- Neonatal Resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - (http://pediatrics.aappublications.org/content/126/5/e1400.full)
- Neonatal ehandbook - (http://www.health.vic.gov.au/neonatalhandbook/procedures/resuscitation.htm)
- Neonatal Resuscitation - (http://circ.ahajournals.org/content/122/18_suppl_3/s909.full.pdf+html)
What is Neonatal Resuscitation?
Neonatal resuscitation is the manual help given by the physician to the baby after its birth to help it breathe and heart to beat in emergency situations.
Neonatal resuscitation program thus forms an important part of emergency neonatology. The presence of a neonatologist is compulsory in the labor room during the delivery of a baby. After the birth of the baby, the obstetrician immediately hands over the baby to the neonatologist. The neonatologist assesses the general health status by a score called as Apgar’s score and performs neonatal resuscitation if the score is low.

Three to five percent of the 25 million infants born every year in India develop asphyxia during birth. Asphyxia is a condition where there is decreased oxygen and increased carbon dioxide in the body. Blood flow is decreased through the body and is accompanied by a decrease in pH of blood. Asphyxia leads to multi-organ dysfunction that may cause death or lead to neurological complications later in life.
Neonatal resuscitation aims to decrease neonatal death and prevent the development of neurological complications because of asphyxia during birth.
Who Requires Neonatal Resuscitation?
One must carefully evaluate the list of risk factors, in which asphyxia can be anticipated in the coming baby. Some of the babies can be listed out to be the definite candidates of neonatal resuscitation, whereas some babies can be a complete surprise. Thus it is necessary, that every delivery be viewed as emergency and help should be immediately available to resuscitate the baby if necessary.
The risk factors that could increase the chances of the fetus developing neonatal asphyxia can be divided into maternal and fetal, they are as listed:
- Maternal Risk Factors:
- Prolonged labor more than 18 hrs
- Per vaginal bleeding in second and third trimester
- Pregnancy induced hypertension
- Addictions of tobacco and alcohol
- Gestational diabetes of mother i.e. diabetes that occurs during pregnancy
- Intake of medications like lithium, NSAIDs etc.
- Maternal infections such as rubella, chlamydia, syphilis and many more.
- No antenatal care received during pregnancy
- Multiple fetuses (twins, triplets, etc.)
- Fetal Risk Factors:
- Premature infants; additional precautions may be required while administrating resuscitation in these babies.
- Low birth weight infants
- Increased or decreased amount of amniotic fluid (the fluid that surrounds the fetus)
- Congenital malformations affecting breathing and heart circulation
- Abnormal position of baby (breech or transverse etc.)
- Prolapse of umbilical cord, where the umbilical cord comes out of the uterus before the baby
How to Prepare for Resuscitation and How to Evaluate the Baby?
Every delivery should be considered as an emergency, and the need for neonatal resuscitation should be anticipated irrespective of the pre-existing risk factors. The labor room of the hospital should be equipped with a ready in use radiant heat source to warm the baby, all resuscitation instruments such as suction catheters, meconium aspirators, self-inflating neonatal resuscitation bags, face-masks for both term and pre-term babies, intubation equipment such as laryngoscopes and endotracheal tubes and at least one person skilled in neonatal resuscitation.
As soon as the baby is born, the pediatrician evaluates the baby for resuscitation on the basis of Apgar’s score. It takes into account following things: heart rate, respiration, muscle tone, reflex irritability, and color of baby.
A quick way to assess if the baby requires resuscitation is by addressing the following questions.
- Is the baby born at term?
- Is the baby breathing or crying?
- Does the baby have good muscle tone? (flexed posture and active movements of baby indicate good tone)
If answers to all the above questions are “YES”, then the baby does not require any resuscitation and is given for routine care that includes cutting the cord, giving warmth to the baby, clearing the airway of baby, drying the baby, and recording vital parameters.
If answers to even one of the above questions is “NO”, the baby needs immediate resuscitation.
What is TABC of Neonatal Resuscitation?
TABC are the components of neonatal resuscitation. They stand for Temperature, Airway, Breathing, and Circulation. Let’s see each one of them in brief.
- Temperature: Preterm babies are more prone to develop low body temperature or hypothermia. Thus, they must be given extra care. The labor room is often pre-warmed, the baby is placed under a radiant warmer and the temperature is monitored continuously. Breastfeeding should be continued so that the skin-to-skin contact with the mother gives the baby warmth; this is called as kangaroo mother care.
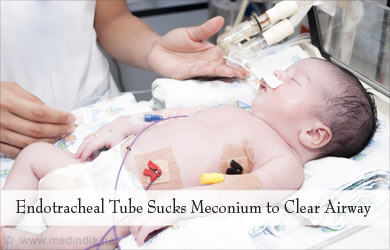
- Airway: The airways should be clear so that the baby can breathe. Secretions if present are removed from mouth and nose by wiping them with a clean cloth or by suctioning with the help of suction catheter. The mouth should always be suctioned before nose. If the baby has aspirated meconium and is not vigorous, endotracheal intubation is done and the meconium is sucked out. Meconium is the first feces of the newborn. In endotracheal intubation, an endotracheal tube is inserted through the mouth and placed in the windpipe.
- Breathing: In order to find out if the blood contains enough oxygen and therefore the baby is breathing well, a small instrument called a pulse oximeter is placed on a limb. If the oxygen content is less, respiration is initiated by using positive pressure ventilation, through bags and masks or by doing endotracheal intubation whenever necessary. Positive pressure ventilation is required when the infant is breathless or gasping, the heart rate is less than 100 beats per minute and the baby has persistent bluish discoloration of skin and mucous membranes despite administration of 100 % free flowing oxygen
- Circulation: Lastly, while resuscitating a newborn, circulation of blood has to be stimulated and maintained with chest compressions and medications as indicated
- Chest Compressions: Chest compression is done by rhythmically compressing the breastbone by thumb technique or two finger technique. In this procedure, the heart is compressed against the spine and the pressure within the chest increases. This mechanically pumps blood to the body. The administration of positive pressure ventilation given along with the chest compressions ensures delivery of oxygenated blood.
Chest compressions are given only in conditions, where heart rate is less than 60 beats per minute despite giving 30 seconds of positive pressure ventilation. It is to be discontinued after heart rate reaches 60 beats per minute or more.
- Medications: Resuscitation medications required may be epinephrine, intravenous solutions like normal saline and ringer lactate to increase the blood volume, and naloxone in case the respiratory depression. Epinephrine is given intravenously if the heart rate is less than 60/min despite PPV and chest compressions for 30 seconds.






