- Koning S, van der Sande R, Verhagen AP, van Suijlekom-Smit LWA, Morris AD, Butler CC, Berger M, van der Wouden JC. Interventions for impetigo. Cochrane Database of Systematic Reviews 2012, Issue 1. Art. No.: CD003261.
- Diagnosis and Treatment of Impetigo - (http://www.aafp.org/afp/2007/0315/p859.html)
- Impetigo - (http://kidshealth.org/en/parents/impetigo.html)
- Impetigo Infection - (https://en.wikipedia.org/wiki/impetigo)
- Impetigo: Diagnosis and Treatment - (http://www.aafp.org/afp/2014/0815/p229.html)
- Overview - Impetigo - (http://www.mayoclinic.org/diseases-conditions/impetigo/home/ovc-20202557)
- What is impetigo? - (http://www.dermnetnz.org/topics/impetigo/)
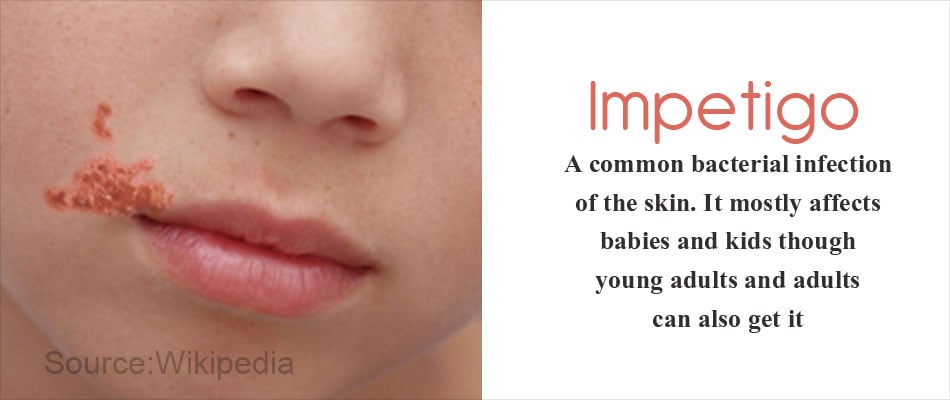
What is Impetigo?
Impetigo is a common bacterial infection of the skin. It mostly affects babies and kids though young adults and adults can also get it.
It is highly contagious and causes pus-filled bumps (pustules) and blisters on the face, neck area, hands, feet and the diaper area. Red sores usually appear near the mouth area on the face. They can be itchy, painful and irritating. It is important not to touch these sores with bare hands as it can cause further infection and spread rapidly.
What are the Causes and Risk Factors of Impetigo?
The pathogens mainly involved in causing impetigo are:
- Staphylococcus aureus - This is the most common one and causes both the bullous and non-bullous types
- Streptococcus pyogenes - This causes mainly non-bullous impetigo
- Methicillin-resistant Staphylococcus aureus (MRSA) - Impetigo is becoming resistant to a lot of antibiotics and hence this new class of bacteria is also another cause.
People who are at risk of getting impetigo are:
- Children - They quickly catch these infections when they are in contact with other children who might have had it. Touching infected toys and other infected objects can lead to spreading the infection. Children in the age group 2-5 are most prone to this infection. Impetigo spreads very fast in crowded places like childcare centers and schools.
- Adults with compromised immunity - Those with diabetes and other preexisting conditions are at risk. Secondary impetigo is also possible in people who have had scabies or eczema.
- People who live in warm climates - Impetigo bacteria thrive well usually during the summer season.
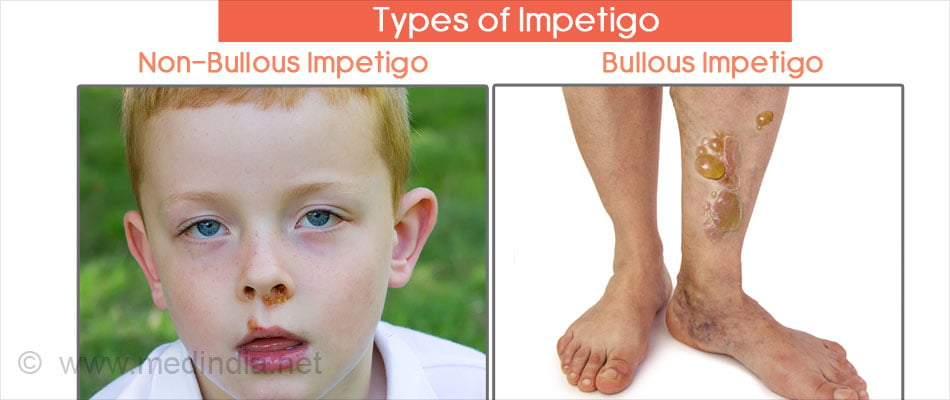
What are the Types and Symptoms of Impetigo?
There are two types of impetigo conditions both with different symptoms.
Non-Bullous Impetigo:
The symptoms of non-bullous impetigo begin with red sores usually around the mouth, face and neck area. The limbs can also be affected. These sores quickly burst and leave behind a thick crust. The crust dries and leaves a reddish mark. The redness usually disappears after a few weeks.
These sores can be itchy and it is important to prevent children from scratching and causing further ulceration. Sometimes the sores are accompanied by high fever.
Bullous Impetigo:
Bullous impetigo begins with fluid-filled blisters on the waist, neck, arms and legs. The blisters quickly spread across the body. These blisters break within a few days and leave behind a yellow crust. The blister area is usually painful and it is important not to touch the blisters. High fever is common in this type of impetigo.
What are Some of the Rare Complications of Impetigo?
Impetigo rarely causes complications but certain symptoms should not be ignored. Get to your doctor immediately if you have the following conditions:
- Cellulitis – An infection of the deeper layers of the skin and tissue.
- Psoriasis – Causes serious itching and burning of the skin along with flaking off of layers.
- Septicemia – A serious bacterial infection of the blood. This is a medical emergency and the child or adult should be treated in the hospital.
- Glomerulonephritis – A condition caused by post-infection due to streptococcal bacteria. This is an inflammation of the small blood vessels in the kidney and needs immediate treatment.
What is the Diagnosis for Impetigo?
Doctors usually diagnose impetigo clinically that show up as honey-colored scabs. Follow-up with bacterial swabs (swab of the liquid produced by the sores) can be taken for microscopy, culture and sensitivity. A complete blood count can indicate a high count of white blood cells that fight infection when impetigo is present.
It is important to get the microscopy tests done so that the right antibiotic can be worked out in the treatment plan. Depending on the type of bacteria seen, the doctor will customize the antibiotic plan.

What is the Treatment for Impetigo?
Depending on the severity of the infection, the doctor will recommend suitable creams or oral antibiotics.
- The most frequently used antibiotic cream for mild cases is mupirocin which is usually applied on the sores at least 3-5 times a day. The sores must first be cleaned with sterile cotton gauze soaked in disinfectant solution before applying the cream.
- For severe cases, oral antibiotics are given. Penicillin and amoxicillin were less effective. Dicloxacillin, flucloxacillin, cloxacillin, erythromycin or amoxicillin/clavulanate (Augmentin) can be used. For people who are allergic to penicillin or infections with MRSA they can use doxycycline or clindamycin. In some cases, oral antibiotics induce side effects like nausea and diarrhea. These usually go away after the course is complete.
How do you Prevent the Recurrence and Spread of Impetigo?
Since impetigo is highly contagious, it is important to prevent the recurrence and spread of the infection to others.
Recurrence of the infection can be prevented by treating carrier sites with antibiotic creams. Apply the cream to previously affected areas like nostrils. Use a good antibacterial hand wash as well as bath soap to keep yourself clean.
Prevent the spread of infection to others by keeping infected children at a distance. Do not send the children to school if they are infected. They must stay home until the crusts dry. Separate towels must be used. Sharing of towels is strictly forbidden. A change of clothes is recommended everyday along with a bath.







