- SEER Stat Fact Sheets: Thyroid Cancer - (http://seer.cancer.gov/statfacts/html/thyro.html)
- Thyroid Cancer Types, Stages and Treatment Overview - (http://www.thyca.org/about/types)
- Thyroid Cancer - (http://www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf)
- Podnos YD, Smith D, Wagman LD, Ellenhorn JD. Radioactive iodine offers survival improvement in patients with follicular carcinoma of the thyroid. Surgery. 2005;128(6):1072-6.
- King AD. Imaging for staging and management of thyroid cancer. Cancer Imaging. 2008; 8(1): 57-69.
- Chiu CG et al. Hemithyroidectomy is the preferred initial operative approach for an indeterminate fine needle aspiration biopsy diagnosis. Can J Surg. 2012 Jun; 55(3): 191-198.
- Schneider DF, Chen H. New Developments in the Diagnosis and Treatment of Thyroid Cancer. CA Cancer J Clin 2013;63:373-394
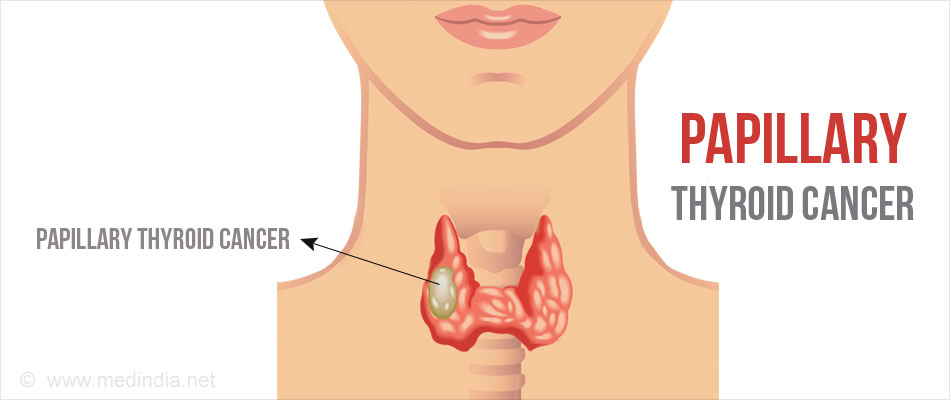
What is Papillary Thyroid Cancer?
Papillary thyroid cancer is the most common type of thyroid cancers accounting for about 80% of all diagnosed thyroid cancers. The thyroid gland is located in front of the neck. It is a butterfly-shaped endocrine gland, with a right lobe and a left lobe connected through a thin piece of tissue, the isthmus. The thyroid gland secretes important hormones (triiodothyronine and thyroxine) that help the body to function normally.
Papillary thyroid cancer is most common in individuals between 25 and 65 years of age. It tends to grow very slowly and often affects only one lobe of the thyroid gland. It is generally treatable with a good prognosis and is rarely fatal.
What are the Variants of Papillary Thyroid Cancer?
Besides the classical type of papillary thyroid cancer, the variants of papillary thyroid cancer include the following:
- Mixed papillary - follicular variant, which is the most common variant
- Columnar, tall cell, insular, and diffuse sclerosing variants, which are rarer but faster growing
What are the Risk factors for Papillary Thyroid Cancer?
Gender and Age
Thyroid cancer can occur at any age, but women in their 40s or 50s are 2-3 times more likely to develop thyroid cancer. Anaplastic thyroid cancer is usually diagnosed after the age of 60 years.
Genetics
People with a genetic condition called familial adenomatous polyposis (FAP) have an increased risk of some other cancers, including papillary thyroid cancer. Patients with Cowden disease are also associated with an increased risk for papillary thyroid cancer. Other genetic variations have also been associated with papillary thyroid cancer.
Radiation Exposure
Exposure to external radiation in the head and neck region is one of the most well known risk factors for thyroid cancer. Children exposed to radioactive fallout from the Chernobyl accident have demonstrated an increased incidence of papillary thyroid cancer. Exposure to radioactive iodine, also called I-131 or RAI, especially in childhood can cause papillary thyroid cancer.
Dietary Iodine Content
Papillary thyroid cancer occurs with higher frequency in regions where dietary iodine content is low.
What are the Symptoms of Papillary Thyroid Cancer?
Papillary thyroid cancer may not show symptoms in the early stages of the disease. Some of the common symptoms include:
- A lump or a hard swelling in the front of the neck.
- Difficulty in swallowing
- Hoarseness of voice
- Noisy type of breathing called stridor
- A feeling of tiredness
- Coughing or choking spells
Where does Papillary Thyroid Cancer Spread To?
Papillary thyroid cancer can spread to:
- The nearby tissues of the neck
- Lymph nodes of the neck, which are bean-shaped bunches of immune system cells
- Distant sites like the lungs, liver or the bones
Papillary thyroid cancer spreads more commonly to regional lymph nodes than to distant sites.
How to Diagnose Papillary Thyroid Cancer?
Tests used in the diagnosis of papillary thyroid cancer include the following:
Physical examination should include an evaluation of size and character of thyroid nodules, and for the presence of neck tenderness that may be present in patients with thyroiditis. Examination of the throat with laryngoscopy should be performed for patients with hoarseness or change in voice. Papillary carcinoma rarely presents as lymph node swelling in the presence of an otherwise normal thyroid gland.
A blood test to check the TSH level should be done to evaluate if the patient is euthyroid (i.e. normal thyroid function), hyperthyroid (i.e. hyperactive thyroid), or hypothyroid (i.e. low thyroid).
Ultrasound is the most important imaging test used to diagnose papillary thyroid cancer. The appearance of the cancer on ultrasound is commonly described as a solid hypoechoic nodule with a well or poorly defined margin, with small foci of punctate calcification. It may also appear as a cyst.

An ultrasound-guided fine needle aspiration biopsy (FNAB) or core biopsy is the investigation of choice for initial diagnosis of thyroid cancer. In this technique, cells are removed from the nodule into the needle (i.e. aspirated) under ultrasound guidance and looked at under the microscope by a specially trained doctor called a cytologist.
An MRI is used to diagnose thyroid tumor invasion into the trachea or esophagus with 100% specificity.
What is the Treatment for Papillary Thyroid Cancer?
Surgery
Surgery is the most commonly used treatment option for treating thyroid cancers.
Small tumors that have not spread outside the thyroid gland can be treated by just removing the side of the thyroid containing the tumor (lobectomy or hemithyroidectomy). Most patients recover fairly quickly after hemithyroidectomy and resume normal activities within one to two weeks.
Isthmusectomy is another standard surgical technique which is a safe alternative to thyroid lobectomy in patients who have nodules confined to the isthmus and pyramidal lobe in the central part of the thyroid gland. It minimizes potential damage to the recurrent laryngeal nerves and parathyroid glands.
A total thyroidectomy may be needed in some patients.
The affected lymph nodes may also be removed during the surgery.
Radioactive Iodine
Radioactive iodine can also be used to destroy the cancer tissue remaining after surgery. In order to stimulate the intracellular uptake of isotope, the TSH (Thyroid Stimulating Hormone) concentration should be at least as high as 30 mU/L. There are two methods for achieving this level. The traditional method requires the patient to withdraw from thyroid hormone replacement over 4–6 weeks whereas in newer method recombinant human TSH (rhTSH) is administered in the form of intramuscular injections on two consecutive days followed by radioactive iodine on the third day. The benefit of this method is that the patient does not experience an extended period of hypothyroidism as with hormone withdrawal.
Patients treated with thyroidectomy or radioactive iodine may require replacement of thyroid hormone with medications following the treatment.
Health tips
- There is not yet clear if there are lifestyle changes that can help you once you have developed thyroid cancer but still you can start with tobacco or smoking cessation.
- Exercises can improve your physical and emotional health. Along with a good diet, they will also help you get to and stay at a healthy weight.
- You may have to control your dietary iodine intake.