcium lost as a result of hypercalcemia.
- Pancreatitis: This occurs as high levels of calcium acts as a stimulus for proteases which are digestive enzymes. These in excess produce pancreatitis.
- Peptic ulcer: This occurs via secretion of the enzyme gastrin which, when in excess leads to formation of peptic ulcer.
- Kidney stones: If there is too much calcium in the urine, crystals might form in the urinary tract. These crystals may combine and form kidney stones and passing a stone can be extremely painful.
- Kidney failure: Severe hypercalcemia can be harmful to the kidney; such damaged kidneys can no longer filter the blood efficiently.
- Hypertension: High blood pressure can occur due to renal insufficiency.
- Dehydration: This may occur due to improper functioning of the kidneys.
- Central nervous system problems: Severe hypercalcemia can lead to confusion, dementia and coma, which can be fatal.
- Depression: This is a psychiatric symptom occurring due to excess calcium.
- Abnormal heart rhythm (arrhythmia): Hypercalcemia affects the electrical impulses of the heart causing it to beat irregularly.
How do you Prevent Hypercalcemia?
The causes for hypercalcemia as such cannot be prevented but
- Maintaining a healthy lifestyle may help prevent many complications of the disease to develop in due course.
- Drinking plenty of fluids is essential to keep you away from dehydration and prevent kidney stones.
- Exercising is again key to stay fit and to keep your bones healthy and maintain bone density. Strength training must be combined with weight bearing exercises.
- Smoking must be stopped as it increases bone destruction and increases comorbid factors and other risk factors.