- About Hypokalemia - (https://en.wikipedia.org/wiki/hypokalemia#signs_and_symptoms)
- Hypokalemia - (https://rarediseases.org/rare-diseases/hypokalemia/)
What is Hypokalemia?
Hypokalemia is defined as low potassium level in the blood. Potassium is an electrolyte whose concentration within the cells is higher than outside the cells i.e. in the blood. The potassium levels as measured in the laboratory indicate the blood levels of potassium, and not the levels within the cells.
Normal potassium levels in the blood serum range from 3.5 to 5.0 mEq /l. Low blood potassium levels is referred to as hypokalemia, while high blood potassium levels are referred to as hyperkalemia.
Hypokalemia can range from mild to severe.
- Mild - serum potassium level ranges from 3-3.5 mEq /L.
- Moderate - serum potassium level ranges between 2.5-3 mEq /L.
- Severe – serum potassium level is below 2.5 mEq /L
Serum refers to the liquid portion of the blood that does not clot, which is used for measuring potassium levels.
How are Potassium Levels Maintained at Normal Levels?
Potassium is obtained from the diet and excreted through the kidneys. It is essential that potassium levels are tightly regulated by physiological mechanisms. The adrenal glands and the pancreas play an important role in maintaining blood potassium levels. The adrenal glands secrete a hormone called aldosterone, which increases excretion of potassium via the urine, while the pancreas secrete insulin, which drives potassium into body cells, thereby reducing its blood level. Alterations in serum potassium levels such as hypokalemia can be potentially life-threatening unless promptly addressed.
Potassium is critical to the normal functioning of muscle and nerve cells. Hypokalemia therefore predominantly affects muscle and nerve function.
What are the Causes of Hypokalemia?
Hypokalemia may be caused by one or more of the following factors:
- Inadequate intake of potassium
- Excessive loss of potassium from the body
- Shift of potassium from the blood (extracellular fluid) into the cells
Inadequate intake in the diet – This is a rare cause of hypokalemia
Excessive loss from body
- Chronic kidney failure
- Severe vomiting and diarrhea
- Diuretic drugs like furosemide and hydrochlorothiazide by causing excessive urination
- Laxative abuse leading to excessive loss from the digestive tract
- Excessive sweating
- Alcohol abuse (causes hypokalemia by various mechanisms)
- Conditions causing excessive aldosterone secretion e.g. primary hyperaldosteronism
- Deficiency of magnesium
- Metabolic alkalosis, a condition marked by increased blood pH, which promotes potassium excretion by the kidneys. It also increases entry of potassium into cells

Shift of potassium from the blood (extracellular fluid) into the cells (thereby reducing blood levels)
- Excess insulin administration
- Drugs such as salbutamol and salmeterol (beta-2 stimulants), and theophylline which are used to treat asthma
- Administration of epinephrine, a drug of emergency
- Over-energetic treatment of vitamin B12 or folate deficiency
- Familial periodic paralysis, which is a genetic disorder characterized by episodes of hypokalemia
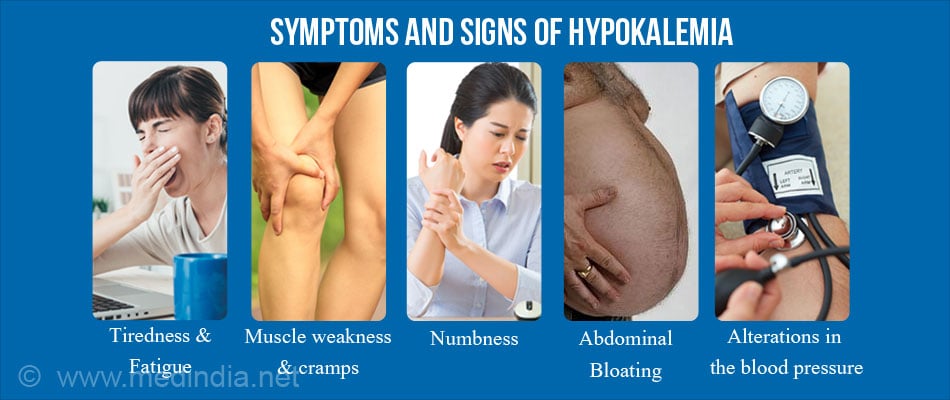
What are the Symptoms and Signs of Hypokalemia?
As potassium is critical to muscle and nerve function, the prominent signs and symptoms of hypokalemia reflect nerve and muscle (which includes voluntary or skeletal muscle, smooth or involuntary muscle in the digestive tract and, most importantly, the heart muscle) dysfunction. These include
- Generalized tiredness and fatigue
- Muscle weakness and cramps
- Diminished tendon reflexes
- Numbness
- Burning or pricking sensations over the extremities (paresthesias)
- Constipation due to decreased bowel muscle movement
- Abdominal bloating
- Alterations in the blood pressure
- Disordered rhythm of the heart (arrhythmia) and ECG changes
- Confusion
- Impaired ability of the kidneys to concentrate urine, leading to passing increased amounts of dilute urine
- Feeling of excessive thirst
How do you Diagnose Hypokalemia?
A history of taking drugs such as diuretics (the most common reason), insulin overdose, or digoxin for congestive heart failure may be obtained from the patient. Hypokalemia may be confirmed by performing the following tests:
Blood Tests:
- Serum potassium levels – Levels below 3.5 mEq/l are diagnostic of hypokalemia
- Serum magnesium levels – Low serum magnesium levels (hypomagnesemia) is a cause of hypokalemia
Urine Tests:
- Urine Potassium levels – In the presence of hypokalemia, urinary levels of potassium give a clue to the possible cause. If the urine potassium levels are less than 20 mEq/l per day, then it is suggestive of an extra-renal cause for the hypokalemia. On the contrary, if the urine potassium levels exceed 20 mEq/l, it indicates a kidney-related cause for the hypokalemia.
- Urine potassium to creatinine ratio – This ratio is also measured to give a clue as to the cause of hypokalemia. A ratio of less than 1.5 mEq/mmol creatinine indicate non-renal causes of potassium loss or intracellular shift of potassium. Higher values are suggestive of loss of potassium through the kidneys.
ECG Changes in Hypokalemia
An ECG should be taken in all cases of suspected hypokalemia or if serum potassium levels are low as heart-related complications can be life-threatening if not treated promptly. A doctor will study the ECG and detect any deviations from the normal.
| Early changes | Decreased amplitude or flattening of T waves |
| Later changes |
|
| Arrhythmias seen in hypokalemia: |
|
Other tests may be conducted depending on the suspected underlying cause.
What are the Serious Complications of Hypokalemia?
- Cardiac arrest
- Heart block
- Electrocardiogram (ECG) changes such a ST segment depression, flat T wave/T wave inversion
- Paralysis of voluntary muscles
- Respiratory failure due to paralysis of muscles of respiration
- Ileus (due to paralysis of smooth muscle of the digestive tract)
- Muscle necrosis (rhabdomyolysis)
- Acute state of confusion and disorientation
How do you Treat Hypokalemia?
The mainstay of treatment is restoration of normal serum potassium levels either by oral or intravenous administration of potassium.
- Oral Potassium – In general, oral potassium supplements given to patients at high risk of developing hypokalemia. High single doses can cause gastrointestinal irritation and bleeding.Therefore oral supplements are given in more than one doses per day. Liquid preparations such as potassium chloride are effective in raising the serum potassium concentrations but are poorly tolerated due to bitter taste. Hence wax coated tablets are preferred. Microencapsulated preparations are also available.
- Intravenous Potassium – In severe hypokalemia or in patients who are unresponsive to oral therapy, it becomes necessary to administer intravenous potassium. As high concentrations can irritate peripheral veins, the potassium should be given in concentrations not exceeding 40 mEq/L.
While giving intravenous potassium, the ECG should be continuously monitored along with regular hourly estimations of serum potassium levels. The potassium should not be added to glucose solutions they can increase the secretion of insulin, which can cause a further worsening of the hypokalemia.
- Magnesium Therapy – When hypomagnesemia is the cause of hypokalemia, concurrent slow intravenous magnesium should be given.
The underlying cause of the hypokalemia should be diagnosed and treated so that it does not recur.
How do you Prevent Hyperkalemia?
To prevent hyperkalemia it is necessary to:
- Patients getting digoxin for congestive heart failure
- Diabetics (as insulin concentrations can fluctuate)
- Persons taking beta-2 agonists such as salbutamol for asthma
- Persons having poor left ventricular function
In patients who require diuretics but are at risk of hypokalemia, spironolactone or triamterene may be given as they do not cause increased potassium excretion. Therefore they are referred to as potassium sparing diuretics.