- What to do about pelvic organ prolapse - (http://www.health.harvard.edu/family-health-guide/what-to-do-about-pelvic-organ-prolapse)
- Surgical Treatments for Vaginal Apical Prolapse - (http://ogscience.org/doix.php?id=10.5468/ogs.2016.59.4.253)
- Pelvic Organ Prolapse - (https://www.nafc.org/pelvic-organ-prolapse/)
- Step-By-Step Approach To Managing Pelvic Organ Prolapse - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc1949085/)
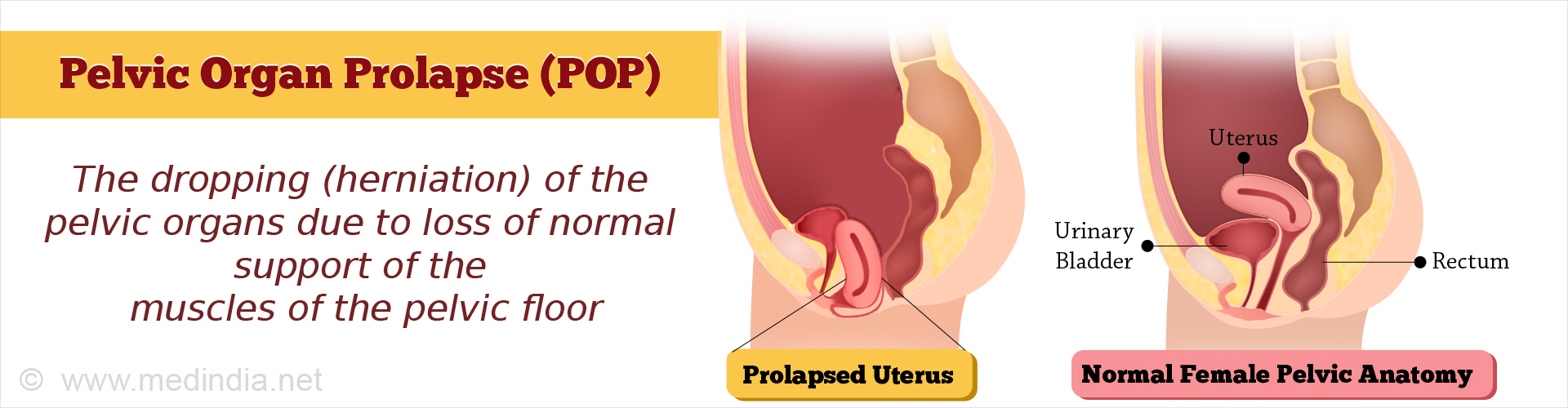
What is Pelvic Organ Prolapse?
Pelvic Organ Prolapse (POP) is the dropping (herniation) of the pelvic organs due to loss of normal support of the muscles of the pelvic floor.
Pelvic organ prolapse or vaginal hernia is caused by several factors. The condition is very uncomfortable for women. It can be managed conservatively by pelvic floor exercises lifestyle modifications and using pessary. In severe cases, surgery is the only option.
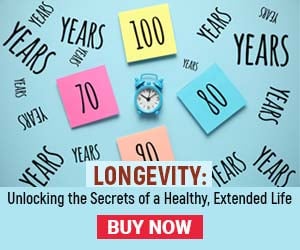
Anatomy of the Female Pelvis
The pelvis is the region which starts approximately 4 inches below the navel and extends up to the vagina, which is the tubular tract extending from the uterus to the exterior in females.
Bones of the Pelvis
The pelvis consists of three bones – the ilium, ischium and pubis on either side, which form the pelvic girdle. The pelvic bones in females are larger and broader than that of males and has a large cavity to hold the developing baby. The sacrum, which consists of 5 fused bones of the vertebral column, connects the two sides of the pelvis at the iliac crest. Located below the sacrum is the coccyx (also called the tail bone), consisting of 3-5 fused bones that forms the base of the vertebral column. At the lower part of the ilium, towards either side, is a socket called the acetabulum to which the head of the femur articulates via a ball-and-socket joint. On the front side, the pelvis is united by two pubic bones that are joined by hyaline and fibrocartilage, and collectively called the pubic symphysis. During childbirth, this joint becomes flexible and allows the baby to pass through the birth canal.
Organs of the Pelvis
The pelvic organs in the female include the uterus or the womb with a pair of tubes and ovaries, one on either side of the uterus. The uterus is connected to the vagina via the cervix.
The urethra of females originate from the internal urethral orifice of the urinary bladder and passes down anterior (in front) to the vagina and opens through the external urethral orifice into the vulva.
The pelvic region also contains the lower portions of the gastrointestinal (GI) tract. These include portions of the small and large intestine. The lower sigmoid colon connects with the rectum, which is also housed within the pelvis at the posterior (behind) portion of the pelvis, behind the urinary bladder and below the uterus.
The rectum in turn opens to the exterior through the anus, a circular band of sphincter muscle that controls the periodic release of feces, the excretory product of the digestive system.
Muscles of the Pelvis
The organs of the pelvis are held in place by several muscles and ligaments that are collectively called the pelvic floor. These support the organs so that they do not prolapse (slip down) under the influence of gravity.
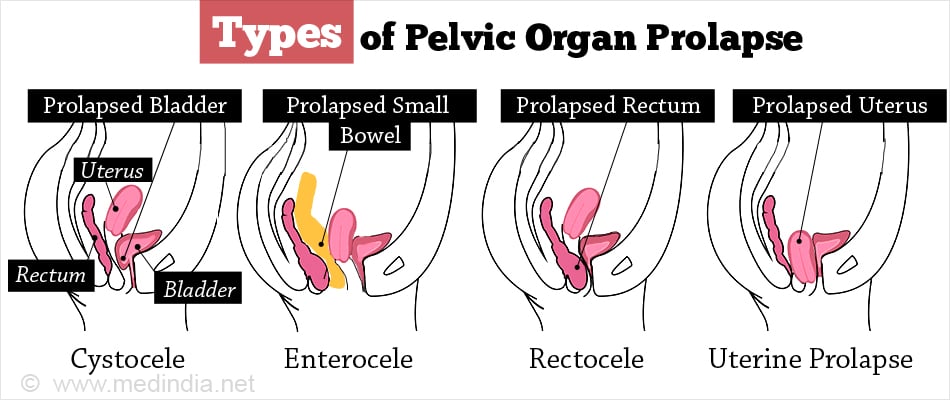
What are the Types of Pelvic Organ Prolapse?
There are five major types of POP, which are briefly described below:
- Cystocele: This condition is caused by weakening of the anterior (front) wall of the vagina, resulting in drooping (herniation) of the urinary bladder into the vagina. Sometimes, the urethra may also herniate, resulting in a condition called urethrocele, which can cause stress urinary incontinence. If both the urinary bladder and the urethra herniate into the vagina, the condition is called cystourethrocele.
- Enterocele: This condition occurs when both the anterior and posterior walls of the vagina separate, because of which the small bowel herniates into the vagina. Enterocele is more common following hysterectomy i.e. surgical removal of the uterus.
- Rectocele: This condition arises due to the weakening of the posterior vaginal wall, causing the rectum to herniate into the vagina.
- Uterine Prolapse: This condition arises when the uterosacral ligaments supporting the upper portion of the vagina become weak, which also causes weakening of the anterior and posterior vaginal walls. This leads to the drooping down of the uterus into the vagina.
- Uterine prolapse exhibits 3 stages:
- First-degree uterine prolapse, where the lower portion of the uterus herniates into the vagina;
- Second-degree uterine prolapse, where the uterus enters the lower portion of the vagina;
- Third-degree uterine prolapse, where the uterus protrudes out of the vaginal opening.
- Vaginal Vault Prolapse: This condition occurs when the support provided by the uterus to the upper portion of the vagina (the vaginal vault) ceases, usually following hysterectomy. Vaginal vault prolapse generally occurs in 10% hysterectomy patients.
What are the Causes of Pelvic Organ Prolapse?
The major causes or risk-factors for developing POP include the following:
- Childbirth: Childbirth involving multiple deliveries, prolonged labor and birth of large-sized babies predispose women to POP.
- Age: POP usually occurs in women with a comparatively higher age, usually above 40 years.
- Menopause: Post-menopausal women are at a higher risk of developing POP. This is because the levels of estrogen, which helps in strengthening the muscles and ligaments, is very low after menopause.
- Muscular Strain: Chronic muscular strain arising from efforts to defecate or urinate due to constipation or retention of urine in the bladder, can result in POP.
- Obesity: Women who are obese are at a higher risk of developing POP.
- Hysterectomy: A woman may be at a higher risk of developing POP if she has had prior hysterectomy. This is because in the absence of the uterus, the support provided by it to the vagina is lost, predisposing the woman to POP.
- Pelvic Surgery: Prior pelvic surgery can result in weakening of the pelvic muscles and ligaments, thereby increasing the chances of POP.
- Heavy Exercise: Heavy strenuous exercises such as frequent weight-lifting can lead to POP.
What are the Symptoms of Pelvic Organ Prolapse?
POP is one of the most uncomfortable disease conditions experienced by women. The condition is characterized by a number of symptoms that contribute to the feeling of uneasiness. The most common symptoms of POP are as follows:
- A feeling of pain and pressure in the pelvic area.
- Lower back pain.
- A feeling of something protruding out of the vagina.
- Bowel movement problems, including constipation.
- Painful sexual intercourse.
- Renal incontinence (involuntary or uncontrolled urination) or an urge to urinate, particularly at night.
- Bleeding from the vagina.
- A feeling of distension or stretching in the groin.
How do you Diagnose Pelvic Organ Prolapse?
If POP is suspected, before any investigations are carried out, a thorough medical history will be taken by the doctor, including number of pregnancies as well as family history of POP. This is followed by a physical examination, with a major focus on pelvic exam. An instrument called a speculum is usually used for this purpose. To confirm the clinical diagnosis, the following investigations may be ordered:
- Intravenous Pyelogram (IVP): This procedure involves injecting an iodinated radio-opaque contrast medium into a vein, followed by taking x-rays of the abdomen at different time periods. IVP is capable of showing the shape, size, structure, and positions of the different parts of the urinary system, such as the kidneys, urinary bladders, ureters and urethra.
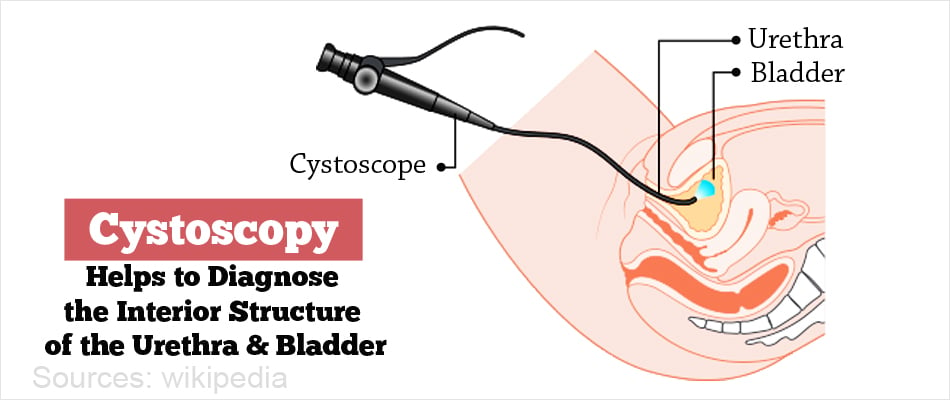
- Cystoscopy: This procedure is used to observe the interior of the urethra and urinary bladder using a device called a cystoscope. This device consists of a fine tube attached to a viewer, which is inserted through the urethra up to the urinary bladder. This allows a thorough examination of the interior structures that cannot be clearly observed using x-ray.
- Computed Tomography: This procedure is commonly called CT scan. It involves taking a series of x-ray photographs of the body (in this case, the pelvic region) from different angles and then analyzing the images by a computer software, which generates cross-sectional slices for viewing. CT scans yield much greater detail than conventional x-ray images.
- Urodynamic Testing: Tests to study urodynamics determine how well the urinary bladder and urethra are performing their function in storing and releasing urine. Urodynamic testing is particularly useful for investigating renal incontinence, a major symptom of cystocele (urinary bladder prolapse).
What are the Treatment Options for Pelvic Organ Prolapse?
If POP has been confirmed diagnostically, there are several conservative management options available before considering surgical intervention. These strategies have the advantage of being cheap, minimally invasive, with less chances of morbidity and mortality (compared to surgery), and can give increased patient satisfaction and patient compliance. These approaches are also suitable for patients awaiting surgery. These are briefly highlighted below:
Conservative Management
- Pelvic Floor Exercise: This exercise is also called Kegel exercise after Arnold Kegel, who first described this exercise in 1948. The Kegel exercise involves repeated contraction and relaxation of the muscles of the pelvic floor, thereby strengthening these muscles and increasing the muscle tone. It also improves stress urinary incontinence.
- Pessary: A pessary is a device made of medical-grade silicone that can be inserted into the vagina to support the areas where the pelvic organs have prolapsed. This device is safe, cost-effective and minimally invasive. Pessaries can be supportive (e.g. ring) or space-occupying (e.g. doughnut, cube).
- Lifestyle Modifications: Lifestyle changes include:
- Consuming lots of fiber in the diet (~20 g daily) to prevent constipation that can increase the pelvic pressure;
- Attaining and maintaining a healthy weight that is appropriate for the height;
- Avoiding lifting heavy objects that can stress the pelvic muscles, and
- Quitting smoking as this can cause coughing which can aggravate POP.
Surgery
If the condition does not improve or worsens further, a surgical intervention may be considered. The choice of the surgical procedure depends on the severity, organs involved, age, future pregnancy plans, as well as other medical conditions. Prolapse surgery can be done transvaginally, abdominally, laparoscopically or by robotic surgery. The various types of surgical approaches are briefly highlighted below:
- Repair of Cystocele: A prolapsed bladder can be repaired by surgery. Likewise, a prolapsed urethra (urethrocele) can also be repaired.
- Repair of Rectocele: A rectocele can be repaired along with a prolapsed small bowel (enterocele) by surgical intervention.
- Hysterectomy: This involves the surgical removal of the whole uterus. Hysterectomy is often recommended in case of a uterine prolapse, but is carried out only if the patient does not want any more children.
- Vaginal Vault Prolapse: This condition is usually treated by laparoscopic surgery to repair the vaginal wall.
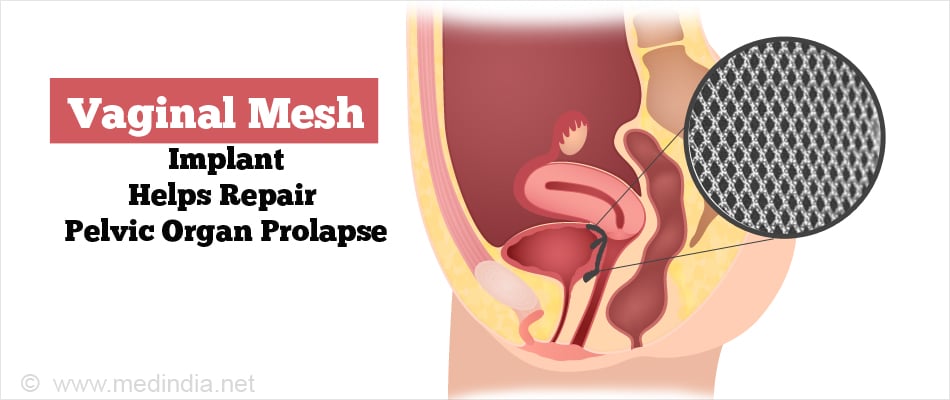
- Implantation of Vaginal Mesh: It is a surgical procedure used for repairing POP and stress urinary incontinence. The mesh is implanted permanently to reinforce the weakened vaginal wall as well as to support the urethra and urinary bladder for alleviating stress urinary incontinence.
- Vaginal Obliteration: In this surgical procedure, the vagina is completely closed-up.
Other Strategies
- Hormone Replacement Therapy (HRT): If POP occurs after menopause, there will be a deficiency in estrogen, which might cause vaginal dryness and painful sex. Although HRT cannot fully treat POP, these symptoms can be alleviated by administration of estrogen.
- Pelvic Floor Stimulation: Thisis a high-end treatment option that involves placing electrical stimulators intravaginally to stimulate the pelvic floor muscles. This strategy can be used when pelvic floor exercises does not yield satisfactory results.
Can Pelvic Organ Prolapse be Prevented?
Since there are several causes of POP, no single strategy can be used as a preventive measure. However, in general, excessive pressure build-up in the abdomen and pelvic region should be avoided, as this can precipitate POP. In this regard, the following measures can be adopted:
- Maintain Normal Weight: The normal weight for height and age should be maintained. In case of overweight and obese women, there is a greater need to reduce weight as being overweight predisposes to POP.
- Avoid Constipation: Chronic constipation causes difficulty in passage of bowel, which can increase chances of POP due to increased pressure in the pelvic cavity. A diet rich in fiber should be consumed to prevent constipation.
- Treat Chronic Cough: Any form of chronic cough should be treated immediately, as this causes increased abdominal and pelvic pressure that can precipitate POP. In this connection, smoker’s cough can have the same detrimental effect. Therefore, quit smoking.
- Avoid Strenuous Activities: Avoid lifting heavy weights which increases pressure in the abdominal and pelvic cavities and can cause POP.
- Do Pelvic Floor Exercise Regularly: Doing pelvic floor or Kegel exercise on a regular basis can strengthen the pelvic floor muscles, thereby preventing POP.

Health Tips to Avoid Pelvic Organ Prolapse:
- Avoid multiple childbirths: Having lesser number of children may reduce your chances of POP at a later stage in life.
- Avoid heavy strenuous exercises: Light aerobic exercises are fine, but heavy exercises involving weights should ideally be avoided by women.
- Consult your doctor about hormone replacement therapy (HRT) following onset of menopause: Since menopause increases the risk of occurrence of POP, it might be a good idea to ask your doctor if HRT would be suitable for you. In HRT, synthetic sex hormones such as estrogen are administered in post-menopausal women.
- Keep your body fit and trim: Maintain your weight in proportion to your height. Follow a balanced diet regimen; do yoga and light free-hand exercises; and walk briskly for 30-40 minutes daily.