- Spasmodic Dysphonia - (https://www.nidcd.nih.gov/health/spasmodic- dysphonia)
- What is Spasmodic Dysphonia? - (https://www.uhb.nhs.uk/Downloads/pdf/PiWhatIsSpasmodicDysphonia.pdf)
- Signs and symptoms of Spasmodic Dysphonia - (https://www.hopkinsmedicine.org/healthlibrary/conditions/otolaryngology/spasmodic_dysphonia_85,P00468)
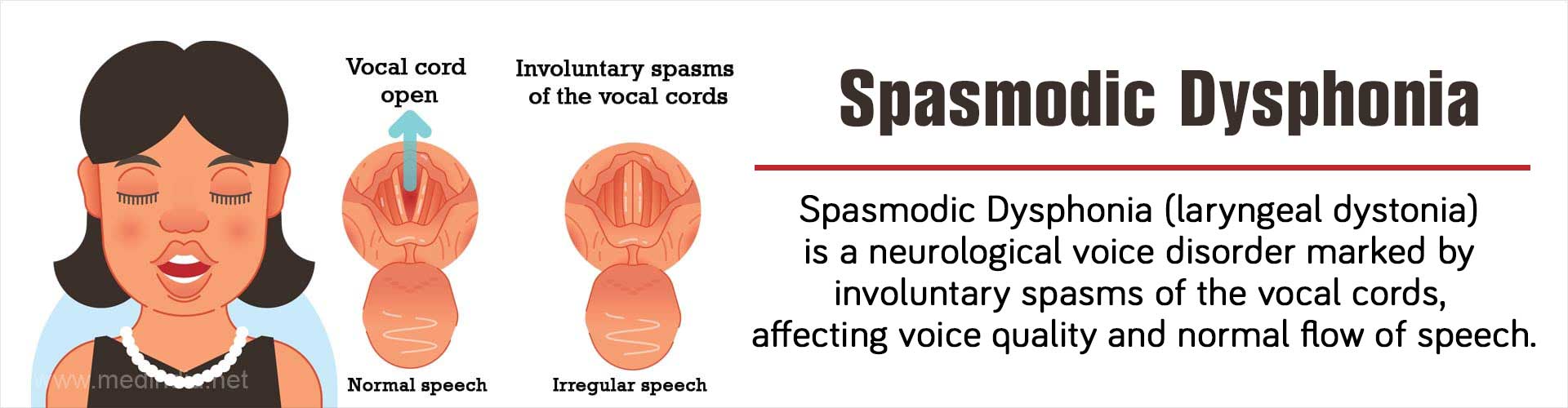
What is Spasmodic Dysphonia?
Spasmodic dysphonia [SD], also referred to as laryngeal or spastic dysphonia is a rare neurological condition, characterized by sudden involuntary spasms of the vocal cords. As a result, speech and voice quality is impacted and talking becomes an effort. The voice has a tight, strained quality and often breaks up.
A disorder that causes involuntary muscle contractions is also termed a dystonia; therefore, another name for spasmodic dysphonia is laryngeal dystonia. Spasmodic dysphonia is therefore a form of focal dystonia, a neurological condition that affects muscle tone in a localized area (focal) of the body.
The severity of spasmodic dysphonia can vary, ranging from difficulty saying a word or two to being unable to talk at all.
It is a life-long condition. It most commonly affects women, especially between the ages of 30 and 50. It is a rare condition, occurring in approximately one to four people per 100,000 people. It is estimated that about 50,000 persons suffer from this condition in North America.
It is often misdiagnosed and mistaken for other voice-related conditions.
Normal Voice or Speech Production
Normally, when we speak, air from the lungs is forced between two muscular folds, (the vocal folds or cords)—with enough pressure to cause them to vibrate, and produce sound. In spasmodic dysphonia, the muscles inside the vocal folds undergo sudden involuntary movements or spasms—which interfere with the ability of the folds to vibrate and produce sound.
What are the Types of Spasmodic Dysphonia?
There are 3 types of spasmodic dysphonia described, namely
- Adductor spasmodic dysphonia - This is the most common type. In this type, sudden involuntary spasms cause the vocal cords to stiffen and slam shut. These spasms interfere with vibration of the vocal cords and production of voice and sound. The spasms may be made worse by stress. Speaking is very strained and seems to be a great effort. Interestingly, the symptoms do not occur when singing, whispering, laughing, speaking at a high pitch, or speaking while breathing in air.
- Abductor spasmodic dysphonia – In this type, the involuntary spasms cause the vocal cords to remain open. When the vocal cords are open, vibration cannot occur, thereby making sound production more difficult. In the open position air escapes during speech, making speech quality quiet, weak and whispery. Spasms do not occur when laughing, crying or singing.
- Mixed spasmodic dysphonia – In this form, there is a combination of the above two types.
What are the Causes of Spasmodic Dysphonia?
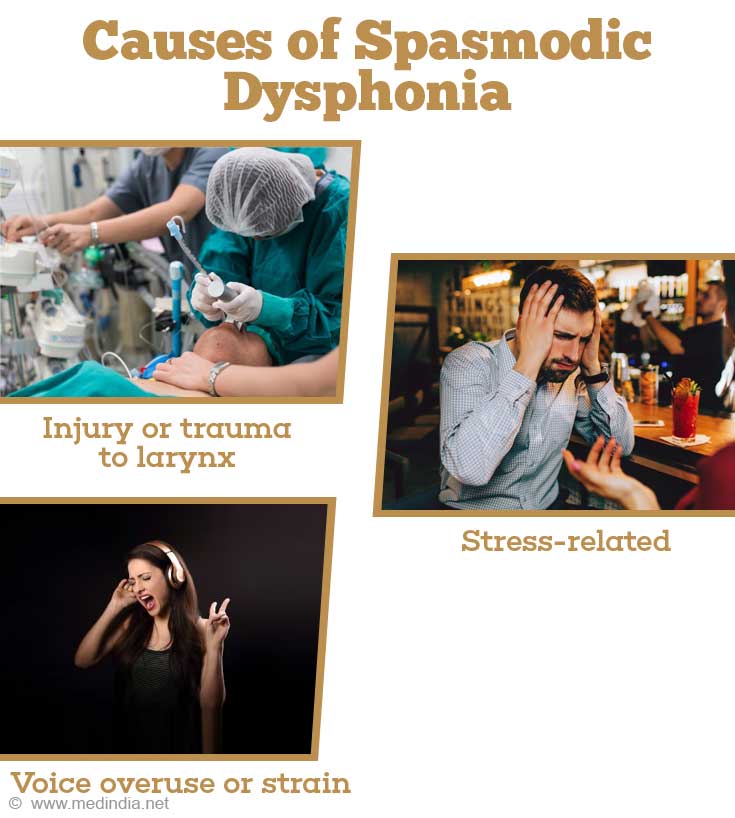
In most Spasmodic Dysphonia cases, the cause is unknown. Several theories have been proposed
- Neurological disorder – The general agreement is that SD is a neurological condition due to a defect in the basal ganglia function, the part of the brain that controls and coordinates movement.
- Trauma – In some cases, the onset is associated with injury or trauma to vocal cords
- Stress-related – Onset is related to a stressful event
- Psychogenic – Associated with underlying emotional or mental conditions
Risk Factors of Spasmodic Dysphonia
There are no obvious risk factors identified for spasmodic dysphonia. However, onset has been found to coincide with certain conditions such as
- Injury or trauma to larynx
- Stress-related
- Following an upper respiratory infection
- Voice overuse or strain
- Familial – associated with specific gene mutations causing whole body dysphonia (including spasmodic dysphonia) with onset at childhood
What are the Signs and Symptoms of Spasmodic Dysphonia?
Symptoms of spasmodic dysphonia may vary based on whether the spasms trigger the vocal cords to close or to open
- Words may be dragged out with great effort or frequently break while talking
- Hoarse quality to voice
- Whispery voice
- Strained and choked manner of speaking
Typically spasmodic dysphonia begins with mild symptoms that appear infrequently. With progression of the disease, speech becomes difficult to understand and every other word becomes punctuated by vocal cord spasm.
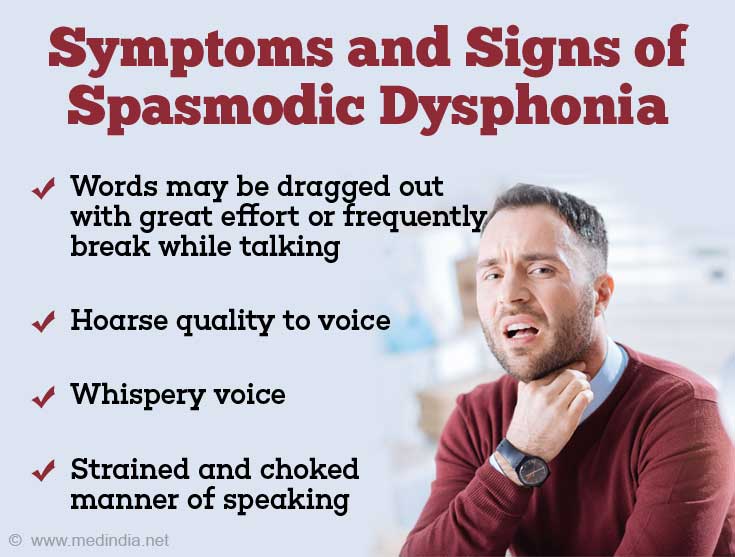
This progression typically stops within two years when the symptoms plateau.
How do you Diagnose Spasmodic Dysphonia?
Diagnosis is often difficult and the condition mimics other voice disorders. Also there is no diagnostic test to diagnose spasmodic dysphonia and diagnosis relies on the presence of clinical symptoms.
The diagnosis of spasmodic dysphonia, usually one of exclusion, and made following careful examination by a team that includes an otolaryngologist (a doctor who specializes in diseases of the ear, nose, throat, head, and neck), a speech-language therapist and a neurologist, a doctor who specializes in nervous system disorders.
The ENT specialist directly examines the vocal folds for other possible causes of the voice disorder. A small illuminated tube is passed through the nose and into the back of the throat (called fiberoptic nasolaryngoscopy) to visualize the vocal fold structure and any abnormal movement during speech and other activities.
The speech therapist assesses the voice quality and symptoms to see whether they are characteristic of spasmodic dysphonia or other voice disorders
The neurologist examines the patient for signs of other associated neurological problems and muscle movement disorders. In the presence of focal neurological signs, further imaging studies of brain including CT scan and MRI may be necessary to identify possible causes.
How is Spasmodic Dysphonia Treated?
Spasmodic dysphonia has no cure and treatment aims at alleviating the symptoms. Treatment depends on the severity of the condition, patient’s age and overall health status.
In most cases voice therapy and medical treatment is preferred as surgery to vocal cords carries risk of permanent damage
Speech therapy – Trains the person to improve muscle control and breathing correctly, which would help in talking more clearly. In addition, people may benefit from psychological counseling to help them accept their condition and cope with it
Medical treatment - Typical drugs used are benzodiazepines, anticholinergics, and dopamine antagonists but their longterm use is limited by their well-known side effects
Botulinum toxin injection - Regular injections of botulinum toxin (Botox) may be advised into the affected muscles. This is the same type of agent that is used in cosmetic treatments to give the face a more wrinkle free and youthful appearance. The toxin blocks the nerve signal to the muscle and helps prevent spasms. However, the effects of this therapy is short-lived (about 6-8 weeks)and recurrences are common necessitating repeat injections.
Augmentative and alternative devices – Certain people with spasmodic dysphonia will be able to communicate better and more easily by using devices that can amplify a person's voice in person or over the phone. Specialized software is integrated to a computer or handheld device such as a personal digital assistant (PDA) or mobile phone to convert text into synthetic speech.
Surgery – Surgery to cut one of the nerves to the vocal cords may be done in certain cases although the longterm effects are not known.
What is the Prognosis of Spasmodic Dysphonia?
Currently the standard therapy in addition to voice therapy is botulinum toxin injection. Surgery is controversial with potential adverse effects and longterm data is not readily available.
The outcome following botulinum injection is variable but side effects such as aspiration and breathy dysphonia disappear within the first week and voice improvement persists for approximately 12 weeks.
Treatment of adductor type of spasmodic dysphonia (SD) with botulinum toxin achieves better results, with an average restoration of 90% of normal voice function.
Treatment of abductor spasmodic dysphonia (SD) is slightly difficult. The abductor muscle (the PCA) is situated between the larynx and pharynx making it more difficult to inject. Most patients need bilateral PCA injections. On an average injection of botulinum toxin restores 70% of normal voice function.