- What is Merkel Cell Carcinoma? - (http://www.skincancer.org/skin-cancer-information/merkel)
- Welcome! Defeating Merkel cell carcinoma begins here. - (https://www.merkelcell.org)
- Merkel Cell Carcinoma Treatment (PDQ�)�Health Professional Version - (https://www.cancer.gov/types/skin/hp/merkel-cell-treatment-pdq)
- Merkel Cell Skin Cancer - (https://www.cancer.org/cancer/merkel-cell-skin-cancer.html)
- Lebbe C, Becker J et al. Diagnosis and treatment of Merkel Cell Carcinoma. European consensus-based interdisciplinary guideline. European Journal of Cancer, 2015.
- Hughes MP, Hardee ME et al. Merkel Cell Carcinoma: Epidemiology, Target, and Therapy. Current Dermatology Reports. 2014; 3(1): 46–53.
What is Merkel Cell Carcinoma?
Merkel cell carcinoma (MCC) is a rare and a highly aggressive type of primary skin cancer. Carcinoma denotes cancer of the skin or the lining of the internal organs. Cancer occurs when body's cells multiply without control. Merkel cell carcinoma was first described by Cyril Toker in 1972 who named it 'trabecular cancer'.
The skin is made up of 3 layers, the epidermis, dermis and the hypodermis (subcutaneous fat layer) followed by the muscle layer. The Merkel cells are found at the interface between the epidermis and the dermis and are connected to the nerve endings responsible for the touch sensation. They also produce hormones. As they have the properties of both nervous and endocrine cells, they are called neuroendocrine cells. They were first discovered by the German histopathologist Freidrich Sigmund Merkel in 1875.
The incidence of MCC is increasing all over the world by around 8% every year. MCC usually appears in sun-damaged areas of skin of the head and neck region (53%), followed by upper and lower limbs (35%); the rest are found on the truck, mouth and genital lining. It is commonly seen in elderly males. MCC can recur even after treatment.
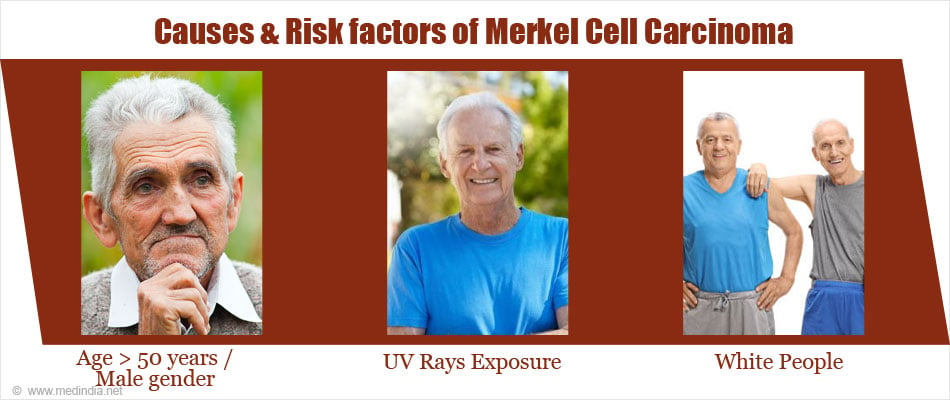
What are the Causes / Risk factors of Merkel Cell Carcinoma?
The cause of MCC is still unknown, though long-term sun exposure and infection with Merkel cell polyomavirus (MCV) has been suggested. Factors that increase the risk of Merkel cell carcinoma are:
- Age > 50 years, majority of the patients are over 70 years of age
- Male gender
- UV rays exposure - exposure to excessive and prolonged sunlight and to tanning beds
- Light skin colour ¨C the cancer is more common in white people
- Low immunity states ¨Ce.g. patients who have undergone organ transplant or suffer from AIDS or chronic lymphocytic leukaemia
- Psoriatic patients treated with ultraviolet A (PUVA) or psoralen
MCC spreads quite quickly both locally and to distant areas of the body. At the time of the diagnosis, about 66% have local cancer, 27% have lymph node involvement and 7% have metastatic disease. The 5-year survival rate, according to SEER data, is 64% for local cancer, 39% for lymph node disease and 18% for metastatic spread. Hence, early diagnosis and treatment are crucial.
What are the Symptoms and Signs of Merkel Cell Carcinoma?
MCC usually starts as firm painless skin lesions or nodules, especially on sun-exposed parts of the body. They are commonly seen on the head and neck regions; followed by the upper limbs, lower limbs and the truck.
The nodules are of varying sizes (few millimetres to 2 cm, the average lesion being 1.5 cm) and appear in different colours-red, pink, purple, blue or skin coloured. They are painless, and rarely can break open to forms ulcers.
As the cancer cells spread through the lymphatics in the dermis, satellite lesions can be seen. These are skin or subcutaneous lesions within 2 cm of the primary tumour. Regional lymph node enlargement is seen about 30-40% patients.
How is Merkel Cell Carcinoma Diagnosed?
Biopsy of the lesion: Once the lesion is found to be suspicious of cancer, it must be confirmed with a biopsy. An incisional biopsy (where a piece of the cancer is obtained) or an excisional biopsy (where the entire tumor is excised) should be done. A pathologist studies the specimen under a microscope (histopathology study) and confirms the diagnosis.
If there is any doubt (as the histopathology of MCC, Ewing's sarcoma, small cell lung cancer, neuroblastoma and medulloblastoma all look similar), special stains called immunohistochemical stains can be used which help in confirming the diagnosis.

Sentinel lymph node biopsy (SLNB): Sentinel lymph node is a single/group of nodes where the cancer cells are more likely to spread first from the primary tumor. This helps in accurate staging of the cancer and subsequent treatment. If SLNB is negative for the cancer, the patient has a better prognosis.
Imaging:
- Ultrasound of regional lymph nodes is done to identify nodal spread.
- Chest X-ray helps to distinguish between Merkel cell cancer that has spread to the lungs as opposed to oat cell carcinoma that arises in the lung.
- CT scan of the chest, abdomen and pelvis need to be done to identify any spread to distant parts.
- 2-fluoro-2-deoxygucose (FDG) positron emission tomography (FDG-PET scan) may help in staging and follow up of MCC. FDG-PET scans have been found to be superior to CT scans in identifying metastatic disease even in subcentimeter nodes. Similarly, post treatment, FDG-PET scans can show treatment response based on the level of FDG uptake.
Test for Merkel Virus: Test for CM2B4 antibody can be used to detect the presence of Merkel cell polyomavirus. However, the presence of the virus does not mean that a person will suffer from the cancer. Likewise, a person who suffers from Merkel cell cancer may not harbor the virus.
Blood tests: A complete blood picture, ESR, kidney function tests like serum urea, creatinine and electrolytes, and liver function tests should be done to check if organs like the liver or the kidneys are affected.
What is meant by Merkel Cell Carcinoma Staging?
Staging is the process that helps to decide on the best treatment and the possible outcomes of a cancer. Stage 1 has best survival rate whereas Stage-4 is potentially fatal.
Staging for MCC is based on the size and the spread of the cancer. MCC can locally infiltrate the underlying tissues like the subcutaneous fat, muscle and connective tissue layers (local spread). MCC can also spread through blood vessels or lymphatics to regional lymph nodes (nodal spread) or to distant organs like lung, liver and brain (metastatic spread). MCC can be classified into the following stages:
Stage 1: The MCC is localized to the skin, the tumor diameter ¡Ü 2 cm, no lymph node involvement is noted, or a lymph node biopsy is not done.
Stage 2: The MCC is localized to the skin, the tumor diameter is > 2 cm and may spread to neighboring tissue but no lymph node involvement is present.
Stage 3: The cancer has spread or is in the process of spreading to regional lymph nodes (in transit metastasis).
Stage 4: The cancer has spread to distant parts of the body or to the internal organs.
Recurrent: This indicates that the cancer has come back after it was treated. It may come back in the previous area or in a different part of the body.
How is Merkel Cell Carcinoma Treated?
Treatment is based on the stage of the cancer.
Surgical treatment: Surgery is the treatment of choice for majority of patients who have operable cancer. Surgery is of several types - excisional surgery, Mohs micrographic surgery and cryosurgery.
- Excisional surgery: Wide local excision with 2-3 cm margin is the treatment of choice for Stage 1 and 2 MCC. Here along with the tumor, 2-3 cm of normal skin is also removed, except in the head and neck regions, where narrow margins are also acceptable.
- Cryosurgery: Extremely cold temperatures produced by liquid nitrogen kill the cancer cells by freezing them.
- Mohs micrographic surgery: This can be offered to patients who have MCC on the face (where wide excision may not be possible) and who already had a sentinel node biopsy done. This procedure involves removing one layer at a time and studying the specimen under the microscope during surgery itself, to make sure that all the cancerous cells are removed.
- Lymph node dissection: If sentinel lymph node biopsy is positive, all affected lymph nodes are removed. SLNB is usually recommended in Stage 1 and 2 due to MCC's potential to metastasize.
Radiotherapy: Standard postoperative treatment (following all types of surgery and lymph node dissection) consists of radiotherapy given over 5-6 week period. Penetrating beams of energy waves are delivered to the cancer cells and the surrounding normal skin margin; this helps destroys the cancer cells that may remain after surgery.

Radiotherapy can be used alone (without prior surgery) if the tumor is inoperable or if the patient refuses surgery. It can also be given to the sentinel lymph nodes as an alternative to lymph node dissection.
Radiotherapy markedly lowers the risk of MCC recurrence at the primary site and regional lymph nodes. It also helps to shrink the tumor and relieve symptoms of distant metastatic disease.
Chemotherapy: Anti-cancer drugs are given orally or injected through a vein; the drug then travels to all the parts of the body. This is usually given to patients who have not responded to radiotherapy or other treatments and also to patients with widespread disease.
Commonly used drugs include Doxorubicin, Cyclophosphamide, Cisplatin, Carboplatin, Topetecan and Etoposide. Treatment is given few times a week and the duration depends on the response and the tolerability of the patient.
Immunotherapy: Here medicines that help the body's own immune system to fight against the cancer cells are used. This is usually given for MCC that has metastasized. Immune Checkpoint Inhibitors (ICI) is the class of drugs that are used here. Examples include Avelumab and Pembrolizumab, which is used off-label.
How can Merkel Cell Carcinoma be Prevented?
- Do not expose yourself to sunlight from 10 am to 4 pm; this is when the sun rays are strong. Avoid sunbathing.
- Cover yourself up with adequate clothes (full sleeve shirts or trousers), a wide brim hat, and an umbrella when outdoors especially in summer.
- Use UV blocking sun glasses.
- Avoid getting tanned, and never use tanning beds.
- Use broad spectrum sunblock creams/lotions (UVA/UVB) on the exposed parts of the body and face. The sunblock cream should have an SPF of at least 15 or higher for daily use. For prolonged periods in the sun, the SPF should be more than 30 or higher.
- Apply about 1 tablespoon of the sunblock cream at least 30 minutes before stepping out in the sun, and reapply once every 2 hours. Reapply immediately after swimming or if there is excessive sweating. Children younger than 6 months should not use the sunscreen cream.

Health tips
- Everyone should watch out for skin changes; it is better to get any new skin lesion examined by your doctor.
- If you see a mole or a lump that is changing in size, shape, color, appearance, and is growing rapidly or starts bleeding with minor trauma like scratching, washing the face or shaving. then see your doctor rightaway.
- Improve immunity by adopting a healthy lifestyle.
- See a doctor at least once a year for a professional skin check-up.