Q: Which specialist should I consult for symptoms of myoclonic epilepsy?
A: You should consult a neurologist.
Q: Is there a cure for myoclonic epilepsy?
A: Yes, juvenile myoclonic epilepsy (JME) can be treated with medications. With the appropriate drugs, the condition can be managed and may, in some cases, go into remission. However, medications have to be continued for life. Drug-resistant JME is hard to treat. Failure to change lifestyle can also be a deterrent to managing the condition.
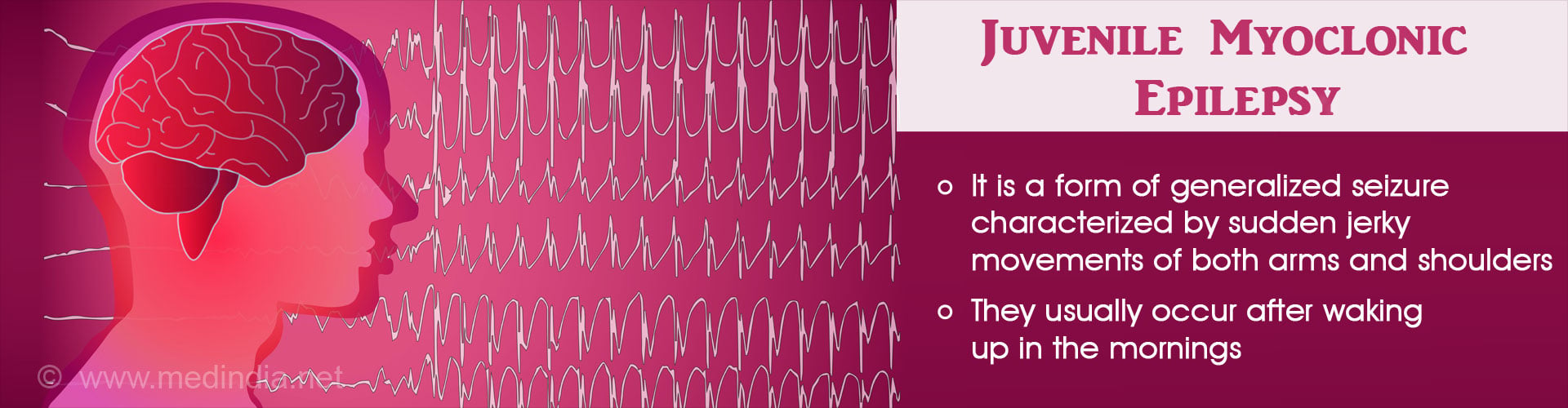
Q: What is the other name for juvenile myoclonic epilepsy (JME)?
A: The alternate name for JME is Janz syndrome.
Q: Can juvenile myoclonic epilepsy be inherited?
A: Juvenile myoclonic epilepsy is a genetic condition and it can be inherited. It is observed in first-degree relatives of the patient.
Q: Is epilepsy contagious?
A: No, epilepsy is not a contagious disease.
Q: Is juvenile myoclonic epilepsy (JME) fatal?
A: Patients with JME are at risk of sudden death, known as sudden unexpected death due to epilepsy (SUDEP). Failure to take medications, mental handicaps, neurological dysfunction, GTCS increase the risk of SUDEP.
Q: What occurs if juvenile myoclonic epilepsy is treated inappropriately?
A: When JME is treated inappropriately with antiepileptic drugs, a condition named myoclonus status epilepticus occurs.
Q: What are the possible conditions that can aggravate seizures in juvenile myoclonic epilepsy (JME)?
A: Obstructive sleep apnea, hyperthyroidism, and psychiatric disorders can aggravate seizures in JME. Drugs, such as phenytoin, carbamazepine, and oxcarbazepine can aggravate seizures and should not be used to treat JME.