- Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004 Aug 10. 110 (6):738-43.
- Hiatt W. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001 May 24;344(21):1608-21.
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007 Jan. 45 Suppl S:S5-67.
- Suzuki J, Shimamura M, Suda H, Wakayama K, Kumagai H, Ikeda Y, et al. Current therapies and investigational drugs for peripheral arterial disease. Hypertens Res. 2016 Apr. 39 (4):183-91.
- Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317-24.
- Thukkani AK, Kinlay S. Endovascular intervention for peripheral artery disease. Circ Res. 2015 Apr 24. 116 (9):1599-613.
- Beebe HG, Dawson DL, Cutler BS, et al. A new pharmacological treatment for intermittent claudication: results of a randomized, multicenter trial. Arch Intern Med. 1999 Sep 27;159(17):2041-50.
What is Peripheral Artery Disease?
Peripheral Arterial Disease (PAD) is a condition where arteries begin to narrow resulting in blockage of blood flow. It is a common condition that affects approximately 9% of the population; however, only a few show symptoms.
Plaque builds up in the arteries that carry blood to your head, organs, and limbs. This plaque is made up of cholesterol, calcium, fibrous tissue, and other substances from the blood. This disease might get overlooked due to the subtle nature of symptoms.
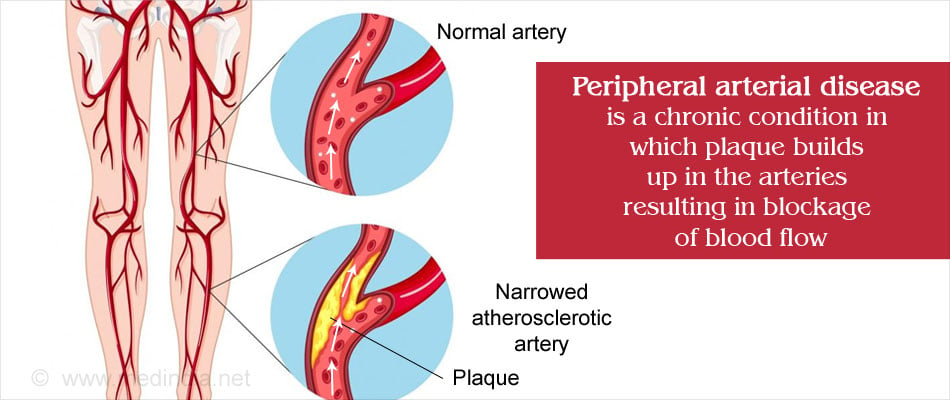
PAD commonly affects individuals with type 2 diabetes and with high cholesterol. It usually affects the arteries of the legs; hence this condition is diagnosed when patients present themselves with leg and foot problems. Blocked arteries cause numbness and pain in the legs.
PAD also affects arteries leading to the head, arms, kidneys and stomach.
Peripheral vascular disease (PVD) is a disorder that can affect any blood vessels outside the brain and heart. Typically, this includes all blood vessels while PAD is restricted to arteries that carry oxygen rich blood. PAD is the most common form of PVD; hence both terms are used interchangeably.
Individuals with PAD are at a high risk for coronary heart disease, heart attack, stroke, and ischemic heart disease.
What are the Causes of PAD?
Vascular disease may be a hereditary condition. You may need to discuss this with your doctor.
The most common cause of PAD is atherosclerosis. Atherosclerosis is the buildup of plaque in the arteries. The exact cause for this build up of plaque is not known.
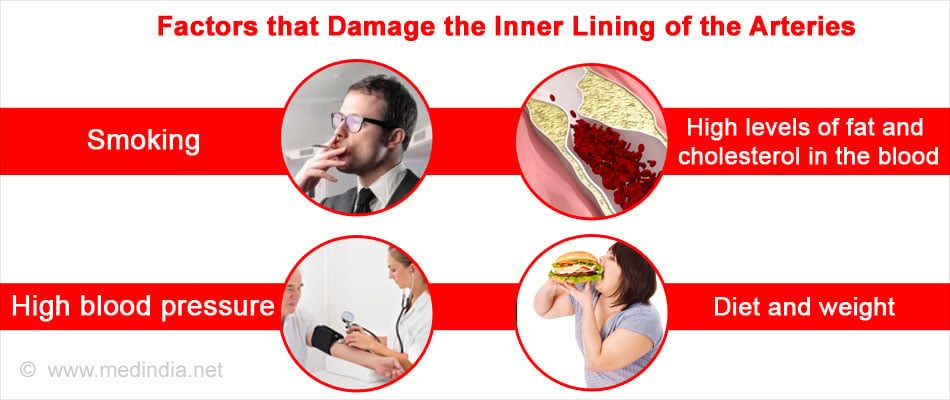
This condition can start due to certain factors that damage the inner lining of the arteries. These factors are as follows:
- Smoking
- High levels of fat and cholesterol in the blood
- High blood pressure
- Insulin resistance that leads to high sugar or diabetes
- Diet and weight
When these factors cause damage to the arteries, the body starts the healing process spontaneously. This leads to plaque formation at the site of damaged arteries. This plaque can break off from the site and lead to the formation of blood clot. This formation of blood clot and plaque can severely narrow and damage arteries causing reduced blood flow to vital organs.
What are the Signs and Symptoms of PAD?
Individuals with PAD show the following symptoms:
- When walking, climbing stairs, or exercising, individuals show pain, numbness, aching, or heaviness in the muscles of the leg. There may be cramping of the muscles of the legs, calves, and feet. Patients with PAD may experience a sensation of pins and needles in the legs or feet. These may subside after resting but return on exertion. This is known as intermittent claudication.

- A weakened or absent pulse in the affected leg.
- Wounds on the feet and leg that heal slowly.
- Pale bluish color of the leg.
- Lower temperature on one leg compared to the other.
- Poor nail growth along with reduced hair growth on the affected leg.
- Erectile dysfunction in men especially with diabetes.
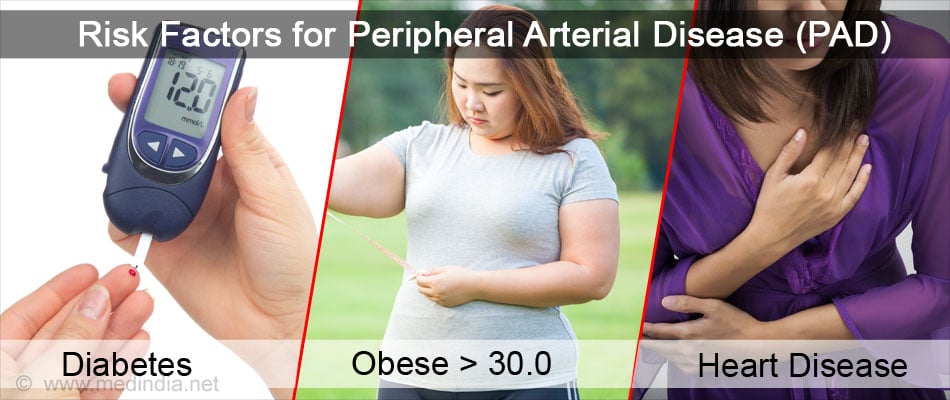
What are the Risk Factors for PAD?
Many people with PAD do not show or experience any symptoms. However, if you do not have PAD, but have the following risk factors, you should check for this vascular disease.
- Over 70-years-old
- Over 50-years-old and have a history of smoking or diabetes
- Younger than 50 years and have diabetes
You are generally at risk for PAD if you have -
- Been smoking
- Diabetes
- A body mass index of more than 30 indicating obesity
- High blood pressure
- High cholesterol (especially high amounts of low-density lipoprotein and low amounts of high-density lipoprotein)
- A family history of PAD, heart disease or stroke
- Reached 50 years of age
What are the Complications of PAD?
Critical limb ischemia: Open sores that do not heal, an injury or an infection in the lower limbs can later progress to tissue death or gangrene. If not treated or controlled immediately, this may call for amputation of the leg.
Stroke and heart attack: If you have PAD, your risk for heart attack, stroke and transient ischemic disease increases tremendously.
Although PAD is a serious disease, it is treatable and you can avoid complications with immediate treatment. If you suffer from PAD, ensure that you see your doctor regularly to check for underlying conditions such as atherosclerosis and cholesterol.
How do you Diagnose PAD?
PAD is diagnosed based on medical history, family history, physical examination, and a few tests. A quick diagnosis is necessary as people with PAD are more susceptible to heart attack and stroke.
- Physical Examination: A complete medical history will be taken by your physician, which is followed by a physical examination. He will examine your legs and check for weakened or absent pulse that indicate the state of blood circulation. He will also check your pulse in the legs for any abnormal sounds. Often a bruit (whooshing sound) is heard, which is a sign of narrowed arteries.
He may check the blood pressure on both limbs to compare the difference. Wounds and their rate of healing will also be inspected.
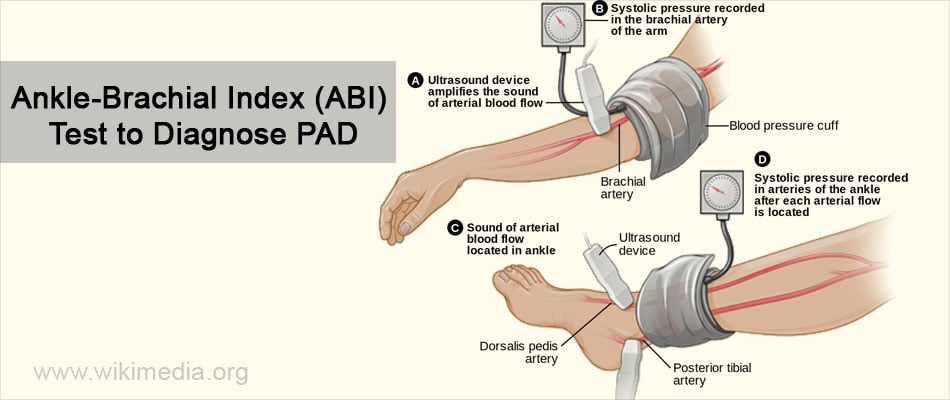
- Ankle-Brachial Index (ABI) Test: A simple ABI test will be performed where the blood pressure in your ankle is taken and compared with the blood pressure in your arms. This is to assess the state of blood circulation in your limbs. This diagnostic test can help to show whether PAD is affecting your limbs.
- Doppler Ultrasound is performed to check the blood flow in major arteries and veins in the limbs.
- Treadmill Test shows the severity of symptoms and how exercise can induce symptoms.
- Magnetic Resonance Angiogram (MRA) uses magnetic and radio waves to capture images of the blood vessels of your limbs. Thus, the extent of blockage and narrowing of blood vessels can be ascertained.
- Arteriogram helps to demonstrate the road map of the arteries. It can show the precise location of the blockage, which also includes the severity of damage. This is done by injecting a dye into the blood vessels, and its movement is monitored.
- Other blood tests will be advised to check for risk factors such as diabetes and cholesterol.
How do you Treat PAD?
The aim of treatment is to prevent a heart attack and stroke, reduce symptoms of claudication, and improve mobility of the affected limb. By improving the quality of life and reducing risk factors, treatment helps to reduce the chances of complications.
PAD, if left untreated, can result in severe infection and gangrene, which calls for immediate amputation of the foot leading to permanent disability.
The standard protocol for the treatment of PAD includes lifestyle changes to include healthy heart habits, medicine, and in some cases, surgery.
Healthy heart habits are as follows:
- Perform moderate physical activity
- Quit smoking
- Eat healthy and maintain a healthy weight
The following medications are administered:
- Cholesterol lowering drugs
- Drugs to reduce blood sugar
- Blood pressure medications
- Blood thinners to reduce blood clot formation
- Symptom relief medications
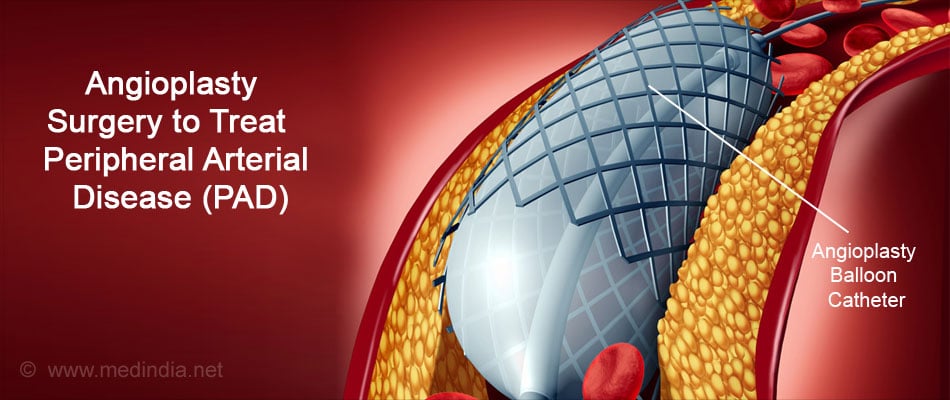
Angioplasty and Surgery
In serious cases, where no relief is observed with medications and lifestyle modifications, the physician may advise surgery.
Bypass Grafting: A blood vessel from another part of the body or a synthetic tube is used as a graft to bypass the blocked area of the artery.
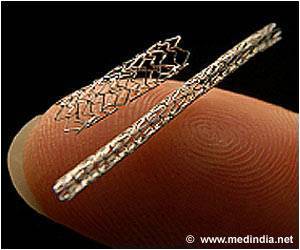
Angioplasty Surgery: A catheter with a balloon fitted at the end is used to disrupt the plaque in the blocked artery. The surgery is performed to improve blood flow by reducing the extent of blockages in the artery. A stent is then placed there to keep the artery open.
Atherectomy: A catheter is used to insert a cutting device into the blocked artery to shave the plaque formed. A laser technique can also be used to dissolve the plaque.
How do you Prevent PAD?
The best way to prevent PAD is to understand the risk factors and control them. This will help delay the onset of this vascular disease. If you have a family history of vascular diseases, you should take more precautions and consult your physician regularly. Prevention of PAD can be achieved by the following:
- Screen periodically for PAD using the ankle–brachial index. This helps to keep track of the blood circulation in your limbs.
- Eat healthy and heart-friendly foods
- Quit smoking
- If you are obese, lose weight and cut down on overeating
- Exercising regularly

Health Tips
Few health tips if you are living with PAD:
- If your legs pain after walking, take a small break and rest for a while. Allow the pain to reduce before walking again.
- Take part in a supervised exercise program.
- Check your feet and toes for soreness or any kind of infections.
- Keep your feet clean and maintain foot hygiene.
- Always wear comfortable shoes.
- If you have bunions, corns, or calluses seek immediate care.