- Hypoxemia in patients with COPD: cause, effects, and disease progression - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3107696/)
- Right-to-Left Interatrial Shunt with Hypoxemia Caused by a Right Atrial Thrombus - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc1894698/)
- Treatment of hypoxemia in obstructive sleep apnea. - (https://www.ncbi.nlm.nih.gov/pubmed/11732817)
- Application of hyperbaric oxygen therapy in a case of prolonged cerebral hypoxia following rapid decompression. - (https://www.ncbi.nlm.nih.gov/pubmed/971162)
- Lung Function Studies: Methacholine Challenge Test - (https://www.thoracic.org/patients/patient-resources/resources/lung-function-studies-methacholine.pdf)
- Causes of and compensations for hypoxemia and hypercapnia. - (https://www.ncbi.nlm.nih.gov/pubmed/23733653)
What is Hypoxemia?
Hypoxemia refers to the abnormally low blood oxygen levels in the body. In hypoxemia, the arterial oxygen tension (PAO2) is below the normal range (normal values are 80-100 mmHg).
Hypoxemia results in low levels of oxygen in the blood and often leads to hypoxia in tissues as the cells get starved of oxygen.
Difference Between Hypoxemia & Hypoxia
In a broader sense, hypoxia is the failure of oxygenation at tissue level whereas hypoxemia occurs at the blood level and hence the two should not be considered the same.
Significant hypoxia can lead to shortness of breath and is commonly experienced at heights where the oxygen saturation in the atmosphere itself is low.
Hypoxia of the brain is dangerous and if not treated can lead to unconsciousness and even death. Most commonly hypoxemia is due to the diseases of the lungs and as a result of low hemoglobin due to anemia.
Medically hypoxemia is studied by looking at the partial pressure of oxygen (mm Hg) in the arterial blood and the amount of oxygen being carried by the hemoglobin of the red blood cells. The oxygen content of blood is important as this is what determines how much blood reaches the cells rather than the pressure of the oxygen in the arterial blood.
Refractory Hypoxemia - When the oxygen levels become really low and the patient is not responding to oxygen supplementation the condition is referred to as refractory hypoxemia.
What are the Causes of Hypoxemia?
Hypoxemia can develop if there is any factor that influences the rate or volume of air entering the lungs or a factor that affects the exchange of air from the lungs to the blood..
Normally the air we breathe has normal 20.9 percent oxygen. When this concentration is low it can cause hypoxemia naturally. However due to certain conditions like anemia or when your ascend to a high altitude it can result in hypoxia.
1. Ventilation-perfusion mismatch is one of the commonest causes of hypoxemia. The air that reaches the walls of the air sacs (alveoli) is termed ventilation and the blood that reaches the alveoli through the capillaries is termed perfusion. The overall ventilation-prefusion ratio or the V/Q ratio is about 0.8; if the ratio is less than this it results in hypoxemia. This ventilation-perfusion mismatch is the principal contributor of hypoxemia in COPD (Chronic Obstructive Pulmonary Disease) patients, who suffer from progressive lung diseases.
2. Right to left shunting occurs in certain pathological conditions where the blood from the right side of the heart moves straight to the left side, without first passing through the lungs. It is often congenital in origin.
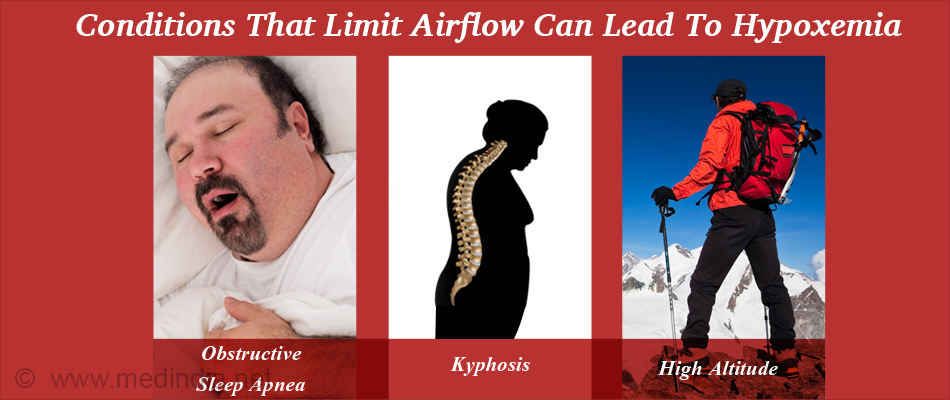
3. Physical states: A variety of physical conditions that physically limit airflow can also lead to hypoxemia.
- Suffocation- Many patients suffering from obstructive sleep apnea have interference in breathing and may have intermittent oxygen desaturation associated with apnea or hypopnea.
- Structural deformities – Conditions such as kyphosis (excessive curvature of the spine in the sagittal plane) and scoliosis (abnormal curvature of the spine in the coronal plane) can restrict breathing and lead to hypoxia.
- Muscle weakness - Limb and ventilatory skeletal muscle dysfunction in COPD patients are often observed and may limit the ability of the diaphragm and cause impairments in gas exchange.
4. Low Environmental Oxygen:
- High Altitude- Decreased external partial pressure of oxygen with altitude can cause hypoxemia.
- Diving- Partial pressures of gases increase during diving and when divers come near surface; this can cause hypoxia.
- Anesthetics- Low partial pressure of oxygen in the lungs occurs when switching from inhaled anesthesia to atmospheric air.
5. Pulmonary disorders that decrease pulmonary ventilation are also causes of hypoxemia.
Emphysema - It is a disease of the lungs that usually develops after many years of smoking. It involves damage to the alveoli of the lung leading to hypoxemia.
Pulmonary embolism- Most patients with severe, acute pulmonary embolism (blood clot) suffer from arterial hypoxemia.
Pneumothorax- It is the abnormal air present in the pleural cavity. It results in lung collapse and compression which ultimately leads to hypoxemia.
Interstitial lung disease- It is a broad category of lung diseases. When responding to any injury, whether from a specific exposure, or unknown causes, the lungs respond to the damage and repair itself. But, if the exposure persists the lungs may be permanently damaged. Hypoxemia is most common in interstitial lung disease.
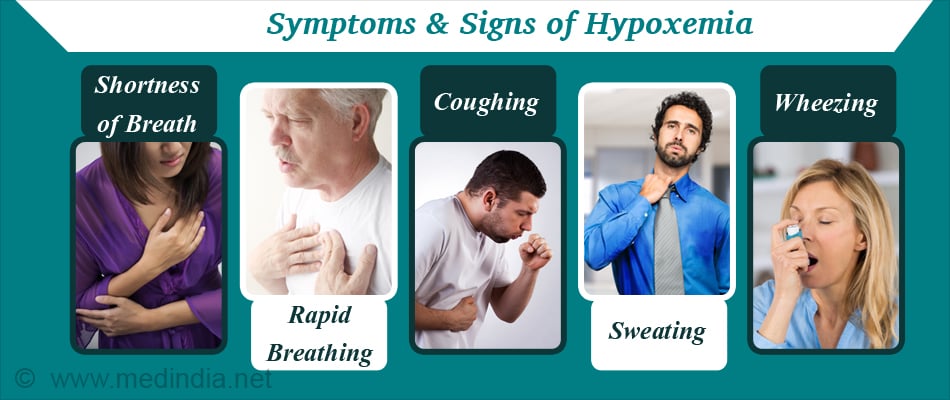
What are the Symptoms and Signs of Hypoxemia?
Symptoms of hypoxemia may be acute or chronic which mainly include:
- Shortness of breath
- Rapid breathing
- Fast heart rate
- Cough
- Sweating
- Wheezing
- Sensation of choking
- Fluid retention at high altitudes
- Changes in the color of skin from blue to cherry red
Severe symptoms seen with cerebral hypoxia may include:
- Confusion
- Inability to communicate
- Coma
How do you Diagnose Hypoxemia?
Hypoxemia is diagnosed by measuring the oxygen level in a blood sample taken from an artery.
- Pulse oximeter is used to measure the oxyhemoglobin saturation of blood (oxygen monitors are placed on fingers or ears). Normal arterial oxygen is approximately 75 to 100 millimeters of mercury (mm Hg). Values below 60 mm Hg indicate that there is a need for supplemental oxygen. Normal pulse oximeter readings usually range from 95-100 % and readings below 90 % are considered low.
- Carbon monoxide detectors are used along with pulse oximeters to eliminate false readings which occurs when carbon monoxide has entered the body.
- Pulmonary function tests - It is a valuable tool for the complete evaluation of the respiratory system. It can help determine the cause of low oxygen saturation.
- Modified apnea testing- Apnea testing can also be used in patients with severe hypoxemia.
- Methacholine challenge test- It is also a type of lung function test; during the test, the patient is made to inhale small dose of methacholine. The breathing test is performed before and after each dose of methacholine.
How do you Treat Hypoxemia?
If the patients feel shortness of breath or any of the general symptoms of hypoxemia, an inhaler or an asthma medicine could help them relieve hypoxemia and ease breathing.
Severe or emergency cases of hypoxemia require the attention of critical care professionals. In such cases, the treatment for hypoxemia may include mechanical ventilation and supplemental oxygen therapy.

A simple disposable plastic mask for controlled low-oxygen levels can also be used. This delivers an inspired oxygen concentration of about 24% with an oxygen flow rate of 1.5 to 2 liter/min; the re-breathing of carbon dioxide under the mask is negligible. This mask is a well-tolerated method for short or long-term low oxygen therapy in patients with hypoxemia that occurs due to varying causes.
Nasal cannula can also be used. It delivers oxygen at a flow rate of 1 to 6 litres per minute (l/min), at concentrations of 24 to 44%.
Hyperbaric oxygen therapy in case of prolonged cerebral hypoxia is also recommended. It mainly works by enhancing the amount of dissolved oxygen in the plasma and thereby increasing O2 delivery to the body tissues.
Corticosteroids- Acute respiratory distress syndrome (ARDS) is an acute hypoxemic state; inflammation is the key factor in the pathophysiology of ARDS. Corticosteroids are potent anti-inflammatory, antifibrotic, and immunomodulator agents which exert their inhibitory effects on the inflammation. Methylprednisolone is an effective steroid used in the treatment of hypoxemia.
Surgical or Continuous Positive Airway Pressure (CPAP) therapy- Hypoxemia complicates the recovery of 30% to 50% of patients after abdominal surgery. CPAP therapy is a better alternative to treat this condition than mechanical ventilation or endtracheal intubation.
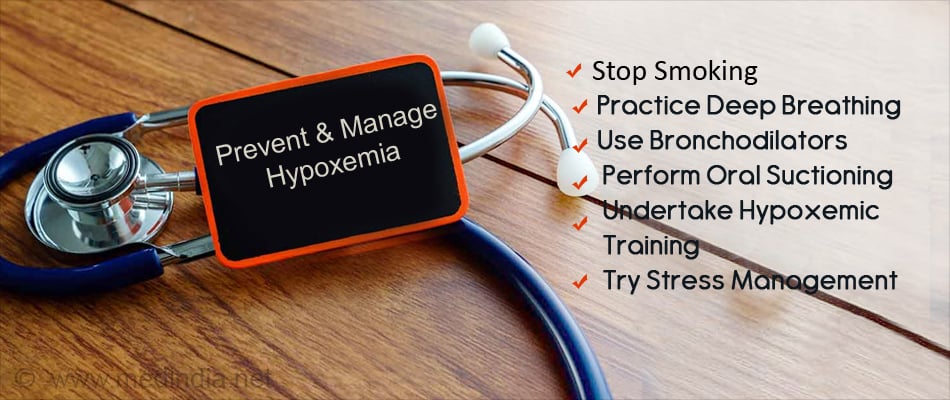
How do you Prevent & Manage Hypoxemia?
- Stop smoking- Smoking can trigger the asthma symptoms leading to hypoxemia.
- Deep breathing and coughing techniques- These techniques help patients effectively clear their airway while maintaining their oxygen levels.
- Use of Bronchodilators- Medications such as bronchodilators effectively relax smooth muscles and open airways in certain disease processes such as COPD.
- Oral suctioning- Patients with muscle disorders or those who have suffered a cerebral vascular accident (CVA) may have ineffective cough reflexes, which could lead to hypoxia. Oral suctioning given to these patients may help to prevent this condition.
- Hypoxic training- Hypoxic training should be given to maintain good health.
- Take medicines and use the rescue inhaler when needed to help prevent flares.
- Stress can trigger many respiratory disorders leading to hypoxemia and should be avoided.