- Mucolipidoses - (http://www.malacards.org/card/mucolipidoses)
- Mucopolysaccharidoses and mucolipidoses - ( https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1347205/)
What are Mucolipidoses?
Mucolipidoses (ML) are a group of inherited metabolic disorders which result in the accumulation of complex carbohydrates and lipids in the lysosomes within the cells. It is classified as a lysosomal storage disorder.
Lysosomes are cell organelles located within human cells. These structures process substances like carbohydrates and lipids and break them down into smaller molecules with the help of enzymes.
People with ML either lack the required enzyme or produce insufficient or abnormal/ineffective enzyme. In the absence of adequate/functioning enzymes, the lysosomes cannot break down carbohydrates or lipids. These substances accumulate in the cells of tissues in the body and lead to tissue and organ damage.
What are the Types of Mucolipidosis?
ML are classified into four types based on the enzyme which is missing/non-functional/mutated.
The four types are sialidosis (ML I) and types II, III and IV:
- Sialdosis or ML Type I – is a result in the deficiency of the enzyme sialidase. Sialidase is required to remove a form of sialic acid from sugar-protein complexes known as glycoproteins. The deficiency causes sugar-like substance accumulating in the bone marrow, neurons and other cells in the body. Infants with sialdosis present with facial features like a flat nasal bridge, puffy eyelids and abnormal tongue size, often with skeletal malformations like hip dislocations. Other symptoms include ataxia (lack of coordinated muscle movement), tremors, vision disturbances, seizures, enlarged liver and spleen, lack of muscle tone and mental retardation. Babies/children with ML pick up recurrent respiratory infections.
- ML Type II and III – are caused by a deficiency of the enzyme N-acetylglucosamine-1-phosphotransferase. ML II is often referred to as inclusion-cell (I-cell) diseases because microscopic examination indicates the presence of masses known as inclusion bodies. These inclusion bodies contain substances like carbohydrates, proteins and lipids which are not broken down. ML II is a severe form of ML and is often seen at birth in infants. Children often present with organ enlargement like heart valves, liver and spleen enlargement. There is a marked delay in gross and fine motor skills, as well as other development delays. Complications of ML II include clouding of the cornea, acute and severe respiratory distress like bronchitis and pneumonia, and congestive heart failure. ML III (Pseudo-Hurler Polydystrophy) is lesser in severity and symptoms are seen in children between the ages 3-5 years. Though ML III is also linked to the enzyme N-acetylglucosamine-1-phosphotransferase, it is less severe as the enzyme retains some of its potency. Children with ML III may present with mild mental retardation and some developmental problems.
- ML IV (Berman Syndrome) – is caused by alterations of protein in the cell thought to be linked with the movement of molecules like calcium across cell membranes. ML IV is often confused with cerebral palsy because of similar symptoms like lack of motor coordination, speech issues and some developmental delays. In some cases, corneal clouding and vision impairment occur.
What are the Symptoms of Mucolipidosis?
Symptoms maybe mild, moderate or severe depending on the type of ML.
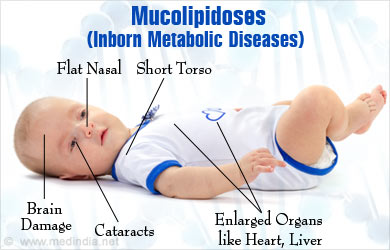
There is a common cluster of symptoms occurring across the four types of ML:
- Facial features like flat nasal bridge and puffy eyelids
- Short torso
- Lack of muscle coordination or ataxia
- Hypotonia or reduced muscle tone
- Developmental delays and mental retardation
- Enlarged organs like heart, liver and spleen
- Corneal clouding and vision impairment
- Respiratory issues
How are Mucolipidoses Inherited?
Mucolipidoses are genetically-inherited autosomal recessive disorders.
Mucolipidoses occur when both parents carry copies of the defective gene. The child usually inherits the disease when he/she receives two copies of the defective gene, one from each parent. Carriers (those who have one defective gene) do not express the disease but they can pass on the defective gene to their offspring.
Genetic testing is available to detect carriers of the gene. Pre-natal diagnosis is also available to detect the presence of ML in the fetus. A procedure known as chorion villi sampling (CVS) is done between the 8th and 10th week of pregnancy. This procedure involves obtaining and testing a micro sample of the placenta.
Parents who are carriers of ML genes or those who have conceived a baby with the genetic defect must be genetically counseled with adequate psychological support.
How are Mucolipidoses Diagnosed?
Diagnosis of mucolipidoses is made based on a combination of medical history, physical examination and clinical investigations.
ML I, II and III are usually confirmed through a blood test which measures enzyme activity in the person’s white blood cells (WBCs). A lower level of activity indicates the particular enzyme deficiency.
Skin biopsy is also a useful method of diagnosis where a small sample of the skin from the patient is taken and is grown in cell culture. The activity of specific enzymes is then measured in the culture cells.

ML IV is usually confirmed when a conjunctival swab is found to have several inclusions.
How are Mucolipidoses Treated?
There is no permanent cure for ML and treatment is based on addressing the symptoms.
ML are treated on a case-to-case basis in providing support for patients. Symptoms are tackled and the overall aim is to keep the individual healthy and functional for as long as possible. For example, vision impairment can be avoided by corneal surgery to remove a thin layer of the cloudy cornea. Respiratory infections are treated with antibiotics. Nutritional supplements may be given to maintain strength.
How can Mucolipidoses be Prevented?
Mucolipidoses can be prevented through genetic counseling. Genetic counseling is essential for those who are suspected carriers or those who have a family history of genetic disorders. Pre-natal testing is also useful if the parents are confirmed to be carriers.






