- Functional gastrointestinal disorders among people with sleep disturbances: a population-based study. - (https://www.ncbi.nlm.nih.gov/pubmed/15595333)
- Noninvasive methods in evaluation of inflammatory bowel disease: where do we stand now? An update - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2827710/)
- Diagnosis and Treatment of Gastrointestinal Disorders in Patients With Primary Immunodeficiency - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3800204/)
- Diet and Inflammatory Bowel Disease: Review of Patient-Targeted Recommendations - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4021001/)
- THE FACTS ABOUT Inflammatory Bowel Diseases - (http://www.ccfa.org/assets/pdfs/updatedibdfactbook.pdf)
- Environmental Risk Factors for Inflammatory Bowel Disease - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2886488/)
- Severe complications of inflammatory bowel disease - (https://www.ncbi.nlm.nih.gov/pubmed/18387381)
What is Inflammatory Bowel Disease?
Inflammatory bowel disease (IBD) is defined as a group of autoimmune diseases that are characterized by chronic intestinal inflammation or bowel obstruction resulting from host-microbial interactions or environmental factors.
The two major diseases of this inflammatory condition are ulcerative colitis (UC) and Crohn's disease (CD).
What are the Causes of Inflammatory Bowel Disease?
The exact cause of IBD is unknown but diet, sleep, environmental factors, and immunoregulatory factors have been associated with IBD.
- Immune system malfunction - One possible cause of IBD is an immune system dysfunction. Gastrointestinal (GI) disorders are reported to be present in 5-50% of patients with primary immunodeficiencies. Dysfunction of the regulatory mechanisms (T-cells) maintaining the balance between active immunity and tolerance in the gut may lead to mucosal inflammation.
- Heredity - An individual is more likely to develop IBD if he has family members with the disease.
- Environmental factors - Factors like hygiene, smoking, oral contraceptives and breastfeeding have been reported to the probable causes of IBD.
- Sleep - Studies show that IBS is prevalent in those with self-reported sleep disturbance. Sleep deprivation can lead to increased levels of inflammatory cytokines, tumor necrosis factor-á and C-reactive protein, leading to further activation of the inflammatory response.
- Diet - Although there are not much studies reported for the influence of diet on IBD but in some cases dietary fiber intake has been associated with a lower risk of developing Crohn’s disease (CD). Also, patients who had a high intake of meat, eggs, protein and alcohol were more likely to have a relapse of Ulcerative Colitis (UC).
What are the Risk Factors of Inflammatory Bowel Disease?
The risk factors or environmental triggers for IBD are as follows:
Age - Although Crohn’s disease and ulcerative colitis can occur at any age but, people are more frequently diagnosed between the ages of 15 and 35.
Smoking - According to a study,active smokers are more than twice as likely as non-smokers to develop Crohn’s disease. In a meta-analysis, a paradoxical relationship has been demonstrated between smoking and IBD. Individuals who smoke actively were less likely to develop UC compared to individuals who were never smokers or ex-smokers.
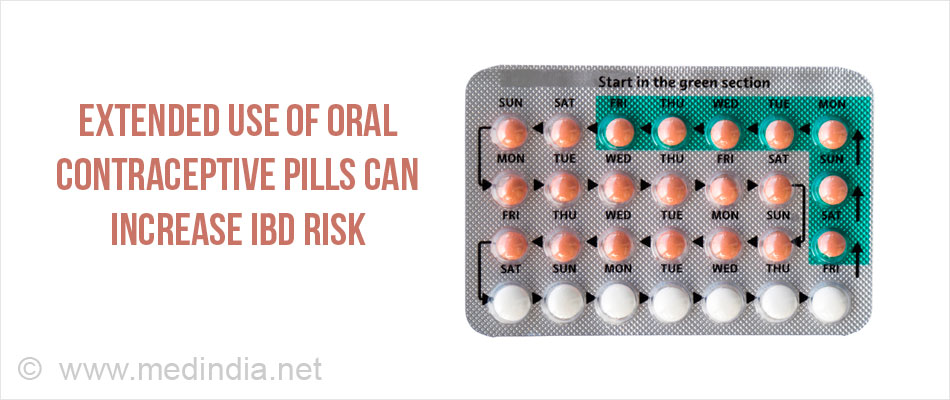
Oral Contraceptive Pills (OCPs) - The risk of CD is increased with the prolonged use of OCPs.
Non-Steroidal Anti-inflammatory Drugs - NSAIDs may cause damage to the intestinal mucosa of the stomach, small bowel, and colon. They also increase intestinal permeability by inhibiting cyclooxygenase, thus, prostaglandin production. Inhibition of prostaglandins has been implicated in IBD due to immunoregulatory effects.
Appendicitis - Children undergoing an appendectomy before 10 years of age are less likely to develop ulcerative colitis later in life, but are at a higher risk of developing Crohn’s disease.
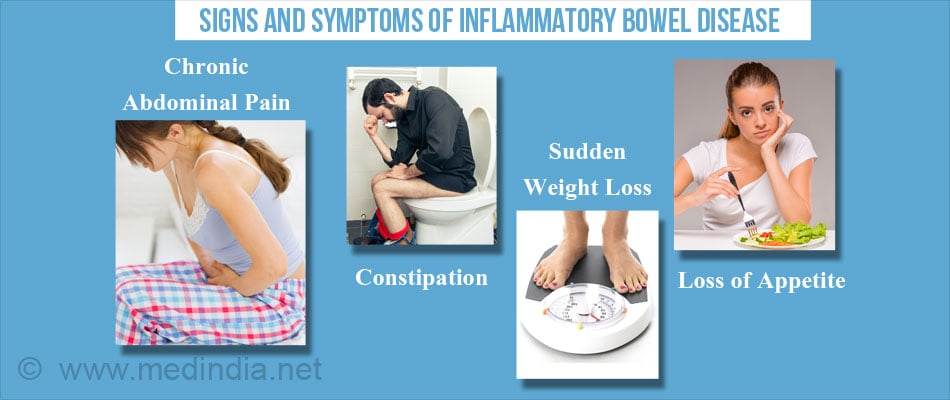
What are the Signs and Symptoms of Inflammatory Bowel Disease?
With IBD, inflamed bowel including redness and swelling are the most common symptoms. Both Ulcerative Colitis and Crohn’s disease almost have common symptoms. Related symptoms, which can range from mild or severe, include:
- Severe or chronic abdominal pain
- Diarrhea
- Rectal bleeding
- Constipation
- Sudden weight loss
- Loss of appetite
- Rectal bleeding
Other symptoms unrelated to the gastrointestinal tract may include:
- Fever
- Skin rashes
- Night sweats
- Mouth sores
- Joint pain
- Weight loss
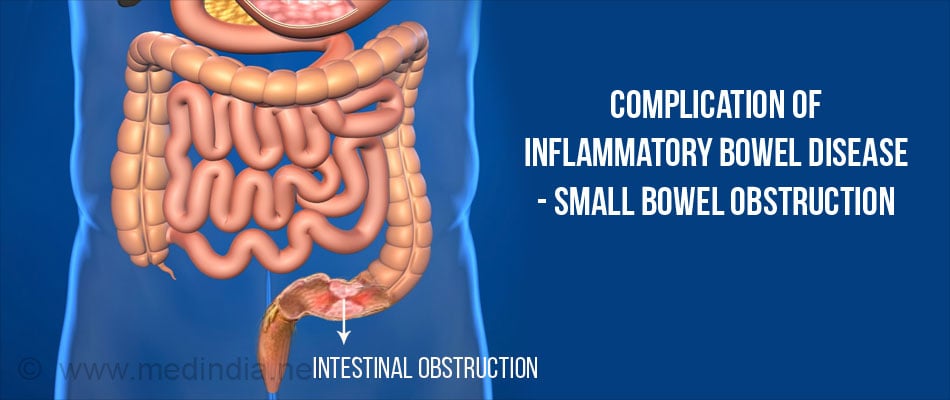
What are the Complications of Inflammatory Bowel Disease?
Patients who have inflammatory bowel disease may occasionally develop severe complications or emergency situations that require extra medical care which include:
- Anemia due to blood loss
- Ischemic colitis Blood flow to part of the large intestine is reduced
- Fistula formation occurs when the inflammation extends through the bowel wall and forms an abnormal tract between the intestines and skin or other organs
- Abdominal abscesses – Abscesses may occur when a fistula becomes infected
- Small bowel obstruction – Inflammation and scarring of the intestine leads to narrowing of bowel lumen and obstruction.
- Malignancy – Risk of colonic malignancy is increased in inflammatory bowel disease. Persons suffering from IBD should undergo regular Colonoscopy.
- Malnutrition – Diarrhea and abdominal pain make it difficult to follow a regular and well-balanced diet, leading to malnutrition
- Primary sclerosing cholangitis (biliary tract inflammation) and uveitis (inflammation of iris and ciliary bodyin the eyes) are some of the extraintestinal complications of IBD.
How do you Diagnose Inflammatory Bowel Disease?
The following tests and procedures are adopted to help confirm a diagnosis of IBD, they are as follows:
Blood Tests
Various laboratoryblood tests including hemoglobin, platelet count, Erythrocyte sedimentation rate (ESR), albumin and C reactive protein (CRP) are used as preliminary screening tests for IBD.
Screening for Anemia
Blood loss from chronically inflamed intestinal mucosa and micronutrient deficiency are the main mechanisms for the development of anemia in patients with IBD. So, screening of anemia is also regularly done.
Fecal Markers
The fecal excretion of Indium 111-labeled leukocytes is considered to be the standard fecal marker of inflammation, and shows a sensitivity of 97% for the diagnosis of IBD. Fecal levels of Alpha1 1-antitrypsin, which is a protease inhibitor is also a useful indicator of IBD specifically CD activity.
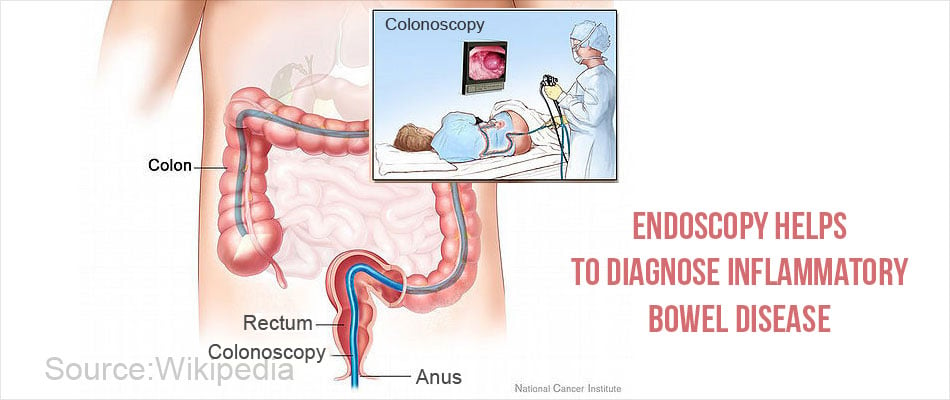
Endoscopy
Different types of endoscopy are used based on the part of GI tract examined.
Sigmoidoscopy examines the lining of the lower part of the large intestine (the rectum and sigmoid colon).
Colonoscopy examines the lining of the entire large intestine (i.e. colon) and some part of small intestine (ileum). This exam can help determine the severity of ulcerative colitis and Crohn’s disease as well as colon cancer.
EGD (Esophagogastroduodenoscopy) – this technique involves examining the lining of the esophagus, stomach, and duodenum.
ERCP (Endoscopic retrograde cholangiopancreatography) examines the bile ducts in the liver and the pancreatic duct.
Leukocyte Scintigraphy
White blood cells get attracted to sites of bowel inflammation. In this test, blood is taken from the arm, and white blood cells in the sample are tagged with a specified amount of a radioactive substance. The blood is injected back into the patient’s body and a special camera is used to see where the radioactive white blood cells travel.
Imaging Technique
It is an alternative to endoscopy a barium follow-through procedure is a useful medical imaging technique for Crohn’s disease when only the small intestine is affected. In this technique, the patient is made to drink a solution containing barium sulfate that appears white on X-ray and highlights the internal lining of the bowel.
Other imaging techniques include computerized tomography (CT) scan and magnetic resonance imaging (MRI) scan to provide detailed images of the small bowel and colon.
How do you Treat Inflammatory Bowel Disease?
There is no known medical or surgical cure for IBD but following drugs are being used in the treatment of IBD for alleviation of symptoms. The chief goal of treatment is reduction of the inflammation that is responsible for the symptoms of IBD.
1. Medical Treatment
Anti-inflammatory drugs- Certain 5-aminosalicylates — including mesalamine balsalazide and olsalazine are available in both oral and enema or suppository forms, which are used for the treatment. They work by the production of anti-inflammatory cytokines that inhibit the production of proinflammatory cytokines.
Immunomodulators
Immunomodulators, such as azathioprine, cyclosporine, mercaptopurine, methotrexate, infliximab, adalimumab, certolizumab, and natalizumab are used. These compounds regulate the immune system by efficiently triggering a Th2-mediated response that hinders Th1-mediated inflammation.
Corticosteroids
Steroids such as hydrocortisone and prednisolone are given in moderate to severe cases of ulcerative colitis or Crohn’s disease that have not responded to other drugs. Due to their numerous side effects, they are not given long-term.
Antibiotics
Antibiotics like metronidazole and Ciprofloxacin help control the infection and heal fistulas in case of CD and UC.
Anti-diarrheal agents
Fiber supplements such as methylcellulose and psyllium increase stool bulk and help to relieve symptoms of mild diarrhea. In severe diarrhea, drugs such as loperamide are administered.
Iron and vitamin supplements
Since most persons with IBD also have iron deficiency and vitamin B12 deficiency, iron supplements and B12 injections have to be taken.
Drug-loaded microcapsules
Artificial cell microencapsulation technique allows the delivery of pharmaceutical compounds to specific tissues in the body in a time-dependent manner. Studies have shown that artificial cell microencapsulation of thalidomide is a potential tool in the remission of Crohn’s disease.
2. Surgical Treatment
If the patient fails to respond to diet changes and medical treatment, surgery may become necessary.
Surgery involves removing damaged portions of the small intestine or colon and anastomosing the cut ends (eg ileoanal anastomosis). Occasionally, when this is not possible, a permanent opening is created on the abdominal wall (ileal stoma) and the stool is collected into a bag for disposal. Other operations include closure of fistulas and drainage of abscesses. Widening of narrowed portions of the intestine (stricturoplasty) is also done in certain cases.
How do you Prevent Inflammatory Bowel Disease?
- Maintain a well-balanced diet in order to prevent nutritional deficiencies occurring particularly in patients with Crohn’s disease.
- Smoking has a negative effect on patients with Crohn’s disease, and quitting smoking might alleviate symptoms.

- Preliminary studies demonstrate that moderate exercise can help prevent IBD. Physical activity improves quality of life which gets affected during IBD.
- Restrict foods high in fiber as these can aggravate symptoms.
- Avoid foods that can cause bloating such as beans, cabbage, broccoli, caffeine, and carbonated drinks.
Health Tips
- Limit dairy products
- Drink plenty of fluids
- Eat small quantities but frequently